S. WESTWATER-WOOD ET AL.
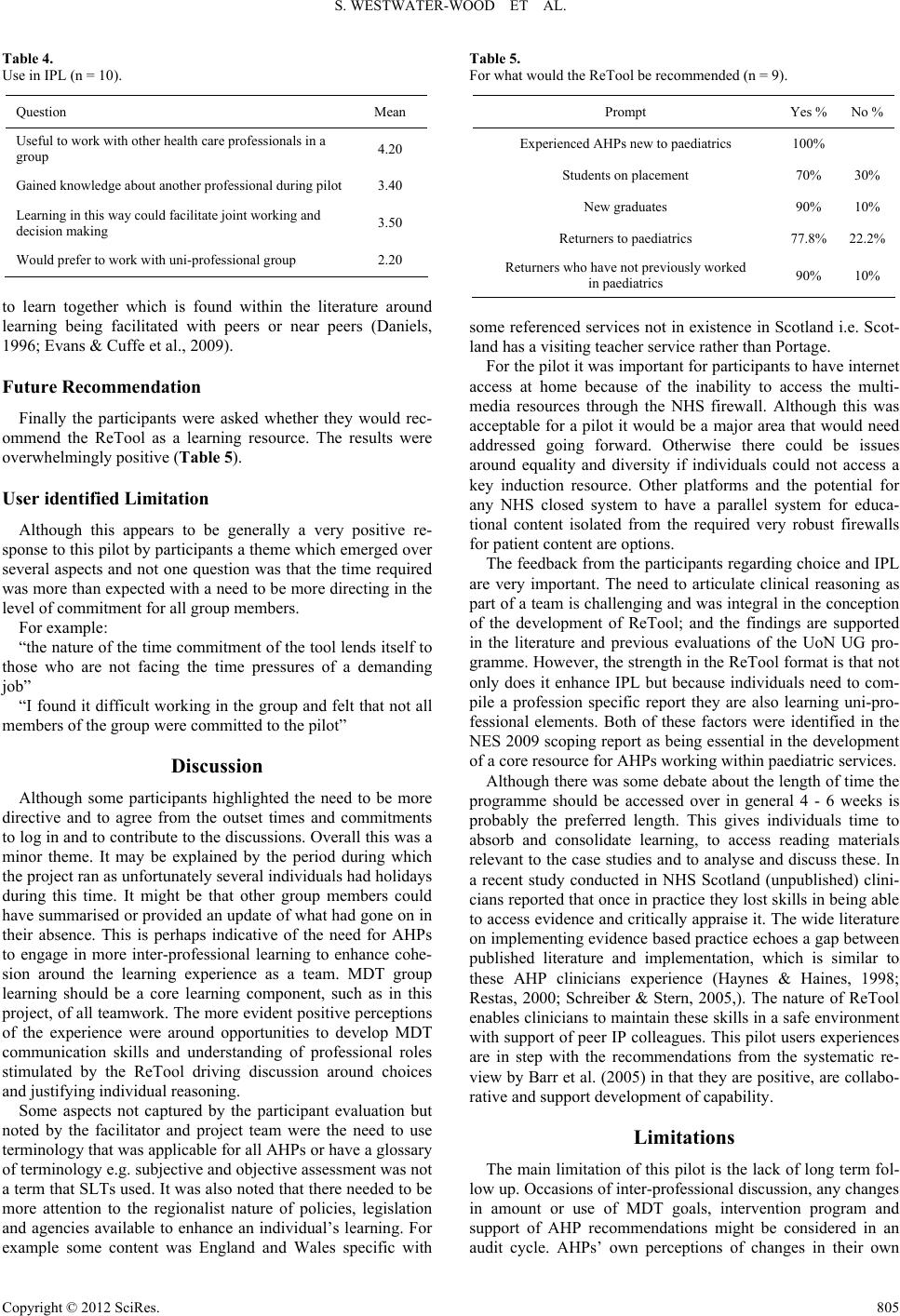
Table 4.
Use in IPL (n = 10).
Question Mean
Useful to work with oth er health care professional s in a
group 4.20
Gained knowl edge about another p r ofessional during pilot 3.40
Learning in this wa y could facilita te joint working and
decision making 3.50
Would prefer to work with uni-professional group 2.20
to learn together which is found within the literature around
learning being facilitated with peers or near peers (Daniels,
1996; Evans & Cuffe et al., 2009).
Future Recommendation
Finally the participants were asked whether they would rec-
ommend the ReTool as a learning resource. The results were
overwhelmingly positiv e (Table 5).
User identified Limitation
Although this appears to be generally a very positive re-
sponse to this pilot by participants a theme which emerged over
several aspects and not one question was that the time required
was more than expected with a need to be more directing in the
level of commitment for all group members.
For example:
“the nature of the time commitment of the tool lends itself to
those who are not facing the time pressures of a demanding
job”
“I found it difficult working in the group and felt that not all
members of the group were committed to the pilot”
Discussion
Although some participants highlighted the need to be more
directive and to agree from the outset times and commitments
to log in and to contribute to the discussions. Overall this was a
minor theme. It may be explained by the period during which
the project ran as unfortunately several individuals had holidays
during this time. It might be that other group members could
have summarised or provided an update of what had gone on in
their absence. This is perhaps indicative of the need for AHPs
to engage in more inter-professional learning to enhance cohe-
sion around the learning experience as a team. MDT group
learning should be a core learning component, such as in this
project, of all teamwork. The more evident positive perceptions
of the experience were around opportunities to develop MDT
communication skills and understanding of professional roles
stimulated by the ReTool driving discussion around choices
and justifying individual reasoning.
Some aspects not captured by the participant evaluation but
noted by the facilitator and project team were the need to use
terminology that was applicable for all AHPs or have a glossary
of terminology e.g. subjective and objective assessment was not
a term that SLTs used. It was also noted that there needed to be
more attention to the regionalist nature of policies, legislation
and agencies available to enhance an individual’s learning. For
example some content was England and Wales specific with
Table 5.
For what would the ReTool be recommended (n = 9).
Prompt Yes %No %
Experienced AHPs new to pae diatrics 100%
Students on pla c eme nt 70% 30%
New graduates 90% 10%
Returners to paediatrics 77.8%22.2%
Returners w ho have not previously worked
in paediatrics 90% 10%
some referenced services not in existence in Scotland i.e. Scot-
land has a visiting teacher service rather than Portage.
For the pilot it was important for participants to have internet
access at home because of the inability to access the multi-
media resources through the NHS firewall. Although this was
acceptable for a pilot it would be a major area that would need
addressed going forward. Otherwise there could be issues
around equality and diversity if individuals could not access a
key induction resource. Other platforms and the potential for
any NHS closed system to have a parallel system for educa-
tional content isolated from the required very robust firewalls
for patient content are options.
The feedback from the participants regarding choice and IPL
are very important. The need to articulate clinical reasoning as
part of a team is challenging and was integral in the conception
of the development of ReTool; and the findings are supported
in the literature and previous evaluations of the UoN UG pro-
gramme. However, the strength in the ReTool format is that not
only does it enhance IPL but because individuals need to com-
pile a profession specific report they are also learning uni-pro-
fessional elements. Both of these factors were identified in the
NES 2009 scoping report as being essential in the development
of a core resource for AHPs working within paediatric services.
Although there was some debate about the length of time the
programme should be accessed over in general 4 - 6 weeks is
probably the preferred length. This gives individuals time to
absorb and consolidate learning, to access reading materials
relevant to the case studies and to analyse and discuss these. In
a recent study conducted in NHS Scotland (unpublished) clini-
cians reported that once in practice they lost skills in being able
to access evidence and critically appraise it. The wide literature
on implementing evidence based practice echoes a gap between
published literature and implementation, which is similar to
these AHP clinicians experience (Haynes & Haines, 1998;
Restas, 2000; Schreiber & Stern, 2005,). The nature of ReTool
enables clinicians to maintain these skills in a safe environment
with support of peer IP colleagues. This pilot users experiences
are in step with the recommendations from the systematic re-
view by Barr et al. (2005) in that they are positive, are collabo-
rative and support development of capability.
Limitations
The main limitation of this pilot is the lack of long term fol-
low up. Occasions of inter-professional discussion, any changes
in amount or use of MDT goals, intervention program and
support of AHP recommendations might be considered in an
audit cycle. AHPs’ own perceptions of changes in their own
Copyright © 2012 SciRes. 805