 Open Journal of Respiratory Diseases, 2013, 3, 13-20 http://dx.doi.org/10.4236/ojrd.2013.31003 Published Online February 2013 (http://www.scirp.org/journal/ojrd) Bronchospasm Diagnosis in Motorcycle Taxi Drivers Exposed to Automotive Pollutants in Porto-Novo* Folly Messan1#, Mohamed Lawani2, Barnabé Akplogan2, Pierre Dansou1, Daouda Mama3, Rodrigue Hounkponou1, Rodrigue A. Dagnitché1 1Laboratory of PSA and Motricity, National Institute of Youth, Physical Education and Sport (INJEPS), University of Abomey-Calavi, Cotonou, Republic of Benin 2Laboratory of Biomechanics and Performance (LABIOP), National Institute of Youth, Physical Education and Sport (INJEPS), University of Abomey-Calavi, Cotonou, Republic of Benin 3Laboratory of Applied Hydrology, Faculty of Sciences and Technics, University of Abomey-Calavi, Cotonou, Republic of Benin Email: #messfly@yahoo.fr Received October 26, 2012; revised November 28, 2012; accepted December 5, 2012 ABSTRACT Background: In African cities, chronic exposure to pollutants is the most common public health problem faced daily by motorcycle taxi drivers. In Benin, studies conducted on motorcycle drivers, have shown the presence of nitrogen oxides, carbon monoxide, sulfur dioxide, volatile organic compounds and particulate matter in ambient air, which may affect lung function. Aims: This study aims to diagnose potential respiratory problems among 48 motorcycle taxi dri- vers (47.02 ± 8.75 years) compared to a control group made up of 52 people (46.38 ± 8.81 years) in Porto-Novo, Benin. Methods: A questionnaire, two exploration pulmonary function tests and two 6-minute walk tests were used to identify symptoms and changes in respiratory variables that reveal the existence of bronchospasm. Results: The frequency of respiratory symptoms noted among motorcycle taxi drivers is higher than that recorded among members of the control group. We observed that motorcycle drivers at rest and after physical effort have significantly lower respiratory vari- ables (FVC, FEV1, PEF, FEF25-75, FEF50 and FEF25) (p < 0.05) than those recoded in control group. Conclusion: It can therefore be concluded that, because of the relatively long duration of exposure among motorcycle taxi drivers, the in- halation of automobile pollutants, may cause respiratory problems in this population. Keywords: Automobile Pollution; Asthma; Bronchospasm; Urban Pollution; Motorcycle-Taxi Drivers; Benin 1. Introduction The socioeconomic status of West African countries has not improved despite the implementation of the Millen- nium Development Objectives in 2000, which aim to reduce extreme poverty and hunger, improve health and ensure environmental sustainability by 2015. With less than five years left to meet these goals, it is clear that problems still remain, including relatively low rates of children enrolled in school, high poverty rates and high levels of environmental pollution generated by urban transport in African capital cities. Indeed, urban popula- tion growth, migration of young people from villages to cities, massive layoffs of civil servants resulting from the structural adjustment programs imposed by the Bretton Woods Institutions in the 1980s and the devaluation of the currency of the African Financial Community (CFA) in 1994, have resulted in a high rate of unemployment in West African countries in general and in Benin in par- ticular. This crisis is most acutely felt in Benin’s major cities, such as Cotonou and Porto-Novo where low in- comes and the lack of transportation policy governing urban public transportation have given rise to informal transportation activity led by motorcycle taxi drivers. These motorcycles imported from Europe are locally called “Zémidjan” and 95% of them have used engines that emit thick black smoke into the atmosphere, particu- larly at intersections during peak traffic hours. The fumes are generated by incomplete combustion of hydrocarbons and other particles due to mechanical failures of the automobiles poorly maintained motors and the poor quality of fuel illegally imported from neighboring, Ni- geria. These motorcycles contribute to the degradation and pollution of the environment, causing health prob- lems among the general population and among profess- sional motorcycle taxi drivers in particular. A study con- ducted on samples of urine and blood collected from motorcycle taxi drivers in Cotonou showed high levels of benzene and ultrafine particles which are likely to dam- age the deoxyribonucleic acid (DNA) [1-3]. Another *The authors declare no conflict of interest. #Corresponding author. C opyright © 2013 SciRes. OJRD 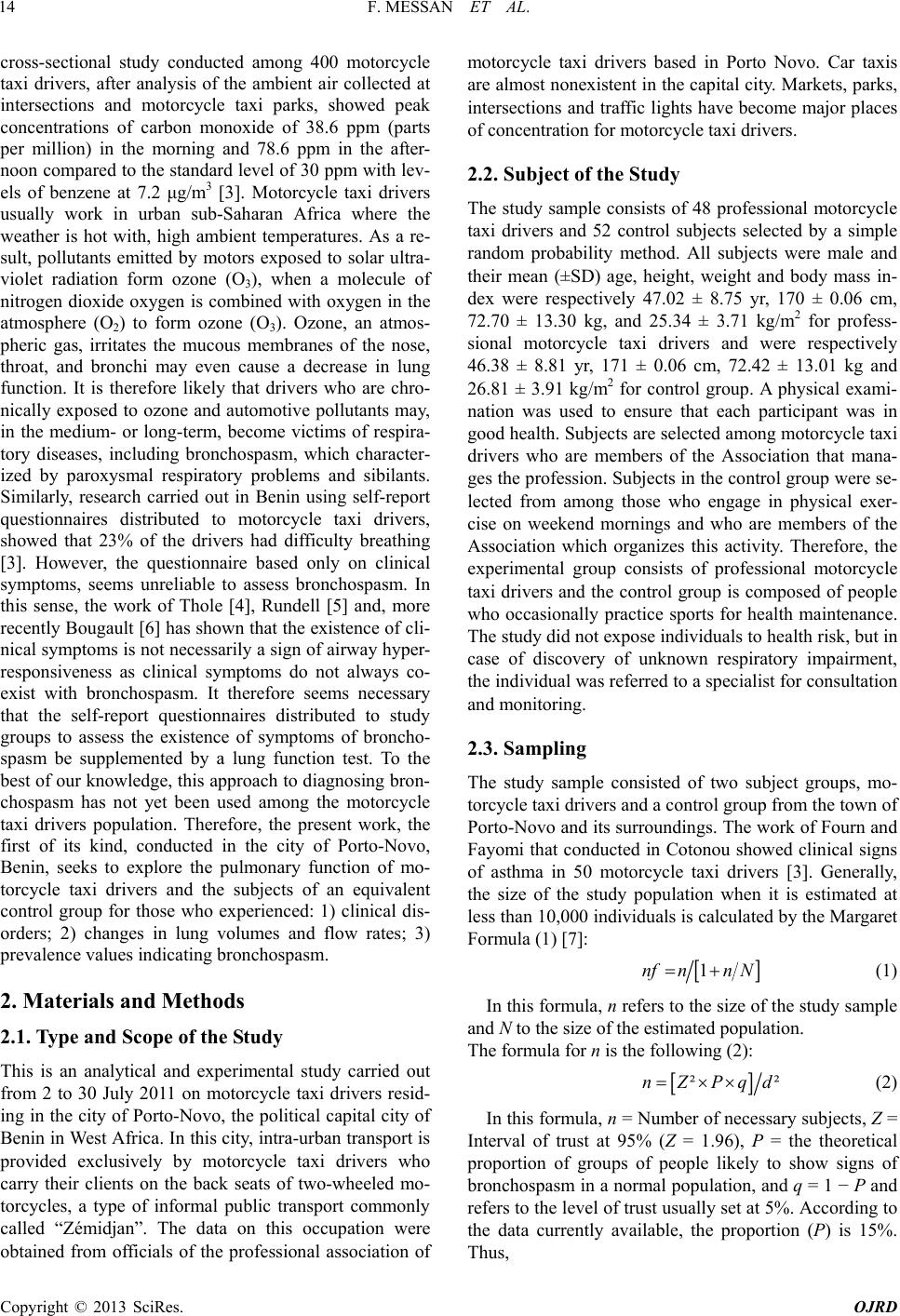 F. MESSAN ET AL. 14 cross-sectional study conducted among 400 motorcycle taxi drivers, after analysis of the ambient air collected at intersections and motorcycle taxi parks, showed peak concentrations of carbon monoxide of 38.6 ppm (parts per million) in the morning and 78.6 ppm in the after- noon compared to the standard level of 30 ppm with lev- els of benzene at 7.2 μg/m3 [3]. Motorcycle taxi drivers usually work in urban sub-Saharan Africa where the weather is hot with, high ambient temperatures. As a re- sult, pollutants emitted by motors exposed to solar ultra- violet radiation form ozone (O3), when a molecule of nitrogen dioxide oxygen is combined with oxygen in the atmosphere (O2) to form ozone (O3). Ozone, an atmos- pheric gas, irritates the mucous membranes of the nose, throat, and bronchi may even cause a decrease in lung function. It is therefore likely that drivers who are chro- nically exposed to ozone and automotive pollutants may, in the medium- or long-term, become victims of respira- tory diseases, including bronchospasm, which character- ized by paroxysmal respiratory problems and sibilants. Similarly, research carried out in Benin using self-report questionnaires distributed to motorcycle taxi drivers, showed that 23% of the drivers had difficulty breathing [3]. However, the questionnaire based only on clinical symptoms, seems unreliable to assess bronchospasm. In this sense, the work of Thole [4], Rundell [5] and, more recently Bougault [6] has shown that the existence of cli- nical symptoms is not necessarily a sign of airway hyper- responsiveness as clinical symptoms do not always co- exist with bronchospasm. It therefore seems necessary that the self-report questionnaires distributed to study groups to assess the existence of symptoms of broncho- spasm be supplemented by a lung function test. To the best of our knowledge, this approach to diagnosing bron- chospasm has not yet been used among the motorcycle taxi drivers population. Therefore, the present work, the first of its kind, conducted in the city of Porto-Novo, Benin, seeks to explore the pulmonary function of mo- torcycle taxi drivers and the subjects of an equivalent control group for those who experienced: 1) clinical dis- orders; 2) changes in lung volumes and flow rates; 3) prevalence values indicating bronchospasm. 2. Materials and Methods 2.1. Type and Scope of the Study This is an analytical and experimental study carried out from 2 to 30 July 2011 on motorcycle taxi drivers resid- ing in the city of Porto-Novo, the political capital city of Benin in West Africa. In this city, intra-urban transport is provided exclusively by motorcycle taxi drivers who carry their clients on the back seats of two-wheeled mo- torcycles, a type of informal public transport commonly called “Zémidjan”. The data on this occupation were obtained from officials of the professional association of motorcycle taxi drivers based in Porto Novo. Car taxis are almost nonexistent in the capital city. Markets, parks, intersections and traffic lights have become major places of concentration for motorcycle taxi drivers. 2.2. Subject of the Study The study sample consists of 48 professional motorcycle taxi drivers and 52 control subjects selected by a simple random probability method. All subjects were male and their mean (±SD) age, height, weight and body mass in- dex were respectively 47.02 ± 8.75 yr, 170 ± 0.06 cm, 72.70 ± 13.30 kg, and 25.34 ± 3.71 kg/m2 for profess- sional motorcycle taxi drivers and were respectively 46.38 ± 8.81 yr, 171 ± 0.06 cm, 72.42 ± 13.01 kg and 26.81 ± 3.91 kg/m2 for control group. A physical exami- nation was used to ensure that each participant was in good health. Subjects are selected among motorcycle taxi drivers who are members of the Association that mana- ges the profession. Subjects in the control group were se- lected from among those who engage in physical exer- cise on weekend mornings and who are members of the Association which organizes this activity. Therefore, the experimental group consists of professional motorcycle taxi drivers and the control group is composed of people who occasionally practice sports for health maintenance. The study did not expose individuals to health risk, but in case of discovery of unknown respiratory impairment, the individual was referred to a specialist for consultation and monitoring. 2.3. Sampling The study sample consisted of two subject groups, mo- torcycle taxi drivers and a control group from the town of Porto-Novo and its surroundings. The work of Fourn and Fayomi that conducted in Cotonou showed clinical signs of asthma in 50 motorcycle taxi drivers [3]. Generally, the size of the study population when it is estimated at less than 10,000 individuals is calculated by the Margaret Formula (1) [7]: 1nfnn N (1) In this formula, n refers to the size of the study sample and N to the size of the estimated population. The formula for n is the following (2): ²nZPqd ² (2) In this formula, n = Number of necessary subjects, Z = Interval of trust at 95% (Z = 1.96), P = the theoretical proportion of groups of people likely to show signs of bronchospasm in a normal population, and q = 1 − P and refers to the level of trust usually set at 5%. According to the data currently available, the proportion (P) is 15%. Thus, Copyright © 2013 SciRes. OJRD  F. MESSAN ET AL. 15 2 1.960.15 0.850.05n 2 (3) then, 1961196 250nf (4) Thus, according to this formula (3), the total sample size should be at least 100 individuals. 2.4. Selection Criteria 2.4.1. Inclusion Criteria Individuals meeting the following criteria are included in the study: 1) male; 2) from the Department of Oueme; 3) at least 30 years old and a resident of Porto-Novo; 4) provision of the signed informed consent form to parti- cipate in the study; 5) own a private motorcycle; 6) hold- ing a membership card of the association of sports practi- tioners or of motorcycle taxi drivers for at least five years, and 7) having at least five years of experience as motor- cycle drivers in Porto-Novo. 2.4.2. Exclusion Criteria Individuals meeting the following criteria are not includ- ed in the study 1) being a victim of myocardial infarction during the previous month; 2) having a resting heart rate greater than or equal to 120 bpm; 3) being a cigarette smoker 4) suffering from asthma or tuberculosis; 5) hav- ing a clinical history of rheumatism or orthopedic symp- toms that obstruct the completion of a 6-minute walk test; 6) conducting imperfect maneuvers during respiratory exploration tests; 7) practicing intense sports activities in addition to motorcycle riding, or 8) refusing to sign the informed consent form. 2.4.3. Materia l s and Techniques Both groups were questioned using a respiratory ques- tionnaire based on that used by the American Thoracic Society (ATS), and also including questions about previ- ously established clinical disorders (e.g., headache and/ or insomnia, conjunctival hyperemia and breathing dis- orders) [8]. The closed-answer questions most often had dichotomous responses and were translated into the local language goun when necessary. Fact sheets were used to collect information from members of both groups, on age, history of diseases and monthly frequencies of motorcy- cle taxi use. A SECA brand human weighing machine, accurate to approximately 500 g with a maximum range of 150 kg, used to determine the body weight of each subject. A wall gauge measuring from zero to two meters was used to measure the height of the subjects standing barefoot and upright, with the head positioned in the ho- rizontal plane of Frankfort [9]. The body mass index (BMI = weight on the square of height (kg·m−2)) was calculated. A trail of 30 linear meters delineated by studs placed at each distance of one meter was used to conduct the 6-minute walk tests (6-MWT) as recommended by the ATS [8]. A double decameter calibrated in centime- ters with a digital display and a Run Tech measuring tape stopwatch, accurate to one hundredth of a second, were used to measure the length of the track and the duration of walking tests. A Run Tech heart rate monitor model 20,488 was used to record the individuals’ heart rates at rest and after physical exercise. Mouthpieces and dis- posable antibacterial filters (Cosmed Ltd., Rome, Italy) were used to avoid cross contamination between patients. Pulmonary function tests were performed using the Mi- cro quark spirometer (Cosmed Ltd, Rome, Italy). At the beginning of each day of operation, the spirometer is ca- librated using a calibration syringe (Cosmed Ltd, Rome, Italy) with a capacity of 3 liters of atmospheric air. In the evaluation of the individuals’ pulmonary function, the Micro Spirometer Quark displays the flow volume curve in real-time on the monitor. The flow emitted varies from 0.03 to 20 L/s and with maximum volume of 10 L, with an accuracy of plus or minus 3%, as recommended by the European Respiratory Society [10] and the American Tho- racic Society [8]. The Micro Quark equipped with a tur- bine vane sensor works as follows: a light is flashed and is continuously recorded by a photoelectric cell. The ro- tating impeller with vanes blocks the light path and chan- ges the electrical collection, depending on the speed of movements induced by the volume of air exhaled by the individual. The interruption of the beam depends on the speed of the air passing through the initial deflector. The electrical impulses are recorded by a tachometer. 2.4.4. Experimental Protocol 2.4.4.1. Experimentation Plan In the first phase of experimentation, the motorcycle taxi drivers and the selected members of the control group filled out the individual information sheets and informed consent forms. The BMI and height of the individuals were measured. In the second phase, the subject, sitting in a chair, observes15 minutes of passive rest after which the following measurements are taken: heart rate while sitting, lung volumes and flow rates while standing. After a 10 minutes passive break, the subject performs the first 6-minute walk test (6-MWT1) followed by 10 minutes of rest, then a second walk test (6-MWT2). At the end of the 6-MWT2, the heart rate is immediately measured while the measurement of respiratory variables is performed after a 10-minute break. 2.4.4.2. Pulmonary Function Tests The pulmonary function tests (PFT) were performed un- der the supervision of a medical technician. After deter- mining the size, body weight, age, sex and race of the in- dividual, the spirometer unit automatically calculates the Copyright © 2013 SciRes. OJRD  F. MESSAN ET AL. 16 theoretical values of each respiratory parameter. In the PFT, the individual, while standing with nose pinched and a turbine between their two hands breathed naturally and quietly through the mouthpiece connected to the spi- rometer. The individual was then instructed to inflate his lungs, and then breathe the air as quickly as possible, in a continuous and complete way. After the test, the best test was selected among the three reproducible tests that have been validated according to the algorithms of the spiro- meter. The lung volumes and peak flows were recorded. 2.4.4.3. Six-Minute Walk Test (6-MWT) This test was carried out according to the protocol sug- gested by the ATS [8]. Subjects are asked to keep a run- ning speed as regular as possible and travel the greatest distance possible in six minutes, running back and forth between two 30-meter markers. All individuals perfor- med the 6-MWT without encouragement and under the supervision of three sports instructors. Because of possi- ble influences that may induce biorhythms that impact performance, all six-minute walk tests were conducted in the morning between 7:30 and 9:30 am, and food intake was not allowed before or during that time-frame. The Intensive Care Unit of Porto Novo Central Hospital was informed of the experiment to prepare for any eventuality. This study was approved by the Scientific Committee of Science and the Technology Sector of the Sports and Phy- sical Activities Department (CSS/sport science), Abomey- Calavi University, in accordance with the Helsinki Act of 1975 on ethics. 2.4.5. Variables S tudied 2.4.5.1. Variables Measured at Rest before the 6-MWT The forced vital capacity (FVC), the forced expiratory volume in one second (FEV1), the peak expiratory flow (PEF), the forced expiratory flow from 25% - 75% of the vital capacity (FEF25-75), the forced expiratory flow from 50% of the vital capacity (FEF50) and the forced expira- tory flow from 25% of the vital capacity (FEF25) ob- tained from respiratory exploration are used as respira- tory variables. The theoretical maximum heart rate (pre- dicted HRmax) equal to the individual’s age subtracted from 220 (220-age), was observed while all subjects were at rest. These variables, noted for both groups of indi- viduals prior to completion of 6-MWT1, were considered to be resting values. Comparison of respiratory variables of the group of motorcycle taxi drivers with those of the control group was used to assess the risk from inhalation of exhaust gases from vehicles. 2.4.5.2. Variables Measured after the 6-MWT The maximum heart rates (HRmax) noted at the end of 6-MWT were expressed as percentage change compared to the predicted HRmax, as assessed at the end of the ex- periment, in addition to the level of intensity of the exer- cise test reached by the subjects. These parameters were calculated using the following formula. max maxmax HR%HR100Predicted HR (5) The best variables recorded at the end of 6-MWT were considered post-exercise values. At the end of 6-MWT, the six-minute walking distance (6-MWD) was calcu- lated following formula. 6-MWD m Number of round trips60 mfinal meters (6) At the end of 6-MWT, the comparison of respiratory variables in the experimental group with the control group was used to evaluate the variation of these para- meters. The diagnosis of bronchospasm was said to be positive in a subject if his post-FEV dropped at least 10% compared with the value at rest as calculated using the formula. FEV % FEV post exercise100FEV pre exercise100 total riding time of 8 hours minimum and 12 hours maxi- (7) 2.4.6. Statistical Analysis The variables were processed using StatView 5 software (version 5) (Abacus Concepts Inc. Berkeley, CA, USA). Descriptive statistics were generated for each variable. The normal distribution of variables, as well as the equi- valence of their respective variances, was checked by the Kolmogorov-Smirnov test and the F-test. Comparisons between groups were performed by unpaired t-tests after the normality of the distribution and homogeneity of va- riances were verified. For all statistical analyses, the null hypothesis was rejected at a probability of P < 0.05. 3. Results Table 1 shows the comparison of biometric parameters and distances between motorcycle taxi drivers and me- mbers of control group. The differences were not signifi- cant (p > 0.05). In contrast, the percentage of predicted HRmax of motorcycle taxi drivers was significantly (p < 0.001) lower than the control group (Table 1). Symptoms recorded during the self-reported questionnaires among motorcycle taxis drivers, were related to clinical disor- ders (headache and/or insomnia) in 30% of cases, con- junctival hyperemia (25%), digestive disorders such as nausea and vomiting (26%), and respiratory disorders and persistent bronchorrhea (20%). In the control group, the same disorders were noted with lower frequencies: headache (18.5%), conjunctival hyperemia (13%), and headache (16%). The included motorcycle drivers had a Copyright © 2013 SciRes. OJRD  F. MESSAN ET AL. 17 Table 1. Comparisons of biometric, distances traveled and heart rates betw een motorcycle taxi drivers group and con- trol group. Parameters Motorcycle taxi dri 8) Control Group (n = 52) vers Group (n = 4 Mean ± SD Mean ± SD Age ears) 7 7 6 6 H (y47.02 ± 8.75 46.38 ± 8.81 Height (m) 1.70 ± 0.06 1.71 ± 0.06 Weight (kg) 2.70 ± 13.30 2.42 ± 13.01 BMI (kg·m−2) 25.34 ± 3.71 26.81 ± 3.91 6-MWD (m) 15.63 ± 65.15 37.05 ± 79.88 Rmax (%) Pred52.36 ± 9.80*** 66.00 ± 9.58 SDn; HRteax; Pred:WD: um per day whereas the control subjects were exposed at, at re ts were noted after the physical exercise of 4. Discussion tudy was to test lung function and to y Motorcycle taxi dri8) Control Group (n = 52) : Standard deviatiomax: Heart Ra m Predicted; 6-M 6-Minute Walking Distance; BMI: Body Mass Index; ***p < 0.001 m to pollution in traffic for one to two hours per day. Among motorcycle taxi drivers, Table 2 shows th st and before physical exercise, respiratory variables were significantly (p < 0.01) lower than those of the con- trol group. The same resul 6MWT (Table 3). A drop of at least 10% in FEV post exercise was observed in 15 motorcycle taxi drivers out of a total of 48, with an average drop in FEV by 19.17% (10.04% 37.04%), which is a prevalence of bronchospa- sm of 31.07%. In the control group, this criterion was found in 12 subjects out of a total of 52, with an average drop of 17.36% in FEV (10.08% 37.41%), which is a prevalence of 23.07%. The aim of this s determine the prevalence of bronchospasm among mo- torcycle taxi drivers working in urban areas of Porto- Novo. Cross-sectional studies previously conducted in Benin showed that in urban environments where informal public transport activities are carried out, the environ- ment is highly polluted [1-3]. Indeed, urban pollution is the result of pollutants emissions from various sources, including traffic and industrial activities within cities. The most prevalent pollutants generated from road transport are nitrogen oxides (NO and NO2), carbon monoxide (CO), sulfur dioxide (SO2), volatile organic compounds and par- ticulate matter [11]. In addition, ozone is a common pol- lutant formed by a photochemical reaction, resulting from the sufficient duration of sunlight in Porto-Novo at high ambient temperatures. Similarly, some particles are emitted directly or formed by reaction between gases and particles. The analysis of ambient air in these cities of Benin reveals a concentration of carbon monoxide rang- Table 2. Comparisons of respiratory variables between Motorcycle taxi drivers group and Control group before 6-MWT. Respirator variables vers Group (n = 4 Mean ± SD Mean ± SD FVC (L) F ) 2.97 ± 0.68** 3.43 ± 0.67 FEV1 (L) 2.00 ± 0.55** 2.42 ± 0.49 PEF (L·s−1) 2.82 ± 1.04** 3.84 ± 1.47 EF25-75 (L·s−1)1.76 ± 0.62*** 2.33 ± 0.66 FEF50 (L·s−1 2.06 ± 0.73** 2.69 ± 0.87 FEF25 (L·s−1) 1.02 ± 0.39** 1.35 ± 0.45 SDation; FVcapacity; FE- able 3. Comparisons of respiratory variables between Mo- iratory Motorcycle taxi dri 8) Control Group : Standard deviC: forced vital V1: forced expira tory volume in one second; PEF: peak expiratory flow; FEF25-75: expiratory flow from 25% - 75% of the vital capacity; FEF25, FEF50: instantaneous expiratory flows at 25% and 50% respectively; **p < 0.01; ***p < 0.001. T torcycle taxi drivers group and Control group after 6- MWT. Resp variables vers Group (n = 4(n = 52) Mean ± SD M ean ± SD FVC (L) F 50 ) 3.06 ± 0.70** 3.45 ± 0.66 FEV1 (L) 1.95 ± 0.54*** 2.46 ± 0.48 PEF (L·s−1) 2.66 ± 0.92*** 3.89 ± 1.63 EF25-75 (L·s−1)1.71 ± 0.60*** 2.28 ± 0.72 FEF (L·s−12.03 ± 0.72** 2.61 ± 1.01 FEF25 (L·s−1) 0.98 ± 0.40** 1.30 ± 0.41 SD:tion; FVCapacity; FE- g between 26 to 38.6 ppm in the morning and 58 to 78.6 Standard devia: forced vital cV1: forced expira tory volume in one second; PEF: peak expiratory flow; FEF25-75: expiratory flow from 25% - 75% of the vital capacity; FEF25, FEF50: instantaneous expiratory flows at 25% and 50% respectively; **p < 0.01; ***p < 0.001. in ppm in the afternoon against a 30 ppm [3]. Likewise, ben- zene was identified with an average value of 7.2 µg/m3. On the basis of a self-report questionnaire that reveals respiratory disorders in the motorcycle taxi drivers, this study suggest that this bronchopulmonary infection could be caused by automobile pollution. To assess possible influences of the ambient polluted air on the lung func- tion of motorcycle taxi drivers and control group residing in Porto-Novo, respiratory variables were carefully mea- sured in the resting state during pulmonary function test- ing. In addition, the individuals were subjected to a stress test because the bronchospasm is recognized as being a latent respiratory disease. The physical characteristics of individuals such as height, body mass and age, that may affect the respiratory variables were compared between Copyright © 2013 SciRes. OJRD  F. MESSAN ET AL. 18 the group of motorcycle taxi drivers and the control group. These comparisons showed no significant diffe- rence between the two groups (p > 0.05), thereby ensur- ing their comparability for the purposes of this study. Variables observed in motorcycle taxi drivers were as- sessed with reference to the control group. The main re- sults noted in this study were as follows: 1) the frequen- cies of symptoms observed among motorcycle taxi driv- ers are higher than those recorded in the control group; 2) the motorcycle taxi drivers experienced, at rest and after exercise testing, peak flow volumes and lung capacity that were significantly lower (p < 0.01) than in the indi- viduals of the control group and; 3) the group of motor- cycle taxi drivers presented a prevalence of 31.25% of bronchospasm, which exceeds the 8.18% prevalence pre- sented in the control group. However, proportions in the control group did not differ significantly (p > 0.05). The high frequency of symptoms, respiratory depression va- riables and high values of prevalence of bronchospasm observed in motorcycle taxi drivers compared to the con- trol group may be due to exhaust gas poisoning. Indeed, inhalation of oxidants such as NO2 generated by road tra- ffic can degrade cell membranes constituents through the toxic peroxides [12]. Experimental studies conducted on animals show a reactivity of NO2 with the airway epithe- lium and thickening of small airways, accompanied by a proliferation of connective tissue around the bronchus [13]. Another study on rats showed a decrease in to the cilia of respiratory epithelia that play an essential role in removing particles reaching the bronchi and bronchioles [14]. Moreover, the toxic effects induced by NO2 gener- ally observed on the respiratory mucosa, may range from irritation to asthma attacks, following a bronchial reac- tivity with cough [15]. An irritating effect on the ocular membranes mucous (conjunctiva) and a decreased resis- tance to pathogens were also noted [16]. SO2, a very so- luble irritant, also acts synergistically with other sub- stances, including particulate matter. The SO2 inhaled is retained by the watery surfaces of the nose and upper respiratory tract thereby causing eye irritation, skin and respiratory infection. Exposure to SO2 increases the inci- dence of chronic bronchitis and pharyngitis. Indeed, epi- demiological studies show that exposure to sulfur dioxide (SO2) at a concentration of approximately 1000 µg/m3 may cause or exacerbate latent respiratory infections and result in increased mortality caused by respiratory or car- diovascular disease [17]. Similarly, the work of Bruske- Hohlfeld [18] showed that an increased level of air pollu- tion consisting of fine particles, especially from vehicle emissions, may lead to respiratory problems. In addition, the high production of particles, carbon monoxide (CO), lies in the anoxia-induced conversion of hemoglobin to car- boxyhemoglobin while that of nitrogen dioxide (NO2) and suspended ultrafine particles are involved in airway dysfunction [19-21]. From the measurement of lung fun- ction performed on children living in Los Angeles [22] and China [23], the effect of ozone on respiratory vari- ables has been highlighted. Indeed, some respiratory pa- rameters such as FEV1, FEF25-75 and FVC were ob- served to decrease over a period of monitoring from 1984 to 1987 [22]. Our results confirm those of Cakmak [24], which conclude that chronic exposure to high concentra- tions of polluted air causes a reduction in lung function. Under these conditions, how can we explain differences in the frequency of symptoms, respiratory variables and values of bronchospasm prevalence noted among motor- cycle taxi drivers and the control group? As part of their profession, the motorcycle taxi drivers are exposed daily to automotive pollutants for 8 hours minimum and some- times as many as 10 to 12 hours, compared with control subjects who are exposed to automotive pollutants one to two hours per day because of their daily activities. Be- cause individuals in both groups were not subjected to the same level and duration of exposure to automotive pollutants, it can be assumed that this fact can explain the differences noted in frequency of symptoms, as well as differences in recorded ventilatory parameters observed at rest. Indeed, motorcycle taxi drivers at rest showed a significant reduction in lung function compared with the control group (Tab le 2 ). The diagnosis of lung function sometimes requires the use of exercise testing which may reveal latent or overt bronchospasm. Indeed, during phy- sical exercise, the airways are exposed to progressively hyper osmolarity. This dehydrating mechanism leads to an increase in the concentrations of Ca2+, K+, Cl− and Na+. As a result, the inflammatory mediators are released and induce airway contraction [25,26]. As part of the study and after the 6-minute walk test, motorcycle taxi drivers showed respiratory variables significantly lower than those noted in individuals of the control group (Table 3). Can physical exercise, with its implications in the occur- rence of bronchospasm, explain the observed differences in respiratory variables? The change in respiratory pa- rameters noted at the end of the 6-minute walk test has several explanations. In fact, the 6-minute walk test is a sub maximal exercise, classically tailored to elderly pa- tients, as recommended by the ATS [8]. The heart rates observed after the exercise test confirm that the 6-minute walk test is actually sub maximal because they corre- spond to 52.36% and 66% of predicted HRmax in motor- cycle taxi drivers and the control group respectively. In addition, variables observed at rest and after physical exercise did not differ significantly between the two groups. Motorcycle taxi drivers seem to be more physi- cally fit and able than the control group because at the end of the effort, the average HRmax recorded among motorcycle taxi drivers (52.36 ± 9.80%) is significantly (p < 0.01) lower than that of control subjects (66% ± Copyright © 2013 SciRes. OJRD  F. MESSAN ET AL. 19 9.58%). The fact remains, however, that the comparison of the distances traveled by the two groups was not sig- nificantly different (p > 0.05) (Table 1). Furthermore, the fact that motorcycle taxis drivers ventilate polluted air for many hours and the corresponding risk of contact between the bronchial mucosa and allergens in the air could increase their sensitivity [27,28]. Indeed, in the event of a hypersensitivity to these allergens, the IgE-de- pendent mechanism would become active, stimulate mast cell membrane and facilitate the penetration of calcium into the cell nucleus. Under these conditions, the mast cells would degranulate the inflammatory mediators which may also induce contraction of smooth muscles of the airways. The findings of previous studies, in the studies [29,30] also point to a link between exposure to gases emitted by traffic and respiratory infection, including bronchospasm. Therefore, the quality of ambient air in- haled at rest as well as during physical exercise appears to be a key factor that can lead to bronchospasm, the pre- valence of which can be determined from comparing FEV at rest and after exerting effort. The prevalence of bronchospasm observed in the control group (23.07%) is higher than that reported in the general population which ranges from 4% to 20% [31-33]. In addition, at the end of the 6-MWT, the prevalence of bronchospasm among mo- torcycle taxi drivers (31.25%) is higher than that obser- ved among basketball players in Benin (26%) [34]. Chro- nic exposure of the general population and of the motor- cycle taxi drivers to traffic pollution has emerged as a pu- blic health problem whose consequences still raise health concerns. Thus, studies showing links between exposure to pollution from nearby urban areas and respiratory di- seases are not unanimous in their findings. Therefore, the knowledge of environmental conditions and their impact on human health require an interdisciplinary approach. 5. Conclusion ies previously conducted in Benin on 6. Acknowledgements professional motorcycle REFERENCES [1] P. H. Avogbe,p, et al., “Ultrafine Cross-sectional stud motorcycle taxi drivers have shown high levels of auto pollutants. These pollutants consist of nitrogen oxides (NO and NO2), carbon monoxide, benzene and volatile organic compounds that influence the well-being and, respiratory health of individuals. For this reason, the present study investigated the lung function of motorcy- cle taxi drivers, individuals with high exposure to auto- motive pollutants to diagnose overt or latent respiratory infection. The results of the study show that motorcycle taxi drivers, both at rest and after exercise, experience high frequencies of asthma symptoms, significant reduc- tions in lung volumes and flow rates and high prevalence of bronchospasm. These results clearly show the exis- tence of respiratory disorders due to chronic exposure to automotive pollutants. The results should enable city counselors of Porto-Novo, to better understand the respi- ratory hazards that motorcycle taxi drivers face every day. To mitigate the harmful effects of pollutants, gasoline vehicles that do not have catalytic converters and diesel cars without particulate filters should be banned. Finally, the study raises awareness about the exposure risks and suggests preventive measures to preserve the health of motorcycle taxi drivers. Measures including, regular in- spections of imported used vehicles, the reduction of exhaust gas, the strengthening of the law on atmospheric environment protection and proper management of cross- roads, can reduce the production of automotive pollutants in the city of Porto-Novo, Benin. The authors would like to thank taxi drivers and subjects in the control group for their participation in the study and field and laboratory staff that collected the data. L. Ayi-Fanou, H. Autru Particulate Matter and High-Level Benzene Urban Air Pollution in Relation to Oxidative DNA Damage,” Car- cinogenesis, Vol. 26, No. 3, 2005, pp. 613-620. doi:10.1093/carcin/bgh353 [2] L. Ayi-Fanou, P. H. Avogbe, B. Fayomi, et al., “DNA- Adducts in Subjects Exposed to Urban Air Pollution by Benzene and Polycyclic Aromatic Hydrocarbons (PAHs) in Cotonou, Benin,” Environmental Toxicology, Vol. 26, No. 1, 2011, pp. 93-102. doi:10.1002/tox.20533 [3] L. Fourn and E. B. Fayomi, “Air Pollution in Urban Area - in Cotonou and Lokossa, Benin,” Bulletin de la Société de Pathologie Exotique, Vol. 99, No. 4, 2006, pp. 264-268. [4] R. T. Thole, R. E. Sallis, A. L. Rubin, et al., “Exercise Induced Bronchospasm Prevalence in Collegiate Cross- Country Runners,” Medicine and Science in Sports and Exercise, Vol. 33, No. 10, 2001, pp. 1641-1646. doi:10.1097/00005768-200110000-00005 [5] K. W. Rundell, J. Im, L. B. Mayers, et al., “Self-Reported 00-00006 Symptoms and Exercise-Induced Asthma in the Elite Ath- lete,” Medicine and Science in Sports and Exercise, Vol. 33, No. 2, 2001, pp. 208-213. doi:10.1097/00005768-2001020 let, “Bronchial [6] V. Bougault, J. Turmel and L. P. Bou Challenges and Respiratory Symptoms in Elite Swimmers and Winter Sport Athletes: Airway Hyperresponsiveness in Asthma: Its Measurement and Clinical Significance,” Chest, Vol. 138, No. 2, 2010, pp. 31S-37S. doi:10.1378/chest.09-1689 [7] O. A. Margaret, “Research Methodology with Statistics racic Society, “Standardization of Spiro- for Health and Social Sciences,” Nathadex Publishers, Ilorin, 2003. [8] American Tho metry: 1994 Update,” American Journal Respiratory Cri- tical Care and Medicine, Vol.152, No. 3, 1995, pp. 1107- 1136. Copyright © 2013 SciRes. OJRD  F. MESSAN ET AL. Copyright © 2013 SciRes. OJRD 20 ic Standardization Reference Manual,” Human Ki- ropean Respira- ironment: Within-Urban Variab [9] T. G. Lohman, A. F. Roche and R. Martorell, “Anthro- pometr netics Books, Champaign, 1998. [10] European Respiratory Society, “Standardized Lung Func- tion Testing. Official Statement of the Eu tory Society,” European Respiratory Journal, Vol. 6, 1993, pp. 53-83. [11] S. Hankey, J. D. Marshall and M. Brauer, “Health Im- pacts of the Built Envility in Physical Inactivity, Air Pollution and Ischemic Heart Disease Mortality,” Environmental Health Perspectives, Vol. 120, No. 2, 2012, pp. 247-253. doi:10.1289/ehp.1103806 [12] J. D. Crapo, B. E. Barry, L. Y. Chang in Lung Structure Caused , et al., “Altera by Inhalation of Oxidants,” tions Journal of Toxicology and Environmental Health, Vol. 13, No. 2-3, 1984, pp. 301-321. doi:10.1080/15287398409530500 [13] L. E. Fujinaka, D. M. Hyde, piratory Bronchiolitis Following L C. G. Plopper, et al., “ ong-Term Ozone Ex- Res- posure in Bonnet Monkeys: A Morphometric Study,” Ex- perimental Lung Research, Vol. 8, No. 2-3, 1985, pp. 167-190. doi:10.3109/01902148509057520 [14] B. E. Barry, R. R. Mercer, F. J. Miller, et al., “Effects of Inhalation of 0.25 ppm Ozone on the Terminal Bronchi- oles of Juvenile and Adult Rats,” Experimental Lung Re- search, Vol. 14, No. 2, 1988, pp. 225-245. doi:10.3109/01902148809115126 [15] C. Pénard-Morand, C. Raherison, D. Cha “Long-Term Exposure to Close-P rpin, et al. roximity Air Pollution , and Asthma and Allergies in Urban Children,” European Respiratory Journal, Vol. 36, No. 1, 2010, pp. 33-40. doi:10.1183/09031936.00116109 [16] B. Rijcken, J. P. Schouten, X. Xu, et al., “Airway Hype responsiveness to Histamine Asso r- ciated with Accelerated of Childhood Asthma and Ozone Pollution in At- Decline in FEV1,” American Journal of Respiratory and Critical Care Medicine, Vol. 151, No. 5, 1995, pp. 1377- 1382. [17] M. C. White, R. A. Etzel, W. D. Wilcox, et al., “Exacer- bations lanta,” Environmental Research, Vol. 65, No. 1, 1994, pp. 56-68. doi:10.1006/enrs.1994.1021 [18] I. Brüske-Hohlfeld, A. Peters and H. E. Wichmann, “Do Nanoparticles Interfere with Human Health?” Ecological ce Skating Facilities: An Internationa Perspectives for Science and Society, Vol. 14, No. 1, 2005, pp. 21-23. [19] M. Brauer, K. Lee, J. D. Spengler, et al., “Nitrogen Di- oxide in Indoor Il Survey,” Journal of the Air & Waste Management Asso- ciation, Vol. 47, No. 10, 1997, pp. 1095-1102. doi:10.1080/10473289.1997.10464399 [20] J. I. Levy, K. Lee, Y. Yanagisawa, et al., “Determi of Nitrogen Dioxide Concentrations in I nants ndoor Ice Skating Rinks,” American Journal of Public Health, Vol. 88, No. 12, 1998, pp. 1781-1786. doi:10.2105/AJPH.88.12.1781 [21] K. W. Rundell, “High Levels of Airborne Ultrafine and Fine Particulate Matter in Indoor Ice Arenas,” Inhalation Toxicology, Vol. 15, No. 3, 2003, pp. 237-250. doi:10.1080/08958370304502 [22] K. H. Kilburn, R. H. Warshaw and J. C. Thornton, “Expi- ratory Flows Decreased in Los Angeles Childr 1984 to 1987: Is this Evidenc en from e of Effects of Air Pollu- tion?” Environmental Research, Vol. 59, No. 1, 1992, pp. 150-158. doi:10.1016/S0013-9351(05)80235-X [23] L. Liu and J. Zhang, “Ambient Air Pollution and Chil- dren’s Lung Function in China” Environment Interna- tional, Vol. 35, No. 1, 2009, pp. 178-186. doi:10.1016/j.envint.2008.06.004 [24] S. Cakmak, R. Dales, J. Leech, et al., “The Influence of Air Pollution on Cardiovascular and Pulmo and Exercise Capacity: Canadian H nary Function ealth Measures Survey (CHMS)” Environmental Research, Vol. 111, No. 8, 2011, pp. 1309-1312. doi:10.1016/j.envres.2011.09.016 [25] S. D. Anderson and P. Kippelen, “Airway Injury as a Mechanism for Exercise-Induced Bronchoconstriction in Elite Athletes,” Journal of Allergy and Clinical Immuno- logy, Vol. 122, No. 2, 2008, pp. 225-235. doi:10.1016/j.jaci.2008.05.001 [26] S. D. Anderson and K. Holzer, “Exercise-Induced Asth- ma: Is It the Right Diagnosis in Elite Athle of Allergy and Clinical Immuntes?” Journal ology, Vol. 106, No. 3, 2000, pp. 419-428. doi:10.1067/mai.2000.108914 [27] M. W. Frampton, “Does Inhalation of Ultrafine Particles Cause Pulmonary Vascular Effects in Humans?” Inhala- tion Toxicology, Vol. 19, No. S1, 2007, pp. 75-79. doi:10.1080/08958370701495071 [28] C. C. Daigle, D. C. Chalupa, F. R. Gibb, et al., “Ultrafine Particle Deposition in Humans during Rest and Exer Inhalation Toxicology, Vol. 15, No cise,” . 6, 2003, pp. 539-552. doi:10.1080/08958370304468 [29] H. R. Anderson, R. Ruggles, K. D. Pandey, et al., “Am- bient Particulate Pollution and the World-Wide Preva- lence of Asthma, Rhino Conjunctivitis and Eczema in Children,” Occupational and Environmental Medicine, Vol. 67, No. 5, 2010, pp. 293-300. doi:10.1136/oem.2009.048785 [30] B. Brunekreef, A. W. Stewart, H. R. Anderson, et al., “Self-Reported Truck Traffic on the Street of and Symptoms of Asthma and Residence Allergic Disease,” Envi- ronmental Health Perspectives, Vol. 117, No. 11, 2009, pp. 1791-1798. doi:10.1289/ehp.0800467 [31] K. W. Rundell and D. M. Jenkinson, “Exercise-Induced Bronchospasm in the Elite Athletes,” Sports Medicine, Vol. 32, No. 9, 2002, pp. 583-600. doi:10.2165/00007256-200232090-00004 [32] W. Nystad, J. Harris and J. S. Borgen, “Asthma and Wheezing among Norwegian Elite Athl and Science in Sports and Exercise, Vol. 3 etes,” Medicine 2, No. 2, 2000, pp. 266-270. doi:10.1097/00005768-200002000-00003 [33] I. Helenius, H. O. Tikkanen and T. Haahtela, “Associa- tion between Type of Training and Risk of Asthma in Elite Athletes,” Thorax, Vol. 52, No. 2, 1997, pp.157-160. doi:10.1136/thx.52.2.157 [34] F. Messan, M. M. Lawani, T. Marqueste et al., “Evalu- ation du DEM25 chez 156 Enfants Exposés à la Pollution Automobile dans la Municipalité de Cotonou,”Mali Me- dical, Vol. 4, 2011, pp.16-21.
|