Paper Menu >>
Journal Menu >>
 Vol.2, No.8, 945-950 (2010) doi:10.4236/health.2010.28140 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ HEALTH A possible association between cervical erosion in pregnant women and congenital abnormalities in their children-a population-based case-control study Ferenc Bánhidy1, Nándor Ács1, Erzsébet H. Puhó2, Andrew E. Czeizel2* 1Second Department of Obstetrics and Gynecology, Semmelweis University, School of Medicine, Budapest, Hungary 2Foundation for the Community Control of Hereditary Diseases, Budapest, Hungary; *Corresponding Author: czeizel@interware.hu Received 25 February 2010; revised 24 March 2010; accepted 25 March 2010. ABSTRACT Objective to study the possible association between erosion of cervix in pregnant women (ECP) and structural birth defects, i.e. congeni- tal abnormalities (CA) in their offspring. Study design: Comparison of cases with CA and all matched controls without any CA born to wo- men with prospectively and medical record ECP in the population-based large data set of the Hungarian Case-Control Surveillance of Con- genital Abnormalities (HCCSCA). Results: HCC- SCA contained 22,843 cases and 38,151 matched controls, the informative offspring of 40 (0.18%) case mothers and the newborns of 25 control mothers (0.07%) with ECP were compared and the higher risk for total CA (adjusted OR with 95% CI: 2.7, 1.6-4.4) was found explained by the higher risk of 9 cases with hypospadias (OR with 95% CI: 4.5, 2.1-9.7) and 10 cases with car- diovascular CAs (OR with 95% CI: 3.4, 1.6-7.1), particularly with conotruncal CAs. Conclusions: An unexpected possible association of ECP with higher risk for hypospadias and conotrun- cal cardiovascular CAs was found and these findings are considered as signals that need confirmation or rejection Keywords: Erosion of Cervix in Pregnant Women; Birth Outcomes; Congenital Abnormalities; Hypospadias; Cardiovascular Malformations 1. INTRODUCTION The objective of our project entitled “Possible associa- tion of maternal diseases during pregnancy with adverse birth outcomes” is conducting a systematic analysis all recorded maternal diseases in the population-based large data set of the Hungarian Case-Control Surveillance of Congenital Abnormalities (HCCSCA) [1]. The prelimi- nary analysis of Erosion of Cervix in Pregnant Women (ECP) showed an unexpected association with high rate of total structural birth defects, i.e. Congenital Abnor- malities (CAs), thus it was necessary to evaluate the specific CAs in detail. The medical term for cervical erosion is cervical ectopy because the cells at the os of the cervix changes from the squamous cells normally found at this region to columnar cells and this patho- logical condition gives a red and eroded appearance [2]. To our best knowledge the possible association of ECP with CAs in their children has not been checked or re- ported in controlled epidemiological studies [3] thus the results of our case-control study based on the HCCSCA [4] are presented here. 2. MATERIALS AND METHODS 2.1. Subjects Cases with CA were selected from the Hungarian Con- genital Abnormality Registry (HCAR) [5] for the HCCSCA. Notification of cases with CA is mandatory for physicians from the birth until the first birthday to the HCAR and most CAs are reported by obstetricians (in Hungary practically all deliveries take place in inpa- tient obstetric clinics and birth attendants are obstetri- cians) or paediatricians (working at neonatal units of inpatient obstetric clinics as well as of various general and special inpatient and outpatient paediatric clinics). Autopsy during the study period was obligatory for all infant deaths and was performed in about 80% of still- born fetuses. Pathologists sent a copy of the autopsy report to the HCAR if defects were identified in stillborn fetuses or infant deaths. Fetal defects diagnosed by pre- natal diagnostic centres with or without elective termina- tion of pregnancy have also been reported to the HCAR 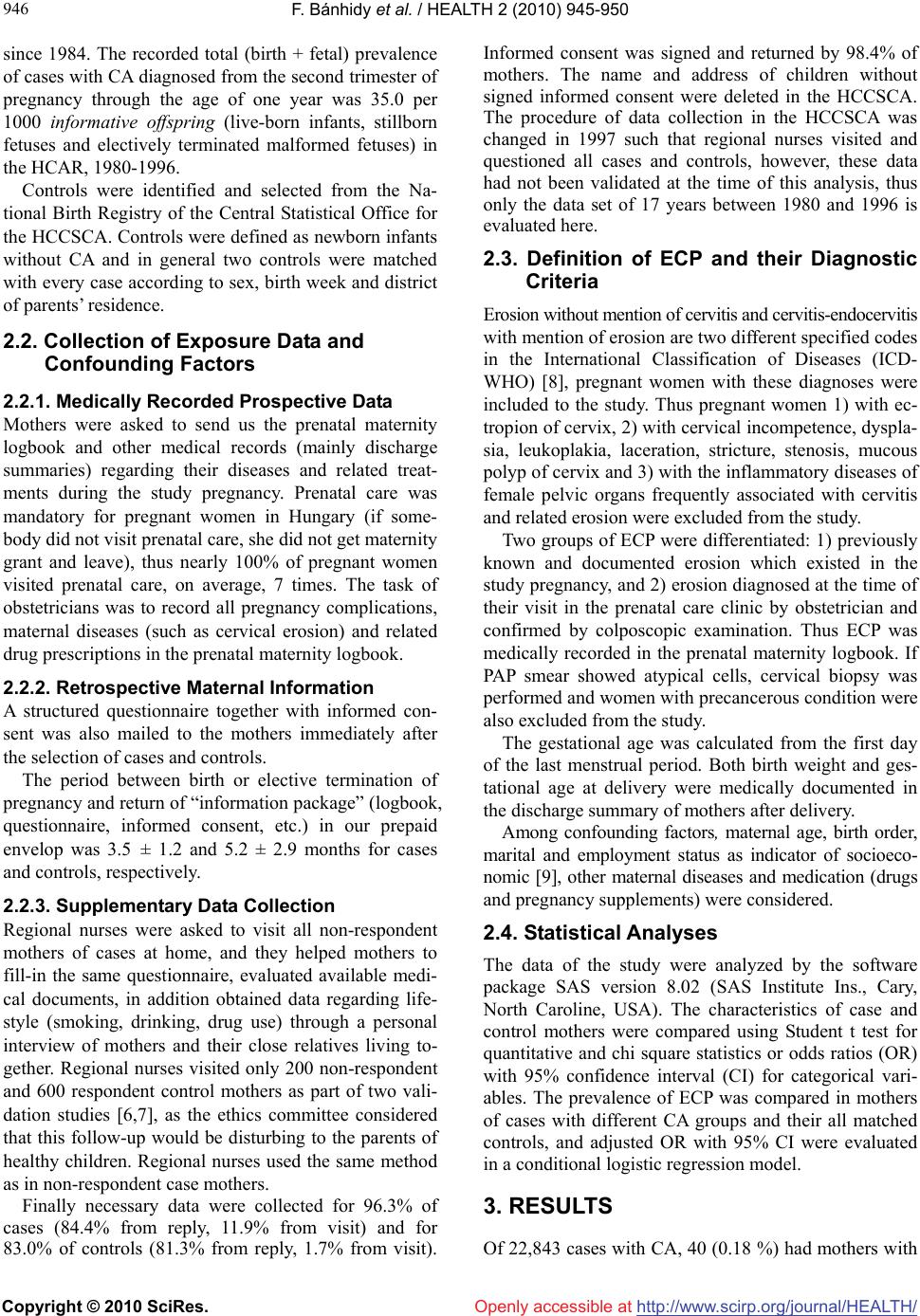 F. Bánhidy et al. / HEALTH 2 (2010) 945-950 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 946 since 1984. The recorded total (birth + fetal) prevalence of cases with CA diagnosed from the second trimester of pregnancy through the age of one year was 35.0 per 1000 informative offspring (live-born infants, stillborn fetuses and electively terminated malformed fetuses) in the HCAR, 1980-1996. Controls were identified and selected from the Na- tional Birth Registry of the Central Statistical Office for the HCCSCA. Controls were defined as newborn infants without CA and in general two controls were matched with every case according to sex, birth week and district of parents’ residence. 2.2. Collection of Exposure Data and Confounding Factors 2.2.1. Medically Recorded Prospective Data Mothers were asked to send us the prenatal maternity logbook and other medical records (mainly discharge summaries) regarding their diseases and related treat- ments during the study pregnancy. Prenatal care was mandatory for pregnant women in Hungary (if some- body did not visit prenatal care, she did not get maternity grant and leave), thus nearly 100% of pregnant women visited prenatal care, on average, 7 times. The task of obstetricians was to record all pregnancy complications, maternal diseases (such as cervical erosion) and related drug prescriptions in the prenatal maternity logbook. 2.2.2. Retrospective Maternal Information A structured questionnaire together with informed con- sent was also mailed to the mothers immediately after the selection of cases and controls. The period between birth or elective termination of pregnancy and return of “information package” (logbook, questionnaire, informed consent, etc.) in our prepaid envelop was 3.5 ± 1.2 and 5.2 ± 2.9 months for cases and controls, respectively. 2.2.3. Supplementary Data Collection Regional nurses were asked to visit all non-respondent mothers of cases at home, and they helped mothers to fill-in the same questionnaire, evaluated available medi- cal documents, in addition obtained data regarding life- style (smoking, drinking, drug use) through a personal interview of mothers and their close relatives living to- gether. Regional nurses visited only 200 non-respondent and 600 respondent control mothers as part of two vali- dation studies [6,7], as the ethics committee considered that this follow-up would be disturbing to the parents of healthy children. Regional nurses used the same method as in non-respondent case mothers. Finally necessary data were collected for 96.3% of cases (84.4% from reply, 11.9% from visit) and for 83.0% of controls (81.3% from reply, 1.7% from visit). Informed consent was signed and returned by 98.4% of mothers. The name and address of children without signed informed consent were deleted in the HCCSCA. The procedure of data collection in the HCCSCA was changed in 1997 such that regional nurses visited and questioned all cases and controls, however, these data had not been validated at the time of this analysis, thus only the data set of 17 years between 1980 and 1996 is evaluated here. 2.3. Definition of ECP and their Diagnostic Criteria Erosion without mention of cervitis and cervitis-endocervitis with mention of erosion are two different specified codes in the International Classification of Diseases (ICD- WHO) [8], pregnant women with these diagnoses were included to the study. Thus pregnant women 1) with ec- tropion of cervix, 2) with cervical incompetence, dyspla- sia, leukoplakia, laceration, stricture, stenosis, mucous polyp of cervix and 3) with the inflammatory diseases of female pelvic organs frequently associated with cervitis and related erosion were excluded from the study. Two groups of ECP were differentiated: 1) previously known and documented erosion which existed in the study pregnancy, and 2) erosion diagnosed at the time of their visit in the prenatal care clinic by obstetrician and confirmed by colposcopic examination. Thus ECP was medically recorded in the prenatal maternity logbook. If PAP smear showed atypical cells, cervical biopsy was performed and women with precancerous condition were also excluded from the study. The gestational age was calculated from the first day of the last menstrual period. Both birth weight and ges- tational age at delivery were medically documented in the discharge summary of mothers after delivery. Among confounding factors, maternal age, birth order, marital and employment status as indicator of socioeco- nomic [9], other maternal diseases and medication (drugs and pregnancy supplements) were considered. 2.4. Statistical Analyses The data of the study were analyzed by the software package SAS version 8.02 (SAS Institute Ins., Cary, North Caroline, USA). The characteristics of case and control mothers were compared using Student t test for quantitative and chi square statistics or odds ratios (OR) with 95% confidence interval (CI) for categorical vari- ables. The prevalence of ECP was compared in mothers of cases with different CA groups and their all matched controls, and adjusted OR with 95% CI were evaluated in a conditional logistic regression model. 3. RESULTS Of 22,843 cases with CA, 40 (0.18 %) had mothers with  F. Bánhidy et al. / HEALTH 2 (2010) 945-950 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 947 947 ECP, while of 38,151 controls, 25 (0.07%) were born to pregnant women affected with ECP. The diagnosis of ECP was based on colposcopic examination and pro- spectively (at the first visit between the 6th and 10th gestational weeks in the prenatal care clinics) medically recorded in the prenatal maternity logbook. Thus the onset of ECP was considered to be before conception or in early pregnancy. Of 40 case mothers, 13 (32.5) had the diagnosis of ECP with cervitis, while of 25 control mothers, 4 (16.0%) had the similar combined diagnosis. Table 1 summarizes the most important maternal variables. Mean maternal age and birth order in mothers with ECP did not differ significantly from the figures of the reference sample. The proportion of unmarried women was somewhat higher in pregnant women with ECP. Control pregnant women with ECP showed a higher socioeconomic status on the basis of their em- ployment status than case pregnant women with ECP. The use of folic acid during pregnancy was higher in control mothers particularly affected with ECP than in case mothers. A similar trend was seen in the use of mul- tivitamins as well. However, these differences did not reach the level of significance due to the limited number of affected pregnant women. Of 2,640 case mothers visited at home, 5 (0.19%) had ECP and 3 (60.0%) were smoker during the study preg- nancy. Of 2,635 mothers without ECP, 575 (21.8%) smoked. Of 800 control mothers visited at home, 152 (19.0%) smoked during the study pregnancy, only one smoker had the diagnosis of ECP. Among maternal diseases, the prevalence of haemor- rhoids was higher both in case mothers (10.0% vs. 3.5%) and control mothers (12.0% vs. 4.3%) with ECP com- pared to pregnant women without ECP. The incidence of threatened preterm delivery (22.5% vs. 11.4% in case and 44.0% vs. 14.3% in control mothers) and anaemia (32.5% vs. 14.2% in case and 28.0% vs. 16.7% in control mothers) was much higher in pregnant women with ECP. Allylestrenol, diazepam, promethazine and terbutaline were used for the prevention/treatment of threatened preterm delivery therefore these drugs showed a higheruse in pregnant women with ECP compared to pregnant women without ECP as reference (Table 2). However, clotrimazole and other antifungal drugs were also used more frequently by pregnant women with ECP. Only allylestrenol treatment occurred more frequently in Table 1. Maternal characteristics Maternal variables Quantitative Case mothers without with ECP (N = 22,803) (N = 40) Control mothers without with ECP (N = 38,126) (N = 25) Comparison of case and control mothers with ECP Maternal age, yr. No. % No. % No. % No.% p = – 19 2,501 11.0 5 12.5 3,2778.6 0 0.0 20 – 29 15,56468.3 29 72.5 27,58372.319 76.0 30 – 4,738 20.8 6 15.0 7,26619.16 24.0 0.21* Mean, S.D. 25.5 ± 5.3 24.5 ± 4.6 25.5 ± 4.9 25.8 ± 4.3 0.33** Birth order (parity) 1 10,69046.9 18 45.0 18,19647.713 52.0 2 or more 12,13353.1 22 55.0 19,93052.312 48.0 0.72* Mean, S.D. 1.9 ± 1.1 1.9 ± 1.5 1.7 ± 0.9 1.8 ± 1.0 0.27** Categorical No. % No. % No. % No. % Unmarried 1,264 5.5 5 12.5 1,470 3.9 2 8.0 0.50** Employment status Professional 1,973 8.7 4 10.0 4,41911.64 16.0 Managerial 5,093 22.3 4 10.0 10,25626.99 36.0 Skilled worker 6,489 28.5 12 30.0 11,90131.27 28.0 Semiskilled worker 4,191 18.4 6 15.0 6,15716.14 16.0 Unskilled worker 1,770 7.8 6 15.0 2,1875.7 0 0.0 Housewife 2,400 10.5 6 15.0 2,3536.2 1 4.0 Others 887 3.9 2 5.0 853 2.2 0 0.0 0.12** Pregnancy supplements OR 95% CI Iron 14,71664.5 26 65.0 26,75170.220 80.0 0.8 0.5 – 1.3 Folic acid 11,25949.4 20 50.0 20,75854.417 68.0 0.7 0.4 – 1.7 Multivitamins 1,327 5.8 3 7.5 2,506 6.6 3 12.0 0.6 0.2 – 2.7 *chi-square test; **Student t-test  F. Bánhidy et al. / HEALTH 2 (2010) 945-950 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 948 control mothers than case mothers with ECP. The birth outcomes of control newborns without CA are presented in Table 3 because CAs in cases may have a more drastic effect for gestational age and birth weight than ECP. There was no significant difference in these variables of controls born to mothers with or without ECP. The estimation regarding the possible association of ECP with the risk of different CAs including at least 3 cases is shown in Table 4. The total rate of CAs showed a higher risk explained by the higher risk of hypospadias in 9 cases and cardiovascular CAs in 10 cases. The mi- nor anomaly manifestation of hypospadias, i.e. coronal type was excluded in the HCAR. The distribution of cardiovascular CAs was the following: transposition of great vessels 1, tetralogy of Fallot 3, ventricular septal defect 3, congenital stenosis of aortic valve 1, persistent ductus arteriosus 1, unspecified 1. 4. DISCUSSION Our population-based case-control study showed a higher risk of hypospadias, and cardiovascular CAs in the chil- dren of women with ECP. Transposition of great vessels, tetralogy of Fallot, and certain part of ventricle septal defects can be combined in the group of conotruncal defects [10], and of 10 cases with cardiovascular CAs, 7 belonged to this group. A higher risk of threatened preterm delivery was re- corded in women with ECP but it did not associate with a higher risk of preterm births on the contrary of the somewhat shorter gestational age. Thus there was an overdiagnosis of threatened preterm delivery or its treatment was very effective. The higher rate of anaemia can be explained partly by the higher rate of haemor- rhoids. The crucial point of the study is the diagnostic validity of ECP. Our study design excluded pregnant women with secondary erosion due to the inflammatory diseases of genital organs. However, about half of case and con- trol mothers with ECP were treated by antimicrobial drugs, thus the infectious origin of ECP cannot be ex- cluded in some pregnant women. Table 2. Frequently used drugs in pregnant women with ECP. Drugs Case mothers without with ECP (N = 22,803) (N = 40) Control mothers without with ECP (N = 38,126) (N = 25) Comparison of case and control mothers with ECP No. % No. % No. % No. % OR 95% CI Allylestrenol 3,472 15.2 9 22.5 5,346 14.0 11 44.0 0.5 0.3 – 0.9 Clotrimazole 1,627 7.1 14 35.0 3,070 8.1 7 28.0 1.3 0.7 – 1.7 Diazepam 2,737 12.0 9 22.5 4,126 10.8 4 16.0 1.4 0.8 – 2.9 Econazole, fluconazole, natamycin, nystatin 248 1.1 6 15.0 408 1.1 4 16.0 0.9 0.3 – 3.4 Metronidazole 383 1.7 5 12.5 565 1.5 5 20.0 0.7 0.2 – 2.9 Metronidazole + micona- zole* 572 2.5 4 10.0 843 2.2 3 12.0 0.8 0.1 – 3.3 Promethazine 3,638 16.0 10 25.0 6,019 15.8 6 24.0 1.0 0.7 – 1.4 Terbutaline 2,340 10.3 10 25.0 3,988 10.5 6 24.0 1.0 0.7 – 1.5 Table 3. Birth outcomes of newborn infants without defects born to women with and without ECP (the latter group as reference). Va ri abl es Pregnant womenwithout with ECP Comparison (N = 38,126) (N = 25) (adjusted) Quantitative Mean S.D. Mean S.D. p = Gestation age at delivery (wk) 39.4 2.1 39.1 2.1 0.12* Birth weight (g) 3,276 511 3,237 586 0.49** Categorical No. % No. % OR (95% CI) Preterm births (less than 37 completed gestational week) 3,494 9.2 2 8.0 0.9 (0.6-1.8)* Low birthweight newborns (less than 2500 g) 2,165 5.7 2 8.0 1.2 (0.7-2.9)** *adjusted for maternal age, birth order and maternal socio-economic status; **adjusted for maternal age, birth order, maternal socio-economic status and gestation age  F. Bánhidy et al. / HEALTH 2 (2010) 945-950 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 949 949 Table 4. Estimation of possible association of maternal ECP with different CAs in their offspring compared to the occurrence of ECP during the study pregnancy in case and control mothers. Study groups Grand total N Pregnancy No. % OR 95% CI** Controls 38,151 25 0.07 Reference Cases with Cardiovascular CAs* 4,480 10 0.22 3.4 1.6 – 7.1 Undescended testis* 2,052 3 0.15 2.2 0.7 – 7.4 Hypospadias* 3,038 9 0.30 4.5 2.1 – 9.7 Clubfoot* 2,424 3 0.12 1.9 0.6 – 6.3 Poly/syndactyly* 1,744 3 0.17 2.6 0.8 – 8.7 Other CAs 9,105 12* 0.13 1.7 0.8 – 3.9 Total 22,843 40 0.18 2.7 1.6 – 4.4 *isolated CAs; **spina bifida with hydrocephalus, atresia of external auditory canal with absence of auricle, anotia, tracheal stenosis, cleft lip, cleft lip + cleft palate, oesophageal atresia, anal atresia, cystic kidney, torticollis, multiple CA: ventricular septal defect + cleft palate + undescended testis, multiple CA: branchial cyst + rectal atresia + clubfoot; *** adjusted OR for maternal age (< 20 yr vs. 20-29 yr vs. 30 yr or more), and employment status (professional-managerial-skilled worker vs. semiskilled worker-unskilled worker-housewife vs. others), birth order (first delivery vs. one or more previous deliveries), and ECP drug treatments(as a dichotomous variable); Bold numbers show significant associations. Theoretically 3 causes are worth differentiating in the origin of ECP: 1) Trauma, however, it is not likely dur- ing early pregnancy. 2) Topical chemicals (e.g. sper- maticidal contraceptive creams) were not used by these pregnant women. 3) The high level of estrogens in the body during pregnancy. At the evaluation of the possible association between ECP and higher risk of hypospadias and conotruncal defects, the effect of ECP itself, the causes of ECP, re- lated drug treatments, other confounders and chance effect should be considered. The direct effect of ECP for the organogenesis of em- bryo/fetus does not seem to be plausible. The causes of ECP may have some association with higher risk of CAs. Our previous study showed an asso- ciation of acute pelvic inflammatory diseases with 4.2- folds higher risk of atrial septal defect, type II [11], however, this type of cardiovascular CA did not occur in the study. Estrogens may have some teratogenic effect in particular circumstances. A higher risk of hypospadias was found in pregnant women exposed to an elevated estrogen intake from drugs or such dietary sources as milk or soy [12]. This hypothesis was supported by an experimental study in mice, showing that supraphysi- ological doses of synthetic estrogen during pregnancy induce hypospadias in 50% of the male fetuses [13]. Some epidemiological studies indicated a causal asso- ciation between sex hormones, particularly oral contra- ceptives and cardiovascular CAs [14] but other studies did not confirm this association [15]. Obviously this possible association may occur only in women and/or fetuses with special genetic predisposition both for ECP and CAs triggered by these hormonal factors. The teratogenic potential of clotrimazole, metronida- zole, metronidazole+miconazole, econazole, nystatin, natamycin, fluconazole was checked in the previous studies based on HCCSCA and these drugs did not show an association with higher risk of hypospadias and car- diovascular CAs [16]. The drugs used for the treatment of threatened preterm delivery such as diazepam [17] and promethazine [18] did also not show any association with a higher risk of hypospadias and cardiovascular CAs in the data set of the HCCSCA, in addition in 112 and 32 pregnant women who attempted suicide with large doses of diazepam [19] and promethazine [20], respectively. However, allylestrenol had some associa- tion with a higher risk of hypospadias [21], but this hormone was used more frequently by control mothers than by case mothers with ECP and at the calculation of adjusted OR was considered. The effect of other and unknown confounders may also be important, finally the chance effect cannot be excluded in multiple testing. The association of ECP with cardiovascular CAs and hypospadias is significant, but the small numbers of cases and controls greatly re- duced the robustness of these associations. The strengths of the study are 1) population-based large data set of the HCCSCA including 65 pregnant women with prospectively and medically recorded ECP based on colposcopic examination in ethnically ho- mogenous European (Caucasian) people. 2) The match- ing of cases and controls, 3) in addition most confound- ers such as other maternal diseases and related treat- ments are known. 4) The good validity of CA diagnoses due to the medically reported cases to the HCAR which were checked by a paediatrician and medical geneticist [5], in addition new information from recent medical examinations and the questionnaire was helpful to ex-  F. Bánhidy et al. / HEALTH 2 (2010) 945-950 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/ 950 Openly accessible at clude cases with misdiagnosed CA or to correct the CA diagnosis in the HCCSCA [4]. However, our data set also has serious weaknesses. 1) ECP is a symptom and not a clinical entity. The study design excluded secondary ECP due to microbial origin, however, the use of antimicrobial drugs questioned the diagnostic criteria of ECP in the study. 2) In general data were not available regarding the possible electro- or cryocautery and diathermy in pregnant women with ECP. The unexpected findings of our study would need a bio- logically plausible explanation. Our hypothesis is based on a special genetic predisposition in pregnant women with a much higher sensitivity for the high level of estrogens during pregnancy. This higher level of estrogens ex- plains the common occurrence of cervical erosion in pregnant women and may associate with a higher risk of hypospadias and conotruncal cardiovascular CA in their offspring. In conclusion, our population-based case-control study showed an association of ECP in early pregnancy with a higher risk for hypospadias and conotruncal cardiovas- cular CAs. These findings are considered only as a sig- nal and further studies are needed to confirm or reject these associations. 5. ACKNOWLEDGEMENTS This study was partly sponsored by a generous grant from Richter Gedeon Pharmaceuticals Ltd., Budapest, Hungary. REFERENCES [1] Czeizel, A.E., Ács, N., Bánhidy, F. and Vogt, G. (2006) Possible association between maternal diseases during pregnancy and congenital abnormalities. In: Engels, J.V., Ed. Birth defects: New research. NOVA Science Pub- lisher, New York, 55-70. [2] Gabbe, S.G., Niebyl, J.R. and Simpson, J.L. (2001) Ob- stetrics: Normal and problem pregnancies. 4th Edition, Churchill Livingstone, New York. [3] Shepard, T.H. and Lemire, R.J. (2004) Catalog of Tera- togenic Agents, 11th Edition. Johns Hopkins University Press, Baltimore. [4] Czeizel, A.E., Rockenbauer, M., Siffel, C. and Varga, E. (2001) Description and mission evaluation of the hun- garian case-control surveillance of congenital abnormali- ties, 1980-1996. Teratology, 63(5), 176-185. [5] Czeizel, A.E. (1997) First 25 years of the hungarian con- genital abnormality registry. Teratology, 55(5), 299-305. [6] Czeizel, A.E., Petik, D. and Vargha, P. (2003) Validation studies of drug exposures in pregnant women. Pharma- coepid Drug Safety, 12(5), 409-416. [7] Czeizel, A.E. and Vargha, P. (2004) Periconceptional folic acid/multivitamin supplementation and twin pre- gnancy. American Journal of Obstetrics and Gynecology, 191(3), 790-794. [8] WHO. (2007) International classification of disease. 10th revision, Wold Health Organization, Geneva [9] Puho, E., Métneki, J. and Czeizel, A.E. (2005) Maternal employment status and isolated orofacial clefts in Hungary. Central European Journal of Public Health, 13(3), 144-148. [10] Adams, F.H., Emmanouilideas, G.C. and Riemenschnei- der, T.A. (1989) Heart disease in infants, children and adolescents. Williams and Wilkins, Baltimore. [11] Ács, F., Bánhidy, F., Puho, H.E. and Czeizel, A.E. (2008) Possible association between acute pelvic inflammatory disease in pregnant women and congenital abnormalities in their offspring? A population-based case-control study. Birth Defects Research (Part A), 82(8), 563-570. [12] Sharpe, R.M. and Skakkeback, N.E. (1993) Are oestro- gens involved in falling sperm counts and disorders of the male reproductive tract? Lancet, 341(8857), 1392- 1395. [13] Kim, K.S., Torres, C.R. Jr, Yucel, S., et al. (2004) Induc- tion of hypospadis in a murine model by maternal expo- sure to synthetic estrogens. Environmental Research, 94, 267-275. [14] Janerich, D.T., Dugan, J.M., Standfast, S.J. and Strite, L. (1977) Congenital heart disease and prenatal exposure to exogenous sex hormeones. British Medical Journal, 1(6068), 1058-1060. [15] Bracken, M.B. (1990) Oral contraception and congenital malformations in offspring: A review and meta-analysis of the prospective studies. Obstetrics & Gynecology, 76(3), 552-557. [16] Czeizel, A.E. (2009) The estimation of human terato- genic/fetotoxic risk of exposures to drugs on the basis of Hungarian experience: a critical evaluation of clinical and epidemiological models of human teratology. Expert Opinion on Drug Safety, 8(3), 283-303. [17] Czeizel, A.E., Erős, E., Rockenbauer, M., Sørensen, H.T. and Olsen, J. (2003) Shortterm oral diazepam treatment during pregnancy—A population-based teratological case-control study. Clinical Drug Investigation, 23, 451- 462. [18] Bártfai, Z., Kocsis, J., Puhó, H.E. and Czeizel, A.E. (2008) A population-based case-control study of pro- methazine use during pregnancy. Reproductive Toxicol- ogy, 25(2), 276-285. [19] Gidai, J., Ács, N., Bánhidy, F. and Czeizel, A.E. (2008) No association found between use of very large doses of diazepam by 112 pregnant women for a suicide attempt and congenital abnormalities in their offspring. Toxic In- dust Health, 24, 29-39. [20] Petik, D., Ács, N., Bánhidy, F. and Czeizel, A.E. (2008) A study of the potential teratogenic effects of large doses of promethazine in 32 self-poisoned pregnant women. Toxic Indust Health, 24(1-2), 87-96. [21] Czeizel, A.E. and Huiskes, N. (1988) A case-control study to evaluate the risk of congenital anomalies as a result of allylestrenol therapy during pregnancy. Clinical Therapeutics, 10, 725-739. |

