H. Wollerich et al. / Open Journal of Nursing 2 (2012) 307-310
308
It is not known if the same holds true for the reliability
of Tb during the direct post-operative phase in patients
admitted after cardiac surgery. Cardiac surgery involves
the opening of the chest and frequently the use of a
heart-lung machine. Thus during and after such surgery
important swings in hemodynamics and temperature can
occur. This may be particularly relevant given the large
thermal gradients from core to periphery that occur dur-
ing anesthesia and cardiac surgery [5].
Objective
In a prospective study we tested the hypothesis that after
cardiac surgery Tb adequately reflects Tpa, and at least
as good as Tr. We also examined the effect of varying
urinary flow rate on the Tb.
2. METHODS
During a 10-month study period (June 2009 to March
2010) consecutive patients aged >18 years, who were
undergoing cardiac surgery and admitted to the depart-
ment of critical care were evaluated for this study. Pa-
tients, with a ileal conduit urinary diversion also known
as Bricker ileal conduit, or patients with suprapubic
catheters, or other patients where urethral catheterization
was contraindicated as well as patients who were under-
going renal replacement therapy were excluded.
Only patients with both a PAC, a urinary bladder
catheter with temperature probe (Tb) and a rectal tem-
perature probe (Tr) were included.
Tb was measured by a probe incorporated in a Foley
urinary catheter (DeRoyal, Powell, USA). Tpa was meas-
ured by a pulmonary artery catheter (PAC) (Edwards,
Irvine California). Tr was measured by a digital ther-
mometer probe (Esophageal/Rectal temperature probe
25˚C - 45˚C, Philips Medical Systems, Andover, USA)
designed for axillar and rectal use. The temperature sen-
sors and the PAC were respectively connected to a tem-
perature and cardiac output module of the bedside moni-
tor (MP70, Philips Medical Systems, Eindhoven, the
Netherlands). Temperature values were recorded in de-
grees Celsius every 30 minutes by the ICU nurses. The
urinary production in ml was recorded every hour. All
data were collected until 24 h after admission or until
ICU discharge if this took place within 24 h.
Tpa was considered the reference value. Thus Tb was
compared with Tpa, and Tr was compared with Tpa us-
ing regression and Bland and Altman analysis.
Since no additional interventions were performed in-
formed consent was not required for this anonymized
analysis of data. The institutional review board of the
University Medical Center Groningen approved this ob-
servational study (METc 2008/279).
3. RESULTS
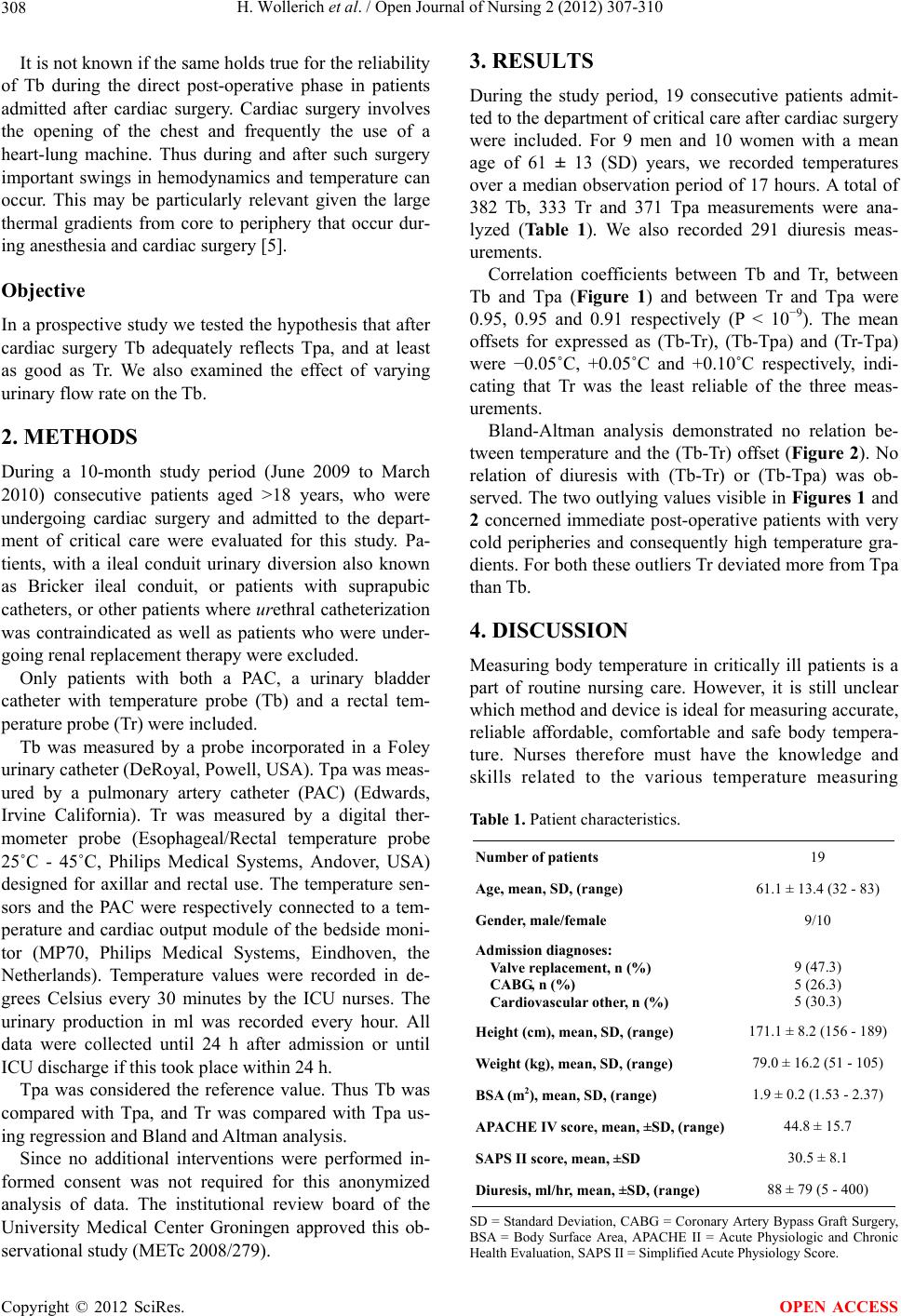
During the study period, 19 consecutive patients admit-
ted to the department of critical care after cardiac surgery
were included. For 9 men and 10 women with a mean
age of 61 ± 13 (SD) years, we recorded temperatures
over a median observation period of 17 hours. A total of
382 Tb, 333 Tr and 371 Tpa measurements were ana-
lyzed (Table 1). We also recorded 291 diuresis meas-
urements.
Correlation coefficients between Tb and Tr, between
Tb and Tpa (Figure 1) and between Tr and Tpa were
0.95, 0.95 and 0.91 respectively (P < 10−9). The mean
offsets for expressed as (Tb-Tr), (Tb-Tpa) and (Tr-Tpa)
were −0.05˚C, +0.05˚C and +0.10˚C respectively, indi-
cating that Tr was the least reliable of the three meas-
urements.
Bland-Altman analysis demonstrated no relation be-
tween temperature and the (Tb-Tr) offset (Figure 2). No
relation of diuresis with (Tb-Tr) or (Tb-Tpa) was ob-
served. The two outlying values visible in Figures 1 and
2 concerned immediate post-operative patients with very
cold peripheries and consequently high temperature gra-
dients. For both these outliers Tr deviated more from Tpa
than Tb.
4. DISCUSSION
Measuring body temperature in critically ill patients is a
part of routine nursing care. However, it is still unclear
which method and device is ideal for measuring accurate,
reliable affordable, comfortable and safe body tempera-
ture. Nurses therefore must have the knowledge and
skills related to the various temperature measuring
Table 1. Patient characteristics.
Number of patients 19
Age, mean, SD, (range) 61.1 ± 13.4 (32 - 83)
Gender, male/female 9/10
Admission diagnoses:
Valve replacement, n (%)
CABG, n (%)
Cardiovascular other, n (%)
9 (47.3)
5 (26.3)
5 (30.3)
Height (cm), mea n , SD, (rang e ) 171.1 ± 8.2 (156 - 189)
Weight (kg), mean, SD, (range) 79.0 ± 16.2 (51 - 105)
BSA (m2), mean, SD, (range) 1.9 ± 0.2 (1.53 - 2.37)
APACHE IV score, me an, ±SD, (range) 44.8 ± 15.7
SAPS II score, mean, ±SD 30.5 ± 8.1
Diuresis, ml/hr, mean, ±SD, (range) 88 ± 79 (5 - 400)
SD = Standard Deviation, CABG = Coronary Artery Bypass Graft Surgery,
BSA = Body Surface Area, APACHE II = Acute Physiologic and Chronic
Health Evaluation, SAPS II = Simplified Acute Physiology Score.
Copyright © 2012 SciRes. OPEN ACCESS