J.-T. Kim et al. / Natural Science 2 (2010) 764-768
Copyright © 2010 SciRes. OPEN ACCESS
767
767
labeled lysate sensitivity and the test for interfering fac-
tors were performed by using solutions for the gel-clot
test as summarized in Table 1. The end-point is the last
positive results in the series of decreasing concentrations
of endotoxin. The geometric mean end-point concentra-
tion is the measured sensitivity of the lysate solution.
The mean value of the logarithms of the end-point con-
centrations is equivalent to the antilogarithm of the mean
value, (Antilog Mean = 0.12 EU/mL). The antilogarithm
of the mean value is calculated to be −0.921. If the geo-
metric mean end-point concentration of 0.12 EU/mL is
not less than 0.5(0.06) and not more than 2,
the labeled sensitivity is confirmed and is used in the
tests performed with this lysate, as shown in Table 3.
For the lysate to clot under standard conditions, < 0.125
EU/mL was found to be the required concentration of
endotoxins. The material extract was prepared in the
static conditions in LAL reagent water for 1 h at 37oC
[11]. After considering the dilution factor, the final con-
centration of endotoxin was determined to be < 0.005
EU/mg. According to FDA’s “Summary of Safety and
Effectiveness Data,” endotoxin concentrations are 0.5
EU/mL, 20 EU/syringe, 0.08 EU/mL for the three ap-
proved injectable dermal HAH fillers in market, respec-
tively [12-14]. Comparing the HAHs that was synthe-
sized in this experiment to the ones approved by FDA,
the amount of < 0.125 EU/mL endotoxins is relatively
safe and effective [12-14].
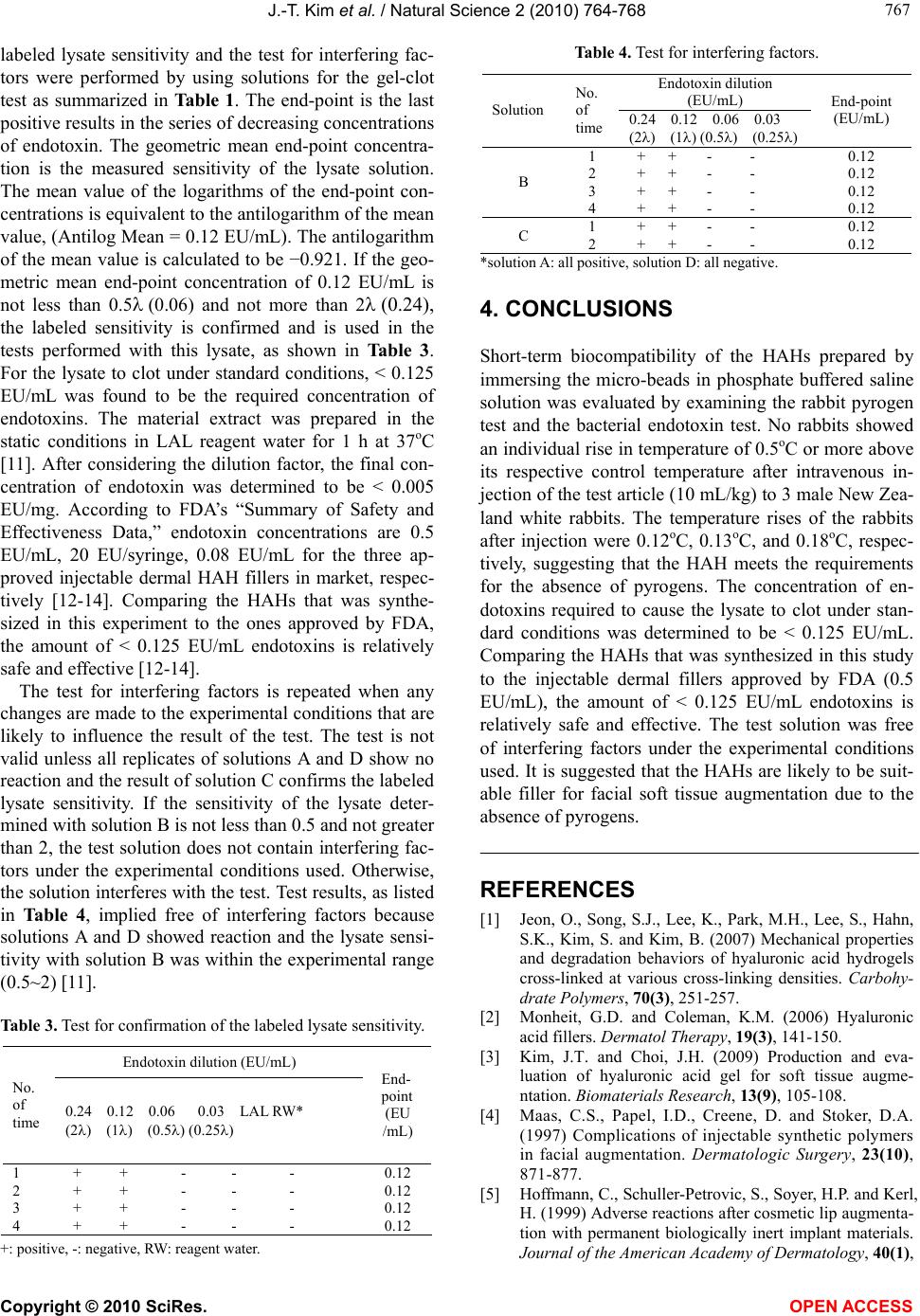
The test for interfering factors is repeated when any
changes are made to the experimental conditions that are
likely to influence the result of the test. The test is not
valid unless all replicates of solutions A and D show no
reaction and the result of solution C confirms the labeled
lysate sensitivity. If the sensitivity of the lysate deter-
mined with solution B is not less than 0.5 and not greater
than 2, the test solution does not contain interfering fac-
tors under the experimental conditions used. Otherwise,
the solution interferes with the test. Test results, as listed
in Table 4, implied free of interfering factors because
solutions A and D showed reaction and the lysate sensi-
tivity with solution B was within the experimental range
(0.5~2) [11].
Table 3. Test for confirmation of the labeled lysate sensitivity.
Endotoxin dilution (EU/mL)
No.
of
time 0.24 0.12 0.06 0.03 LAL RW*
(2) (1) (0.5) (0.25)
End-
point
(EU
/mL)
1
2
3
4
+ + - - -
+ + - - -
+ + - - -
+ + - - -
0.12
0.12
0.12
0.12
+: positive, -: negative, RW: reagent water.
Table 4. Test for interfering factors.
Endotoxin dilution
(EU/mL)
Solution
No.
of
time 0.24 0.12 0.06 0.03
(2) (1) (0.5) (0.25)
End-point
(EU/mL)
B
1
2
3
4
+ + - -
+ + - -
+ + - -
+ + - -
0.12
0.12
0.12
0.12
C 1
2
+ + - -
+ + - -
0.12
0.12
*solution A: all positive, solution D: all negative.
4. CONCLUSIONS
Short-term biocompatibility of the HAHs prepared by
immersing the micro-beads in phosphate buffered saline
solution was evaluated by examining the rabbit pyrogen
test and the bacterial endotoxin test. No rabbits showed
an individual rise in temperature of 0.5oC or more above
its respective control temperature after intravenous in-
jection of the test article (10 mL/kg) to 3 male New Zea-
land white rabbits. The temperature rises of the rabbits
after injection were 0.12oC, 0.13oC, and 0.18oC, respec-
tively, suggesting that the HAH meets the requirements
for the absence of pyrogens. The concentration of en-
dotoxins required to cause the lysate to clot under stan-
dard conditions was determined to be < 0.125 EU/mL.
Comparing the HAHs that was synthesized in this study
to the injectable dermal fillers approved by FDA (0.5
EU/mL), the amount of < 0.125 EU/mL endotoxins is
relatively safe and effective. The test solution was free
of interfering factors under the experimental conditions
used. It is suggested that the HAHs are likely to be suit-
able filler for facial soft tissue augmentation due to the
absence of pyrogens.
REFERENCES
[1] Jeon, O., Song, S.J., Lee, K., Park, M.H., Lee, S., Hahn,
S.K., Kim, S. and Kim, B. (2007) Mechanical properties
and degradation behaviors of hyaluronic acid hydrogels
cross-linked at various cross-linking densities. Carbohy-
drate Polymers, 70(3), 251-257.
[2] Monheit, G.D. and Coleman, K.M. (2006) Hyaluronic
acid fillers. Dermatol Therapy, 19(3), 141-150.
[3] Kim, J.T. and Choi, J.H. (2009) Production and eva-
luation of hyaluronic acid gel for soft tissue augme-
ntation. Biomaterials Research, 13(9), 105-108.
[4] Maas, C.S., Papel, I.D., Creene, D. and Stoker, D.A.
(1997) Complications of injectable synthetic polymers
in facial augmentation. Dermatologic Surgery, 23(10),
871-877.
[5] Hoffmann, C., Schuller-Petrovic, S., Soyer, H.P. and Kerl,
H. (1999) Adverse reactions after cosmetic lip augmenta-
tion with permanent biologically inert implant materials.
Journal of the American Academy of Dermatology, 40(1),