 Open Journal of Psychiatry, 2012, 2, 305-316 OJPsych http://dx.doi.org/10.4236/ojpsych.2012.24043 Published Online October 2012 (http://www.SciRP.org/journal/ojpsych/) Elderly patients with very late-onset schizophrenia-like psychosis and early-onset schizophrenia: Cross-sectional and retrospective clinical findings Caroline Girard1,2, Martine Simard1,2* 1School of Psychology, Laval University, Quebec City, Canada 2Research Centre at Mental Health University Institute of Quebec, Quebec City, Canada Email: *Martine.Simard@psy.ulaval.ca Received 15 June 2012; revised 18 July 2012; accepted 29 July 2012 ABSTRACT Objectives: The aim of this study was to characterize the symptoms at onset/past and current symptoms of patients with Very Late-Onset Schizophrenia-Like Psychosis (VLOSLP; first onset of psychotic symp- toms at/or after 60 years old) with those of elderly patients diagnosed with schizophrenia before the age of 40 years old (Early-Onset Schizophrenia—EOS) in order to validate the clinical nosology proposed by the International Late-Onset Schizophrenia Group. Methods: This is a between-patient comparison study with retrospective and current data taken from an historical cohort that was conducted from May/2005 to August/2008. Seventeen VLOSLP and 17 EOS were included. Schizophrenia and schizophrenia-like psychotic disorders were initially diagnosed by board- certified psychiatrists with the Diagnostic and Statis- tical Manual Criteria at use at onset of the disorders. Patients’ symptoms were assessed with the Scale for the Assessment of Positive Symptoms (SAPS) and the Scale for the Assessment of Negative Symptoms (SANS). The general scores on the SAPS/SANS were the primary outcomes. Results: Both groups had hal- lucinations and delusions at onset of the disease, but the following symptoms were more present and se- vere in EOS than in VLOSLP: hallucinations (p = 0.001); assiduity loss (p < 0.001); grandiosity (p = 0.001); reference (p < 0.001) and influence (p = 0.001) delusions. VLOSLP had mostly persecutory delusions. At current evaluation (follow-up of cohort), most pa- tients in the two groups presented residual symptoms of anhedonia and apathy, but EOS, presented more symptoms of friendship poverty (d = 1.42, larg e effect size) than VLOSLP. The neuroimaging studies (when available) at follow-up demonstrated greater vascular cerebral lesions/vulnerability in VLOSLP than in EOS patients. Conclusion: This study showed that both VLOSLP and EOS had positive and negative symptoms in the past/at onset of the disease, but they were more severe in EOS than in VLOSLP. However, the positive symptoms of both groups at follow-up of the cohort (current evaluation) responded relatively well to neuroleptics. Keywords: Psychosis; Negative Symptoms; Schizophrenia; Very-Late-Onset 1. INTRODUCTION A recent study found that the one-year prevalence of all schizophrenia spectrum disorders in individuals aged 60 years and older was 0.71% [1]. Clearly, with the aging of population, these late-onset disorders will become a more important health issue [2,3]. Indeed the greatest per-capita expenditures for individuals with schizophre- nia were reported among the older beneficiaries [4]. At the beginning of the new millennium, The International Late-Onset Schizophrenia (ILOS) Group attempted to disentangle inconsistencies regarding the diagnostic sys- tems and nomenclature of late-onset schizophrenia/psy- chosis disorders [5]. Following a Medline literature re- view and two days of debate, this group achieved con- sensus on diagnosis and recommended a nosology for these disorders: The diagnosis of late-onset schizophre- nia (LOS) for an illness onset after the age of 40 and the diagnosis of very-late-onset schizophrenia-like psychosis (VLOSLP) for an illness onset after the age of 60. The International Late-Onset Schizophrenia Group proposed that early-onset schizophrenia or EOS (onset before the age of 40) and LOS (onset after 40 years old) would be more similar than different in terms of symptoms [5,6] whereas VLOSLP (onset after 60 years old) would pre- sent with a lower prevalence of formal thought disorder and affective blunting, and a higher prevalence of visual hallucinations than EOS [5]. This nomenclature may *Corresponding author. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 306 have had face validity and clinical utility, but required further investigation in several domains, especially re- garding the differential clinical symptomatology with EOS [5,7]. Following the publication of the nomenclature pro- posed by the ILOS Group, numerous studies were con- ducted to differentiate the clinical profile between LOS and EOS patients [6,8-17]. However, because the present paper will rather focus on VLOSLP/EOS than on LOS/ EOS, the LOS/EOS differential nomenclature will not be further developed; the interested readers shall consult Pearman and Batra [6] for a recent review on this par- ticular topic. Studies on VLOSLP alone [18-23], as well as studies comparing the profile of patients with VLOSLP with that of patients with LOS [14,24,25], elderly EOS [14,24, 26-29] and healthy controls [30,31] were also realized to better differentially characterize the demographics, clini- cal symptoms and evolution [14,20,29] of VLOSLP pa- tients. In terms of positive symptoms, mild paranoid delu- sions [14,26] mostly persecutory [18,20,21,24,25], audi- tory [18,21,25,26] and visual hallucinations [18,21,25], as well as all the Scale for the Assessment of Positive Symptoms (SAPS) [32] behavioral disturbances except for psychomotor abnormalities [25] were described in VLOSLP. These symptoms were sometimes as common as in LOS [25]. However, presence of formal thought disorders in VLOSLP generated contradictory results. Some authors reported formal thought disorders in 100% of French-speaking VLOSLP patients [25], while other authors working mostly on English- and Deutsch-speak- ing patients reported a low prevalence [18], and a lower risk of formal thought disorder in VLOSLP than in EOS patients [14]. Formal thought disorder was found to be absent in VLOSLP patients in the remaining studies [20, 24]. The presence of negative symptoms was also very controversial [14,20,21,25]. In a previous study realized by our team [25], both VLOSLP and LOS patients pre- sented with several negative symptoms as measured by the Scale for the Assessment of Negative Symptoms (SANS) [33]; only apathy was more frequent in LOS than in VLOSLP. However, in most studies, negative symptoms were absent in VLOSLP [14,20] while they were present in EOS and to a lesser extent in LOS [14]. Negative symptoms were not at all or barely mentioned in several studies on VLOSLP [18,21,24,26]. Regarding the evolution of VLOSLP, Mazeh and col- leagues [29] reported that the majority of VLOSLP pa- tients did not present cognitive and functional deteriora- tion over a mean follow-up period of 30 months, on the contrary to EOS patients (42% with functional decline and 16% with cognitive decline). However, the research- ers only administered the Clinical Global Impression (CGI) scale and a telephone interview in which they asked 3 questions to the caregiver in order to assess the cognitive and functional status of the patient. Köhler and colleagues [14] also found that generally, later age of onset was associated with better outcome, although there was a significant gender by age of onset interaction, with men displaying poorer outcome in the EOS/LOS group and women tending to have a worse outcome in the VLOSLP. Good response to antipsychotics [24,26,34,35], even better than in LOS [24] and elderly EOS patients [24,26], was often registered in VLOSLP patients. VLOSLP in- dividuals, especially inpatients [35], responded well to atypical antipsychotics [20,35], and in particular to ami- sulpride [34]. In terms of sociodemographics, there was generally a female preponderance in VLOSLP [1,14,18,20,22,24-26, 29]. Regarding education, in one instance patients with VLOSLP were described as being more educated than elderly EOS [26] but in another study they were reported to be less educated than LOS [25]. Regarding social abilities, VLOSLP patients were described as having a better premorbid social functioning than elderly EOS, because they had been more married [26] and/or wi- dowed/divorced [22,25] than single. However, other au- thors found that a majority of VLOSLP patients living in the community were alone [20]. Male patients with VLOSLP might be more socially isolated than women [23]. Interestingly, some studies have shown that ethnicity might play a role on the demographics and symptoms’ profiles of VLOSLP [20-23]. Some authors reported that Black Caribbean [20,21] as well as migrant patients with different ethnic origins [22,23] diagnosed with VLOSLP were younger and more likely to be male than their Brit- ish counterparts. Black Caribbean VLOSLP patients tended to present more with delusions of a “bizarre” or mystical nature and with a somatic or hypochondriacal content than British patients [21]. In summary, studies on VLOSLP patients over the last decade have consistently reported the presence of para- noid delusions and generally less severe positive symp- toms than in EOS. However, the presence/absence and severity of negative symptoms remains a controversial issue. Regarding the evolution of VLOSLP, gender might have an impact on the outcome, with VLOSLP women possibly having a poorer prognosis than men; but few studies addressed this question so further research are required. Finally, ethnicity might play a role in demo- graphic characteristics as well as in the clinical profile of VLOSLP patients. As there were very few studies con- ducted on a French-speaking population with VLOSLP, the differential clinical and sociodemographic profile of Copyright © 2012 SciRes. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 307 French-speaking patients with VLOSLP versus that of French-speaking patients with EOS shall be further in- vestigated. Indeed, do VLOSLP patients share the same symptomatology/etiology than EOS, or do they have a neurodegenerative and/or neurovascular substrate to their disorder as it has been suggested by some authors [36- 38]? To address these issues, our team performed a histori- cal cohort study on the cognitive and clinical profile/ evolution of elderly patients with VLOSLP versus those of patients with life-long EOS. The detailed method and cognitive results were presented in a previous report [39]. In summary, although VLOSLP and EOS patients did not meet the diagnostic criteria for dementia at onset of the psychotic disorder, the results showed that the groups presented at follow-up with cognitive deficits in several domains, and 20% of VLOSLP had developed dementia overtime (after onset of psychotic disorders) compared to 5.9% of EOS [39]. The objective of the present paper is thus to present the clinical results of this historical cohort study, i.e. to characterize and compare the current (follow-up) and past (at onset of the psychotic disorder) positive and negative symptoms of patients with VLOSLP with those of patients aged 55 years and older who received a diag- nosis of EOS. In terms of clinical profile, VLOSLP were hypothesized to present with less severe current (follow- up) and past positive symptoms than EOS, to present with some negative symptoms, but of less severity than those of EOS patients. In terms of demographics, VLO- SLP were hypothesized to be predominantly female, to have a better premorbid social functioning, i.e. to be more married/widowed/divorced than EOS (more single), and to be less educated than EOS, per the findings of a previous study on a French-speaking population by our team [25]. 2. METHODS Research design and settings: This was a between- patient comparison study made at follow-up, with a ret- rospective component (onset of the psychotic disorder), following the historical cohort [39]. Patients were re- cruited in psychiatric/geriatric psychiatry units of five hospitals in the province of Quebec, Canada. Participants: Seventeen elderly patients presenting for the first time at/or after 60 years old with either schi- zophrenia, schizophreniform disorder, delusional disor- der, non-specific psychotic disorder or paraphrenia (VLO- SLP) were compared to 17 patients aged 55 years old and older who had received a diagnosis of schizophrenia before the age of 40 (EOS). Supplementary inclusion criteria for both groups involved: 1) The absence of de- mentia at onset of the initial psychotic episode (per the medical chart) (onset of historical cohort); and 2) psy- chotic symptoms at onset (of historical cohort) not ex- plained by another psychiatric and/or neurological and/or systemic/medical disorder. The initial diagnoses had to be made by board-certified psychiatrists using the offi- cial Diagnostic and Statistical Manual Criteria (DSM) employed at the time. Ethical considerations: This research was approved by the Ethical Research Committee of all hospitals in- volved in this study. Written informed consent was ob- tained from every patient and/or legal substitute by a research assistant not involved in the evaluation. Patients had to: 1) Consent to participate in the evaluations of the study; 2) Allow the investigator to review the medical file or, if not, accept to answer a socio-demographic/medical questionnaire; 3) Allow an investigator to contact a fa- mily member/friend (facultative, given that patients pre- senting with paranoid symptoms might be reluctant to involve family members of friends in the study); 4) Con- sent to have a summary of his/her results put in his/her personal medical file (facultative). All data were coded/ registered anonymously in the database. Material: Socio-demographics and medical data were first collected using a standard questionnaire on physical status, medical/family antecedents, current medications (dosages) and past investigations. This information was corroborated by the patient medical records (when con- sent obtained, see above). A semi-structured interview designed to investigate the current and past psychiatric symptoms was afterwards administered. This interview was based on the Scale for the Assessment of Positive Symptoms (SAPS) [32], and the Scale for the Assess- ment of Negative Symptoms (SANS) [33]. Each symp- tom was scored using a Likert scale (from 0 = absence to 4 = very important) reflecting the severity of each symp- tom. Statistical analyses: Descriptive and univariate analy- ses were performed to compare some socio-demo- graphics and present/past symptom profile of VLOSLP and EOS. Chi-square and Fisher’s exact test were con- ducted to compare categorical variables. Independent t- tests were used to compare continuous variables. Analy- ses were performed using SPSS for Windows version 17. This was an analytical study and thus multiple compari- sons were made. An alpha of p < 0.05 was applied to the socio-demographic (Table 1), medical (Table 2) and primary variables (Table 3) which were the general scores obtained on the SAPS/SANS (see Table 3). Only the variables found significant on these general scores were further analysed to specify the symptoms’ typology. A Bonferroni correction was applied to these results in order to avoid the type I error. As a result, an alpha of p ≤ 0.001 was determined. In addition, Effect sizes (d) [40], were calculated on all descriptive data of Tables 3-5 with the following interpretation per Cohen [40]: d = Copyright © 2012 SciRes. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 Copyright © 2012 SciRes. 308 OPEN ACCESS Table 1. Socio-demographic data. Variables Total sample (N = 34) VLOSLP (n = 17) EOS (n = 17) T-test Chi-square Gender (Female/Male) 24/10 13/4 11/6 - 0.452 Age at evaluation (years) 70.9 (8.8) Range: 50 - 84 76.3 (4.2) 65.5 (9.1) <0.001* Age at first symptoms (years) 50.9 (22.9) Range: 17 - 84 71.2 (5.6) 27.9 (7.4) <0.001* - Age at diagnosis (years) 52.8 (22.8) Range: 17 - 81 73.1 (5.3) 29.9 (7.3) <0.001* - Remission index 1(years) 2.8 (3.5) 5.1 (5.9) 0.176 - Disease duration (years) 19.9 (17.1) 5.3 (5.2) 36.4 (8.1) <0.001* - Diagnosis SZ: Szophreniform dis.: Delusional dis.: NS psychotic dis.: Paraphrenia: 17 2 6 7 2 2 6 7 2 17 - <0.001* Education (years) 9.88 (4.15) Range: 4 - 21 7.47 (2.09) 12.29 (4.33) <0.001* - Civil status Single: Married: Divorced: Widowed: 14 7 6 7 3 5 2 7 11 2 4 0 - 0.004* Number of children 1.76 (2.22) Range: 0 - 7 2.94 (2.54) 0.59 (0.87) 0.002* - 1Number of years between last episode and evaluation; Legend: VLOSLP: Very Late-Onset Schizophrenia-Like Psychosis; EOS: Early-Onset Schizophrenia; SZ: Schizophrenia; Szophreniform dis.: Schizophreniform disorder; Delusional dis.: Delusional disorder; NS psychotic dis.: Non-specific psychotic disorder. *p < 0.05. Table 2. Medical data from medical records. Variables Total sample (N = 34) VLOSLP (n = 17) EOS (n = 16) Chi-square Fisher exact test Positive family history Schizophrenia 10/30 2/16 8/14 0.010 0.019 Psychiatric disorders 18/29 7/16 11/13 0.024 0.052 Dementia 7/31 5/16 2/15 0.233 0.394 Current medication Typical neuroleptics 12/34 2/17 10/16 0.004 0.010* Atypical neuroleptics 30/34 16/17 14/16 0.287 0.601 Benzodiazepines 24/33 9/16 15/16 0.039 0.057 Antidepressants 14/34 8/17 6/16 0.486 0.728 Mood stabilizers 3/34 1/17 2/16 0.545 1.000 Anti-parkinsonian agents 9/34 1/17 8/16 0.007 0.017 Nootropics 0/34 0/17 0/16 - - Medical condition High blood pressure 18/33 12/16 6/16 0.022 0.037 Diabetes 10/33 4/16 6/16 0.520 0.708 Dyslipidemia/hypercholesterolemia 15/33 7/16 8/16 0.849 1.000 Cardiac condition 13/34 7/17 6/16 0.724 1.000 Smoking 6/34 3/17 3/16 1.000 1.000 Obesity 9/29 5/16 4/13 0.978 1.000 Hypothyroidia 8/33 3/16 5/16 0.475 0.688  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 309 Continued CT-Scan results Abnormalities at CT-Scan 13/22 11/16 2/6 0.132 0.178 Positive personality trait/disorder - Paranoid - Schizotypic - Passive-dependant - Obsessive - Mixte 13/34 2 2 3 3 3 7/17 2 0 2 2 1 6/16 0 2 1 1 2 0.410 Current anxiety symptoms 5/34 4/17 1/16 0.146 0.335 Past anxiety symptoms 27/32 13/17 14/15 0.190 0.338 Current depressive symptoms 2/34 2/17 0/16 0.145 0.485 Past depressive symptoms 22/32 11/17 11/15 0.599 0.712 Legend: VLOSLP: Very Late-Onset Schizophrenia-Like Psychosis; EOS: Early-Onset Schizophrenia; Note: Access to medical files for 17 VLOSLP and 16 EOS. *p < 0.05. Table 3. General psychiatric profile. VLOSLP ( n = 17) Mean (SD) EOS (n = 17) Mean (SD) Effect size (d) T-test (p) Number of hallucinations (/7)0.75 (1.18) 0.82 (0.95) 0.07 0.845 Number of delusions (/20) 1.06 (1.39) 2.94 (3.47) 0.77 0.059 Number of behavioral disturbances (/4) 0.19 (0.54) 0.59 (0.71) 0.64 0.078 SAPS Number of formal thought disorders (/8) 0.75 (1.57) 0.47 (0.94) 0.22 0.537 Number of affective poverty symptoms (/7) 1.56 (1.83) 2.76 (2.56) 0.55 0.133 Number of alogia symptoms (/5) 0.88 (1.59) 1.06 (1.35) 0.12 0.721 Number of apathy symptoms (/3) 1.19 (1.17) 1.00 (1.00) 0.18 0.623 Current condition SANS Number of anhedonia symptoms (/4) 2.19 (1.52) 2.76 (1.39) 0.39 0.263 Number of hallucinations (/7)2.06 (1.52) 3.94 (1.44) 1.27 0.001* Number of delusions (/20) 2.65 (1.62) 7.06 (3.13) 1.86 <0.001* Number of behavioral disturbances (/4) 1.47 (0.94) 2.47 (0.87) 1.11 0.003* SAPS Number of formal thought disorders (/8) 1.53 (1.97) 2.43 (2.28) 0.42 0.248 Number of affective poverty symptoms (/7) 1.24 (1.89) 2.00 (1.63) 0.43 0.224 Number of alogia symptoms (/5) 0.76 (1.15) 1.21 (1.25) 0.38 0.306 Number of apathy symptoms (/3) 1.24 (1.20) 2.18 (0.64) 1.02 0.009* At onset/Past condition SANS Number of anhedonia symptoms (/4) 2.94 (0.66) 3.65 (0.61) 1.12 0.003* Legend: SAPS: Scale for the Assessment of Positive Symptoms; SANS: Scale for the Assessment of Negative Symptoms; VLOSLP: Very Late-Onset Schizo- phrenia-Like Psychosis; EOS: Early-Onset Schizophrenia. *p < 0.05. Copyright © 2012 SciRes. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 310 Table 4. Positive symptoms. Variables VLOSLP (n = 17) Ratio1 SAPS EOS (n = 17) Ratio SAPSES (d) T-test (p) Mean (SD) Mean (SD) Hallucinations Current Past 5/16 15/17 8/17 16/16 Auditory Current Past 5/16 14/17 1.12 (1.73) 3.12 (1.54) 7/17 15/16 0.82 (1.07) 3.24 (1.30) 0.21 0.09 - 0.811 Commenting voices Current Past 1/15 5/17 0.35 (1.00) 1.18 (1.88) 2/16 11/15 0.29 (0.69) 2.59 (1.77) 0.07 0.77 - 0.031 Conversing voices Current Past 1/15 4/17 0.35 (1.00) 0.94 (1.75) 0/17 6/15 - 1.47 (1.84) - 0.29 - 0.396 Ordering voices Current Past 2/16 4/17 0.35 (1.00) 0.76 (1.56) 1/17 9/16 0.12 (0.49) 2.12 (1.97) 0.31 0.77 - 0.034 Somatic Current Past 2/15 1/17 0.53 (1.18) 0.24 (0.97) 2/17 9/16 0.41 (1.18) 1.71 (1.76) 0.10 1.08 - 0.006 Olfactive/Gustative Current Past 0/16 2/17 0.06 (0.24) 0.41 (1.18) 0/16 2/16 0.06 (0.24) 0.41 (1.00) 0.00 0.00 - 1.000 Visual Current Past 1/15 5/17 0.35 (1.00) 0.94 (1.64) 2/16 11/16 0.29 (0.69) 2.24 (1.72) 0.07 0.77 - 0.031 Delusions Current Past 8/16 16/17 11/16 17/17 Persecutory Current Past 6/16 15/17 1.12 (1.54) 3.29 (1.45) 5/16 16/16 0.71 (1.16) 3.82 (0.73) 0.30 0.49 - 0.191 Jealousy Current Past 0/16 5/17 0.06 (0.24) 0.88 (1.58) 0/17 1/16 - 0.29 (0.99) - 0.46 - 0.203 Sexual/Erotomaniac Current Past 2/16 5/17 0.41 (1.06) 1.12 (1.80) 2/17 6/16 0.47 (1.33) 1.24 (1.68) 0.05 0.07 - 0.845 Culpability Current Past 0/16 0/17 0.06 (0.24) - 2/16 5/17 0.41 (1.00) 1.00 (1.73) 0.57 - - 0.030 Grandiosity Current Past 1/16 1/16 0.18 (0.53) 0.24 (0.97) 5/17 10/16 0.82 (1.38) 2.18 (1.85) 0.67 1.38 - 0.001* Catastrophic Current Past 0/16 0/17 0.06 (0.24) - 2/17 7/17 0.41 (1.18) 1.59 (1.97) 0.49 - - 0.004 Mystic/religious Current Past 0/16 3/17 0.06 (0.24) 0.24 (0.56) 4/16 8/15 0.65 (1.22) 1.82 (1.81) 0.81 1.33 - 0.003 Somatic Current Past 2/16 2/16 0.47 (1.18) 0.29 (0.77) 2/16 4/15 0.47 (1.18) 1.24 (1.75) 0.00 0.75 - 0.055 Reference Current Past 3/16 6/16 0.65 (1.32) 1.35 (1.84) 6/14 16/17 1.24 (1.48) 3.47 (1.01) 0.42 1.49 - <0.001* Influence Current Past 1/16 1/17 0.24 (0.75) 0.18 (0.73) 2/16 9/16 0.41 (1.06) 2.00 (1.87) 0.19 1.40 - 0.001* Thought reading Current Past 1/16 0/17 0.12 (0.33) - 2/16 6/16 0.35 (0.86) 1.35 (1.80) 0.39 - - 0.007 Thought diffusion Current Past 1/16 1/16 0.18 (0.53) 0.29 (0.99) 7/17 8/15 1.12 (1.50) 1.88 (1.87) 0.93 1.11 - 0.005 Thought imposition Current Past 0/16 0/17 0.06 (0.24) - 2/17 5/16 0.29 (0.85) 1.06 (1.60) 0.42 - - 0.015 Behavioral disturbances Current Past 2/16 14/17 8/17 17/17 Bizarre presentation Current Past 0/17 1/17 - 0.24 (0.97) 4/17 5/16 0.65 (1.22) 0.82 (1.24) - 0.53 - 0.133 Inappropriate social and/or sexual conducts Current Past 2/16 12/17 0.35 (0.86) 2.29 (1.65) 2/17 12/15 0.18 (0.53) 2.47 (1.63) 0.25 0.11 - 0.755 Agressive and/or agitated behaviour Current Past 1/16 9/17 0.18 (0.53) 1.88 (1.87) 0/17 16/17 - 3.06 (1.09) - 0.79 - 0.034 Repetitive/Stereotyped behaviour Current Past 0/16 3/17 0.06 (0.24) 0.47 (1.13) 4/16 9/15 0.47 (0.80) 1.59 (1.37) 0.79 0.89 - 0.014 Formal thought disorders Current Past 4/16 8/17 4/17 9/14 Loosening of associations Current Past 2/16 7/17 0.41 (1.00) 1.41 (1.81) 4/17 8/14 0.53 (1.01) 1.94 (1.82) 0.12 0.29 - - Tangentiality Current Past 3/16 7/17 0.53 (1.07) 1.29 (1.65) 1/17 8/14 0.12 (0.49) 1.82 (1.70) 0.53 0.32 - - Copyright © 2012 SciRes. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 311 Continued Incoherence Current Past 1/16 1/17 0.18 (0.53) 0.18 (0.73) 0/17 2/14 - 0.53 (1.07) - 0.39 - - Illogical speech Current Past 1/16 2/17 0.12 (0.33) 0.29 (0.85) 0/17 3/14 - 0.88 (1.54) - 0.49 - - Circumstantial speech Current Past 2/16 5/17 0.47 (1.18) 0.88 (1.45) 3/17 7/14 0.47 (1.07) 1.65 (1.73) 0.00 0.48 - - Logorrhea Current Past 1/16 2/17 0.24 (0.75) 0.35 (1.00) 0/17 4/14 - 0.82 (1.24) - 0.42 - - 1Ratio refers to the proportion of patients presenting this symptom. Legends: VLOSLP: Very Late-Onset Schizophrenia-Like Psychosis; EOS: Early-Onset Schi- zophrenia; ES = Effect Size; SD = Standard Deviation. *p < 0.001. Table 5. Negative symptoms. Variables VLOSLP (n = 17) Ratio1 SANS EOS (n = 17) Ratio SANS ES (d) T-test (p) Mean (SD) Mean (SD) Affective poverty Current Past 8/16 7/17 11/17 12/16 Restricted face expression Current Past 6/16 6/17 0.88 (1.17) 1.06 (1.52) 10/17 7/15 1.47 (1.33) 1.47 (1.63) 0.47 0.26 - - Gesture poverty Current Past 4/16 2/17 0.59 (1.06) 0.29 (0.85) 7/17 1/14 0.88 (1.11) 0.35 (0.79) 0.27 0.07 - - Visual contact poverty Current Past 1/16 1/17 0.18 (0.53) 0.18 (0.73) 4/17 3/15 0.59 (1.18) 0.65 (1.22) 0.48 0.48 - - Reduced emotional reactivity Current Past 7/16 7/17 1.12 (1.36) 1.47 (1.84) 11/17 12/15 1.88 (1.58) 2.88 (1.69) 0.52 0.79 - - Inappropriate affect Current Past 1/16 2/17 0.18 (0.53) 0.35 (1.06) 3/17 7/15 0.41 (0.94) 1.76 (1.95) 0.31 0.94 - - Voice monotony Current Past 3/16 1/17 0.41 (0.80) 0.18 (0.73) 6/17 0/14 0.82 (1.19) 0.18 (0.39) 0.41 0.00 - - Alogia Current Past 5/16 6/17 8/17 8/14 Speech poverty Current Past 5/16 5/17 0.88 (1.32) 0.94 (1.52) 5/17 6/14 0.65 (1.06) 1.18 (1.33) 0.19 0.17 - - Speech content poverty Current Past 4/16 5/17 0.82 (1.43) 1.00 (1.62) 4/17 4/14 0.65 (1.22) 0.88 (1.27) 0.13 0.08 - - Speech freezing Current Past 2/16 3/17 0.41 (1.00) 0.47 (1.07) 4/17 4/13 0.47 (0.87) 0.94 (1.25) 0.06 0.41 - - Apathy Current Past 10/16 11/17 10/17 17/17 Presentation and personal hygiene neglected Current Past 4/16 4/16 0.76 (1.35) 0.82 (1.47) 1/17 6/17 0.18 (0.73) 0.88 (1.36) 0.56 0.04 - 0.904 Assiduity loss Current Past 5/16 9/17 1.12 (1.76) 1.65 (1.69) 8/17 17/17 1.35 (1.58) 3.59 (0.51) 0.14 1.71 - <0.001* Physical anergia Current Past 10/16 8/16 1.65 (1.41) 1.53 (1.63) 8/17 14/16 1.35 (1.58) 2.94 (1.34) 0.20 0.95 - 0.010 Anhedonia Current Past 13/16 17/17 15/17 17/17 Restricted interests and hobbies Current Past 10/16 14/15 1.94 (1.68) 2.82 (1.19) 10/17 17/17 1.59 (1.54) 3.53 (0.51) 0.22 0.84 - 0.031 Incapacity with intimate relations Current Past 7/15 14/17 1.47 (1.66) 2.76 (1.48) 13/17 17/17 2.47 (1.55) - 0.62 - - 0.005 Friendship poverty Current Past 12/16 15/16 2.53 (1.74) 3.29 (1.26) 13/17 16/17 3.94 (0.24) 3.71 (0.99) 1.42 0.37 - 0.297 1Ratio refers to the proportion of patients presenting this symptom. Legends: VLOSLP: Very Late-Onset Schizophrenia-Like Psychosis; EOS: Early-Onset Schi- zophrenia; ES = Effect Size; SD = Standard Deviation. *p < 0.001. Copyright © 2012 SciRes. OPEN ACCESS 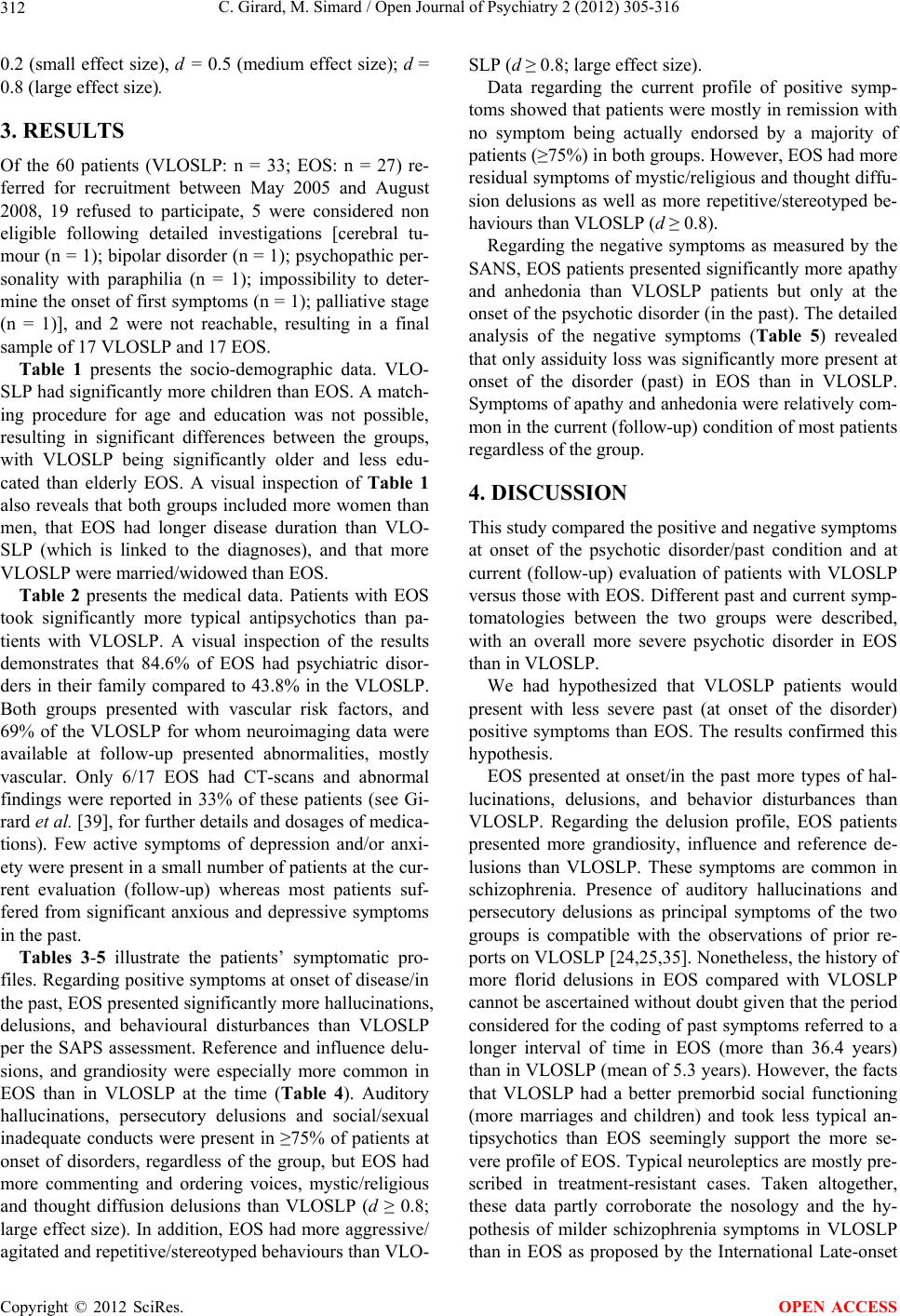 C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 Copyright © 2012 SciRes. 312 OPEN ACCESS 0.2 (small effect size), d = 0.5 (medium effect size); d = 0.8 (large effect size). 3. RESULTS Of the 60 patients (VLOSLP: n = 33; EOS: n = 27) re- ferred for recruitment between May 2005 and August 2008, 19 refused to participate, 5 were considered non eligible following detailed investigations [cerebral tu- mour (n = 1); bipolar disorder (n = 1); psychopathic per- sonality with paraphilia (n = 1); impossibility to deter- mine the onset of first symptoms (n = 1); palliative stage (n = 1)], and 2 were not reachable, resulting in a final sample of 17 VLOSLP and 17 EOS. Table 1 presents the socio-demographic data. VLO- SLP had significantly more children than EOS. A match- ing procedure for age and education was not possible, resulting in significant differences between the groups, with VLOSLP being significantly older and less edu- cated than elderly EOS. A visual inspection of Table 1 also reveals that both groups included more women than men, that EOS had longer disease duration than VLO- SLP (which is linked to the diagnoses), and that more VLOSLP were married/widowed than EOS. Table 2 presents the medical data. Patients with EOS took significantly more typical antipsychotics than pa- tients with VLOSLP. A visual inspection of the results demonstrates that 84.6% of EOS had psychiatric disor- ders in their family compared to 43.8% in the VLOSLP. Both groups presented with vascular risk factors, and 69% of the VLOSLP for whom neuroimaging data were available at follow-up presented abnormalities, mostly vascular. Only 6/17 EOS had CT-scans and abnormal findings were reported in 33% of these patients (see Gi- rard et al. [39], for further details and dosages of medica- tions). Few active symptoms of depression and/or anxi- ety were present in a small number of patients at the cur- rent evaluation (follow-up) whereas most patients suf- fered from significant anxious and depressive symptoms in the past. Tables 3-5 illustrate the patients’ symptomatic pro- files. Regarding positive symptoms at onset of disease/in the past, EOS presented significantly more hallucinations, delusions, and behavioural disturbances than VLOSLP per the SAPS assessment. Reference and influence delu- sions, and grandiosity were especially more common in EOS than in VLOSLP at the time (Table 4). Auditory hallucinations, persecutory delusions and social/sexual inadequate conducts were present in ≥75% of patients at onset of disorders, regardless of the group, but EOS had more commenting and ordering voices, mystic/religious and thought diffusion delusions than VLOSLP (d ≥ 0.8; large effect size). In addition, EOS had more aggressive/ agitated and repetitive/stereotyped behaviours than VLO- SLP (d ≥ 0.8; large effect size). Data regarding the current profile of positive symp- toms showed that patients were mostly in remission with no symptom being actually endorsed by a majority of patients (≥75%) in both groups. However, EOS had more residual symptoms of mystic/religious and thought diffu- sion delusions as well as more repetitive/stereotyped be- haviours than VLOSLP (d ≥ 0.8). Regarding the negative symptoms as measured by the SANS, EOS patients presented significantly more apathy and anhedonia than VLOSLP patients but only at the onset of the psychotic disorder (in the past). The detailed analysis of the negative symptoms (Table 5) revealed that only assiduity loss was significantly more present at onset of the disorder (past) in EOS than in VLOSLP. Symptoms of apathy and anhedonia were relatively com- mon in the current (follow-up) condition of most patients regardless of the group. 4. DISCUSSION This study compared the positive and negative symptoms at onset of the psychotic disorder/past condition and at current (follow-up) evaluation of patients with VLOSLP versus those with EOS. Different past and current symp- tomatologies between the two groups were described, with an overall more severe psychotic disorder in EOS than in VLOSLP. We had hypothesized that VLOSLP patients would present with less severe past (at onset of the disorder) positive symptoms than EOS. The results confirmed this hypothesis. EOS presented at onset/in the past more types of hal- lucinations, delusions, and behavior disturbances than VLOSLP. Regarding the delusion profile, EOS patients presented more grandiosity, influence and reference de- lusions than VLOSLP. These symptoms are common in schizophrenia. Presence of auditory hallucinations and persecutory delusions as principal symptoms of the two groups is compatible with the observations of prior re- ports on VLOSLP [24,25,35]. Nonetheless, the history of more florid delusions in EOS compared with VLOSLP cannot be ascertained without doubt given that the period considered for the coding of past symptoms referred to a longer interval of time in EOS (more than 36.4 years) than in VLOSLP (mean of 5.3 years). However, the facts that VLOSLP had a better premorbid social functioning (more marriages and children) and took less typical an- tipsychotics than EOS seemingly support the more se- vere profile of EOS. Typical neuroleptics are mostly pre- scribed in treatment-resistant cases. Taken altogether, these data partly corroborate the nosology and the hy- pothesis of milder schizophrenia symptoms in VLOSLP than in EOS as proposed by the International Late-onset 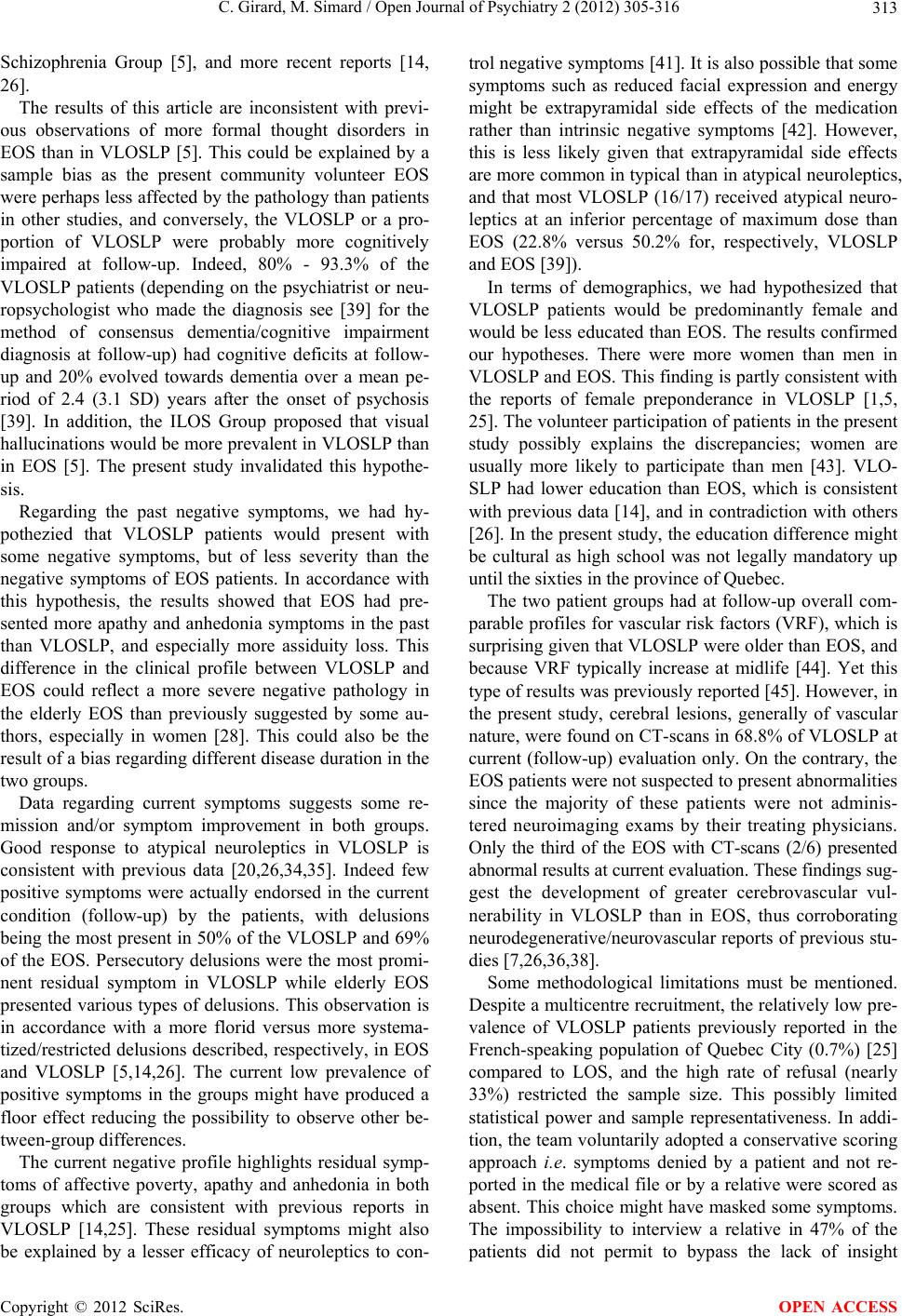 C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 313 Schizophrenia Group [5], and more recent reports [14, 26]. The results of this article are inconsistent with previ- ous observations of more formal thought disorders in EOS than in VLOSLP [5]. This could be explained by a sample bias as the present community volunteer EOS were perhaps less affected by the pathology than patients in other studies, and conversely, the VLOSLP or a pro- portion of VLOSLP were probably more cognitively impaired at follow-up. Indeed, 80% - 93.3% of the VLOSLP patients (depending on the psychiatrist or neu- ropsychologist who made the diagnosis see [39] for the method of consensus dementia/cognitive impairment diagnosis at follow-up) had cognitive deficits at follow- up and 20% evolved towards dementia over a mean pe- riod of 2.4 (3.1 SD) years after the onset of psychosis [39]. In addition, the ILOS Group proposed that visual hallucinations would be more prevalent in VLOSLP than in EOS [5]. The present study invalidated this hypothe- sis. Regarding the past negative symptoms, we had hy- pothezied that VLOSLP patients would present with some negative symptoms, but of less severity than the negative symptoms of EOS patients. In accordance with this hypothesis, the results showed that EOS had pre- sented more apathy and anhedonia symptoms in the past than VLOSLP, and especially more assiduity loss. This difference in the clinical profile between VLOSLP and EOS could reflect a more severe negative pathology in the elderly EOS than previously suggested by some au- thors, especially in women [28]. This could also be the result of a bias regarding different disease duration in the two groups. Data regarding current symptoms suggests some re- mission and/or symptom improvement in both groups. Good response to atypical neuroleptics in VLOSLP is consistent with previous data [20,26,34,35]. Indeed few positive symptoms were actually endorsed in the current condition (follow-up) by the patients, with delusions being the most present in 50% of the VLOSLP and 69% of the EOS. Persecutory delusions were the most promi- nent residual symptom in VLOSLP while elderly EOS presented various types of delusions. This observation is in accordance with a more florid versus more systema- tized/restricted delusions described, respectively, in EOS and VLOSLP [5,14,26]. The current low prevalence of positive symptoms in the groups might have produced a floor effect reducing the possibility to observe other be- tween-group differences. The current negative profile highlights residual symp- toms of affective poverty, apathy and anhedonia in both groups which are consistent with previous reports in VLOSLP [14,25]. These residual symptoms might also be explained by a lesser efficacy of neuroleptics to con- trol negative symptoms [41]. It is also possible that some symptoms such as reduced facial expression and energy might be extrapyramidal side effects of the medication rather than intrinsic negative symptoms [42]. However, this is less likely given that extrapyramidal side effects are more common in typical than in atypical neuroleptics, and that most VLOSLP (16/17) received atypical neuro- leptics at an inferior percentage of maximum dose than EOS (22.8% versus 50.2% for, respectively, VLOSLP and EOS [39]). In terms of demographics, we had hypothesized that VLOSLP patients would be predominantly female and would be less educated than EOS. The results confirmed our hypotheses. There were more women than men in VLOSLP and EOS. This finding is partly consistent with the reports of female preponderance in VLOSLP [1,5, 25]. The volunteer participation of patients in the present study possibly explains the discrepancies; women are usually more likely to participate than men [43]. VLO- SLP had lower education than EOS, which is consistent with previous data [14], and in contradiction with others [26]. In the present study, the education difference might be cultural as high school was not legally mandatory up until the sixties in the province of Quebec. The two patient groups had at follow-up overall com- parable profiles for vascular risk factors (VRF), which is surprising given that VLOSLP were older than EOS, and because VRF typically increase at midlife [44]. Yet this type of results was previously reported [45]. However, in the present study, cerebral lesions, generally of vascular nature, were found on CT-scans in 68.8% of VLOSLP at current (follow-up) evaluation only. On the contrary, the EOS patients were not suspected to present abnormalities since the majority of these patients were not adminis- tered neuroimaging exams by their treating physicians. Only the third of the EOS with CT-scans (2/6) presented abnormal results at current evaluation. These findings sug- gest the development of greater cerebrovascular vul- nerability in VLOSLP than in EOS, thus corroborating neurodegenerative/neurovascular reports of previous stu- dies [7,26,36,38]. Some methodological limitations must be mentioned. Despite a multicentre recruitment, the relatively low pre- valence of VLOSLP patients previously reported in the French-speaking population of Quebec City (0.7%) [25] compared to LOS, and the high rate of refusal (nearly 33%) restricted the sample size. This possibly limited statistical power and sample representativeness. In addi- tion, the team voluntarily adopted a conservative scoring approach i.e. symptoms denied by a patient and not re- ported in the medical file or by a relative were scored as absent. This choice might have masked some symptoms. The impossibility to interview a relative in 47% of the patients did not permit to bypass the lack of insight Copyright © 2012 SciRes. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 314 commonly mentioned in schizophrenia [46] and in late paraphrenia [47]; thus some symptoms might have been missed. The SAPS/SANS were completed by a single rater, which ensured the consistency of ratings, but could have introduced a bias in scoring if the rater had preconcep- tions. The absence of inter-rater procedure must also be mentioned since there was variability in the details of medical records filled by different physicians at onset of the disorders. This might be explained by the fact that patients were recruited in several settings. This short- coming is characteristic of historical cohorts. Further- more, negative symptoms could have been difficult to distinguish from the confounding effects of depression, medications, institutionalization, poverty, etc. [48]. Finally, inconsistency regarding the onset of disease and group composition must be considered. Indeed, the onset of symptoms was preferentially defined as the mo- ment symptoms were first noticed by the patient/family member. When this information was unavailable, onset was defined as the time of diagnosis. However, this me- thod is less reliable; first signs of psychosis may arise many years before the diagnosis. This may have resulted by the inclusion in the VLOSLP group of some patients presenting first psychotic symptoms before the age of 40 years old, although the mean old age at diagnosis (mean = 73.1 ± 5.3 years) makes this hypothesis unlikely. Al- ternatively, it is possible that patients who presented cerebral abnormalities at follow-up were in fact suffering from some prior cerebral dysfunction that was unrecog- nized at the onset of psychotic symptoms or masked by the presence of psychotic symptoms. Despite these limitations, this study provided impor- tant data on the current and past symptomatic presenta- tion of VLOSLP in a French-speaking population living in the community. 5. ACKNOWLEDGEMENTS The authors wish to thank Drs. Robert Noiseux, François Primeau, Nicole Robert, Michel Dugas, François Rousseau, Nadine Gagnon, Evelyn Keller and Patrick Bernier for kindly referring the patients. This work was supported by doctoral awards (C.G.) from Réseau Qué- bécois de Recherche sur le Vieillissement, Fonds de la Recherche en Santé du Québec, and Fondation de l’Université Laval (Bourse Hydro Québec), and by a 2005 NARSAD Young Investigator Award (M.S). Parts of this article were presented at the 2nd Schizophrenia Interna- tional Research Society Conference, Firenze, Italy, April 10-14th, 2010. REFERENCES [1] Meesters, P.D., et al. (2012) Schizophrenia spectrum disorders in later life: Prevalence and distribution of age at onset and sex in a Dutch catchment area. American Journal of Geriatric Psychiatry, 20, 18-28. doi:10.1097/JGP.0b013e3182011b7f [2] Mitford, E., Reay, R., McCabe, K., Paxton, R. and Turk- ington, D. (2010) Ageism in first episode psychosis. In- ternational Journal of Geriatric Psychiatry, 25, 1112- 1118. doi:10.1002/gps.2437 [3] Reeves, R.R. and Brister, J.C. (2008) Psychosis in Late life: Emerging issues. Journal of Psychosocial Nursing, 46, 45-52. [4] Bartels, S.J., Clark, R.E., Peacock, W.J., Dums, A.R. and Pratt, S.I. (2003) Medicare and medicaid costs for schi- zophrenia patients by age cohort compared with costs for depression, dementia, and medically ill patients. Ameri- can Journal of Geriatric Psychiatry, 11, 648-657. [5] Howard, R., Rabins, P.V., Seeman, M.V., Jeste, D.V. and the International Late-Onset Schizophrenia Group (2000) Late-onset schizophrenia and very-late-onset schizophre- nia-like psychosis: An international consensus. American Journal of Psychiatry, 157, 172-178. doi:10.1176/appi.ajp.157.2.172 [6] Pearman, A. and Batra, A. (2012) Late-onset schizoph- renia: A review for clinicians. Clinical Gerontologist, 35, 126-147. doi:10.1080/07317115.2011.642943 [7] Lagodka, A. and Robert, P. (2009) Is late-onset schizoph- renia related to neurodegenerative process? A review of the literature. L’Encéphale, 35, 386-393. doi:10.1016/j.encep.2008.06.008 [8] Howard, R., Castle, D., Wessely, S. and Murray, R.M. (1993) A comparative study of 470 cases of early- and late-onset schizophrenia. British Journal of Psychiatry, 163, 352-357. doi:10.1192/bjp.163.3.352 [9] Jeste, D.V., Harris, M.J., Krull, A., Kuck, J., McAdams, L.A. and Heaton, R. (1995) Clinical and neuropsycho- logical characteristics of patients with late-onset schizoph- renia. American Journal of Psychiatry, 152, 722-730. [10] Palmer, B.W., Bondi, M.W., Twamley, E.W., Thal, L., Golshan, S. and Jeste, D.V. (2003) Are late-onset schi- zophrenia spectrum disorders neurodegenerative condi- tions? Annual rates of change on two measures. Journal of Neuropsychiatry and Clinical Neurosciences, 15, 45- 52. doi:10.1176/appi.neuropsych.15.1.45 [11] Sato, T., Bottlender, R., Schröter, A. and Moller, H.J. (2004) Psychopathology of early-onset versus late-onset schizophrenia revisited: An observation of 473 neuroleptic- naïve patients before and after first-admission treatments. Schizophrenia Research, 67, 175-183. doi:10.1016/S0920-9964(03)00015-X [12] Huang, C. and Zhang, Y. (2009) Clinical differences be- tween late-onset and early-onset chronically hospitalized elderly schizophrenic patients in Taiwan. International Journal of Geriatric Psychiatry, 24, 1166-1172. doi:10.1002/gps.2241 [13] Köhler, S., van Os, J., de Graaf, R., Vollebergh, W., Verhey, F. and Krabbendam, L. (2007) Psychosis risk as a function of age at onset: A comparison between early- and late-onset psychosis in a general population sample. Social Psychiatry and Psychiatric Epidemiology, 42, 288- 294. doi:10.1007/s00127-007-0171-6 [14] Köhler, S., et al. (2009) Evidence that better outcome of Copyright © 2012 SciRes. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 315 psychosis in women is reversed with increasing age at onset: A population-based 5-year follow-up study. Schi- zophrenia Research, 113, 226-232. doi:10.1016/j.schres.2009.05.017 [15] Vahia, I.V., Palmer, B.W., Depp, C., Fellows, I., Golshan, S., Kraemer, H.C. and Jeste, D.V. (2010) Is late-onset schizophrenia a subtype of schizophrenia? Acta Psychi- atrica Scandinavia, 122, 414-426. doi:10.1111/ j.1600-0447.2010.01552.x [16] Riecher-Rössler, A., Häfner, H., Häfner-Ranabauer, W., Löffler, W. and Reinhard, I. (2003) Late-onset schizo- phrenia versus paranoid psychoses: A valid diagnostic Distinction? American Journal of Geriatric Psychiatry, 11, 595-604. [17] Brunelle, S., Cole, M.G. and Elie, M. (2011) Risk factors for late-onset psychoses: A systematic review of cohort studies. International Journal of Geriatric Psychiatry, 27, 240-252. doi:10.1002/gps.2702 [18] Hassett, A. (1999) A descriptive study of first presen- tation psychosis in old age. Australian and New Zealand Journal of Psychiatry, 33, 814-824. doi:10.1046/j.1440-1614.1999.00651.x [19] Quin, R.C., Clare, L., Ryan, P. and Jackson, M. (2009) Not of this world: The subjective experience of late-onset psychosis. Aging and Mental Health, 13, 779-787. doi:10.1080/13607860903046453 [20] Reeves, S., Stewart, R. and Howard, R. (2002) Service contact and psychopathology in very-late-onset schizoph- renia-like psychosis: The effects of gender and ethnicity. International Journal of Geriat ric Psychiat ry, 17, 473- 479. doi:10.1002/gps.614 [21] Reeves, S., Hudson, S., Fletcher, H., Sauer, J., Stewart, R. and Howard, R. (2003) Are black Caribbean patients like- ly to receive an incorrect diagnosis of very-late-onset schizophrenia-like psychosis than their white British coun- terparts? American Journal of Geriatric Psychiatry, 11, 674-677. [22] Romero-Rubiales, F., Reeves, S. and Howard, R. (2004) Have risk factors for very-late-onset schizophrenia-like psychosis changed in the last 40 years? International Journal of Geriatric Psychiatry, 19, 803-807. doi:10.1002/gps.1152 [23] Mitter, P., Reeves, S., Romero-Rubiales, F., Bell, P., Ste- wart, R. and Howard, R. (2005) Migrant status, age, gen- der and social isolation in very late-onset schizophrenia- like psychosis. International Journal of Geriatric Psy- chiatry, 20, 1046-1051. doi:10.1002/gps.1396 [24] Alici-Evcimen, Y., Ertan, T. and Eker, E. (2003) Case series with late-onset psychosis hospitalized in geriatric psychiatry unit in Turkey: Experience in 9 years. Inter- national Psychogeria tri cs , 15, 69-72. doi:10.1017/S1041610203008767 [25] Girard, C. and Simard, M. (2008) Clinical characteriza- tion of late- and very-late-onset first psychotic episode in psychiatric inpatients. American Journal of Geriatric Psy- chiatry, 16, 478-487. doi:10.1097/JGP.0b013e31816c7b3c [26] Barak, Y., Aizenberg, D., Mirecki, I., Mazeh, D. and Achi- ron, A. (2002) Very late-onset schizophrenia-like psy- chosis: Clinical and imaging characteristics in compari- son with elderly patients with schizophrenia. Journal of Nervous Mental Disease, 190, 733-736. doi:10.1097/00005053-200211000-00002 [27] Arbus, C., Clement, J.-P., Bougerol, T., Fremont, P., Lan- crenon, S. and Camus, V. (2012) Health management of older persons with chronically medicated disorders: The results of a survey in France. International Psychogeriat- rics, 24, 496-502. doi:10.1017/S1041610211001487 [28] Häfner, H., Hambrecht, M., Löffler, W., Munk-Jorgensen, P. and Riecher-Rössler, A. (1998) Is schizophrenia a dis- order of all ages? A comparison of first episodes and early course across the life-cycle. Psychological Medicine, 28, 351-365. doi:10.1017/S0033291797006399 [29] Mazeh, D., Zemishani, C., Aizenberg, D. and Barak, Y. (2005) Patients with very-late-onset schizophrenia-like psychosis: A follow-up study. American Journal of Geri- atric Psychiatry, 13, 417-419. [30] Howard, R.J., et al. (1997) A controlled family study of late-onset non-affective psychosis (late paraphrenia). Bri- tish Journal of Psychiatry, 170, 511-514. doi:10.1192/bjp.170.6.511 [31] Bentall, R.P., et al. (2009) The cognitive and affective structure of paranoid delusions. Archives of General Psychiatry, 66, 236-247. doi:10.1001/archgenpsychiatry.2009.1 [32] Andreasen, N.C. (1984) Scale for the assessment of po- sitive symptoms (SAPS). University of Iowa, Iowa City. [33] Andreasen, N.C. (1983) Scale for the assessment of neg- ative symptoms (SANS) University of Iowa, Iowa City. [34] Psarros, C., Theleritis, C.G., Paparrigopoulos, T.J., Politis, A.M. and Papadimitriou, G.N. (2009) Amisulpride for the treatment of very-late-onset schizophrenia-like psychosis. International Journal of Geriatric Psychiatry, 24, 518- 522. doi:10.1002/gps.2146 [35] Scott, J., Greenwald, B.S., Kramer, E. and Shuwall, M. (2011) Atypical (second generation) antipsychotic treat- ment response in very late-onset schizophrenia-like psy- chosis. International Psychogeriatrics, 23, 742-748. doi:10.1017/S1041610210002188 [36] Brodaty, H., Sachdev, P., Koschera, A., Monk, D. and Cullen, B. (2003) Long-term outcome of late-onset schi- zophrenia: 5-year follow-up study. British Journal of Psy- chiatry, 183, 213-219. doi:10.1192/bjp.183.3.213 [37] Casanova, M.F., Stevens, J.R., Brown, R., Royston, C. and Bruton, C. (2002) Disentangling the pathology of schi- zophrenia and paraphrenia. Acta Neuropathologica, 103, 313-320. doi:10.1007/s00401-001-0468-6 [38] Tsujino, N., et al. (2011) Cerebral blood flow changes in very-late-onset schizophrenia-like psychosis with cata- tonia before and after successful treatment. Psychiatry and Clinical Neurosciences, 65, 600-603. doi:10.1111/ j.1440-1819.2011.02257.x [39] Girard, G., et al. (2011) Late-onset-psychosis: Cognition. International Psychogeriatrics, 23, 1301-1306. doi:10.1017/S1041610211000238 [40] Cohen, J. (1988) Statistical power analysis for the behav- ioral sciences. 2nd Edition, Lawrence Erlbaum Associates, Copyright © 2012 SciRes. OPEN ACCESS  C. Girard, M. Simard / Open Journal of Psychiatry 2 (2012) 305-316 Copyright © 2012 SciRes. 316 OPEN ACCESS Hillsdale. [41] Jockers-Scherübl, M.C., Bauer, A., Godemann, F., Reis- chies, F.M., Selig, F. and Schlattman, P. (2005) Negative symptoms of schizophrenia are improved by the addition of paroxetine to neuroleptics: A double-blind placebo con- trolled study. International Clinical Psychopharmacol- ogy, 20, 27-31. doi:10.1097/00004850-200501000-00006 [42] Gareri, P., De Fazio, P., De Fazio, S., Marigliano, N., Ferreri Ibbadu, G. and Sarro, G. (2006) Adverse effects of atypical antipsychotics in the elderly: A review. Drugs and Aging, 23, 937-956. doi:10.2165/00002512-200623120-00002 [43] Lee, S., Saito, T., Takahashi, M. and Kai, I. (2008) Vol- unteer participation among older adults in Japan: An analysis of participation and reasons for non-participation. Archives of Gerontology and Geriatry, 47, 173-187. doi:10.1016/j.archger.2007.08.004 [44] Wiederkehr, S., Simard, M., Fortin, C. and van Reekum, R. (2008) Validity of the clinical diagnostic criteria for vascular dementia: A critical review. Part II. The Journal of Neuropsychiatry and Clinical Neurosciences, 20, 162- 177. doi:10.1176/appi.neuropsych.20.2.162 [45] Sachdev, P., Brodaty, H., Rose, N. and Cathcart, S. (1999) Schizophrenia with onset after age 50 years. 2: Neuro- logical, neuropsychological and MRI investigation. Brit- ish Journal of Psychiatry, 175, 416-421. doi:10.1192/bjp.175.5.416 [46] Ostling, S., Borjesson-Hanson, A. and Skoog, I. (2007) Psychotic symptoms and paranoid ideation in a popula- tion-based sample of 95-year-olds. American Journal of Geriatric Psychiatry, 15, 999-1004. doi:10.1097/JGP.0b013e31814622b9 [47] Almeida, O., Levy, R., Howard, R.J. and David, A.S. (1996) Insight and paranoid disorders in late life (late paraphrenia). International Journal of Geriatric Psychi- atry, 11, 653-658. doi:10.1002/(SICI)1099-1166(199607)11:7<653::AID-G PS380>3.0.CO;2-9 [48] Howard, R. (2001) Late-onset schizophrenia and very late-onset schizophrenia-like psychosis. Review in Clini- cal Gerontology, 11, 337-352. doi:10.1017/S0959259801011455
|