Primary Cutaneous Diffuse Large B-Cell Lymphoma (Leg Type) Presenting as Necrotising Fasciitis 101
(a) (b)
(c)
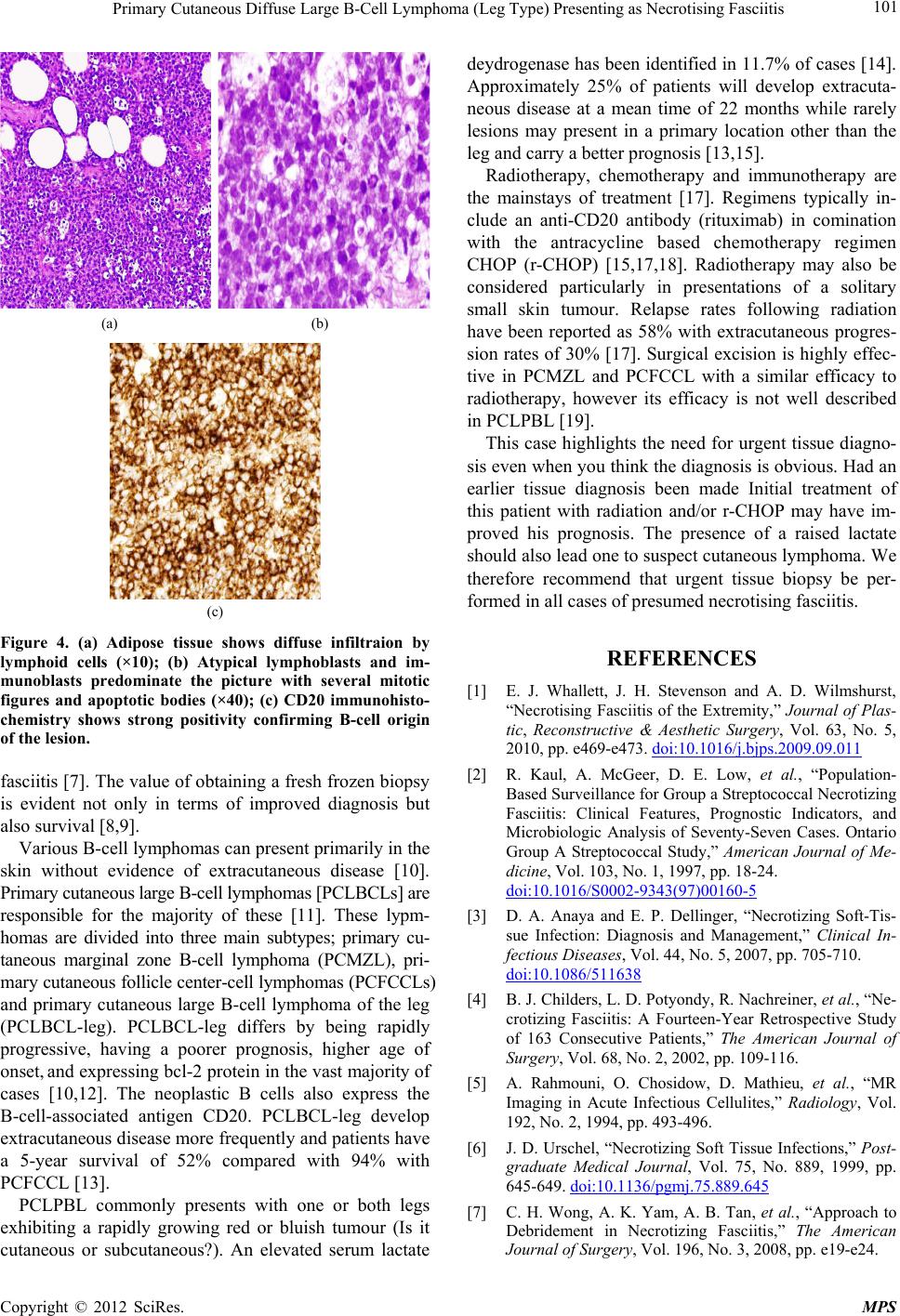
Figure 4. (a) Adipose tissue shows diffuse infiltraion by
lymphoid cells (×10); (b) Atypical lymphoblasts and im-
munoblasts predominate the picture with several mitotic
figures and apoptotic bodies (×40); (c) CD20 immunohisto-
chemistry shows strong positivity confirming B-cell origin
of the lesion.
fasciitis [7]. The va lue of obtaining a fresh frozen b iopsy
is evident not only in terms of improved diagnosis but
also survival [8,9].
Various B-cell lymphomas can present primarily in the
skin without evidence of extracutaneous disease [10].
Primary cutaneous large B-cell lymphomas [PCLBCLs] are
responsible for the majority of these [11]. These lypm-
homas are divided into three main subtypes; primary cu-
taneous marginal zone B-cell lymphoma (PCMZL), pri-
mary cutaneous follicle center-cell lymphomas (PCFCCLs)
and primary cutaneous large B-cell lymphoma of the leg
(PCLBCL-leg). PCLBCL-leg differs by being rapidly
progressive, having a poorer prognosis, higher age of
onset, and expressing bcl-2 protein in the vast majority of
cases [10,12]. The neoplastic B cells also express the
B-cell-associated antigen CD20. PCLBCL-leg develop
extracutaneous disease more frequently and patients have
a 5-year survival of 52% compared with 94% with
PCFCCL [13].
PCLPBL commonly presents with one or both legs
exhibiting a rapidly growing red or bluish tumour (Is it
cutaneous or subcutaneous?). An elevated serum lactate
deydrogenase has been identified in 11.7% of cases [14].
Approximately 25% of patients will develop extracuta-
neous disease at a mean time of 22 months while rarely
lesions may present in a primary location other than the
leg and carry a better prognosis [13,15].
Radiotherapy, chemotherapy and immunotherapy are
the mainstays of treatment [17]. Regimens typically in-
clude an anti-CD20 antibody (rituximab) in comination
with the antracycline based chemotherapy regimen
CHOP (r-CHOP) [15,17,18]. Radiotherapy may also be
considered particularly in presentations of a solitary
small skin tumour. Relapse rates following radiation
have been reported as 58% with extracutaneous progres-
sion rates of 30% [17]. Surgical excision is highly effec-
tive in PCMZL and PCFCCL with a similar efficacy to
radiotherapy, however its efficacy is not well described
in PCLPBL [19].
This case highlights the need for urgent tissue diagno-
sis even when you think the diag nosis is obvio us. Had an
earlier tissue diagnosis been made Initial treatment of
this patient with radiation and/or r-CHOP may have im-
proved his prognosis. The presence of a raised lactate
should also lead one to suspect cutaneous lymphoma. We
therefore recommend that urgent tissue biopsy be per-
formed in all cases of presumed necrotising fasciitis.
REFERENCES
[1] E. J. Whallett, J. H. Stevenson and A. D. Wilmshurst,
“Necrotising Fasciitis of the Extremity,” Journal of Plas-
tic, Reconstructive & Aesthetic Surgery, Vol. 63, No. 5,
2010, pp. e469-e473. doi:10.1016/j.bjps.2009.09.011
[2] R. Kaul, A. McGeer, D. E. Low, et al., “Population-
Based Surveillance for Group a Streptococcal Necrotizing
Fasciitis: Clinical Features, Prognostic Indicators, and
Microbiologic Analysis of Seventy-Seven Cases. Ontario
Group A Streptococcal Study,” American Journal of Me-
dicine, Vol. 103, No. 1, 1997, pp. 18-24.
doi:10.1016/S0002-9343(97)00160-5
[3] D. A. Anaya and E. P. Dellinger, “Necrotizing Soft-Tis-
sue Infection: Diagnosis and Management,” Clinical In-
fectious Diseases, Vol. 44, No. 5, 2007, pp. 705-710.
doi:10.1086/511638
[4] B. J. Childers, L. D. Potyondy, R. Nachreiner, et al., “Ne-
crotizing Fasciitis: A Fourteen-Year Retrospective Study
of 163 Consecutive Patients,” The American Journal of
Surgery, Vol. 68, No. 2, 2002, pp. 109-116.
[5] A. Rahmouni, O. Chosidow, D. Mathieu, et al., “MR
Imaging in Acute Infectious Cellulites,” Radiology, Vol.
192, No. 2, 1994, pp. 493-496.
[6] J. D. Urschel, “Necrotiz ing Soft Tissue Infections,” Post-
graduate Medical Journal, Vol. 75, No. 889, 1999, pp.
645-649. doi:10.1136/pgmj.75.889.645
[7] C. H. Wong, A. K. Yam, A. B. Tan, et al., “Approach to
Debridement in Necrotizing Fasciitis,” The American
Journal of Surgery, Vol. 196, No. 3, 2008, pp. e19-e24.
Copyright © 2012 SciRes. MPS