M. Rivero-Garvía et al. / Open Journal of Pediatrics 2 (2012) 257-259
258
The lesion was hypointense on T1-weighted images and
hyperintense on T2-weighted studies, and showed no
enhancement after contrast administration. The main
diagnosis was epidermoid cysts. The patient underwent
suboccipital craniotomy (Figure 1). After V-shaped dural
opening, the tumor was explored, revealing the presence
of desquamated keratin as well as hair follicles sur-
rounded by a thin capsule (Figure 2). Gross total resec-
tion of the lesion was achieved.
The patient was not sequelae of the disease.
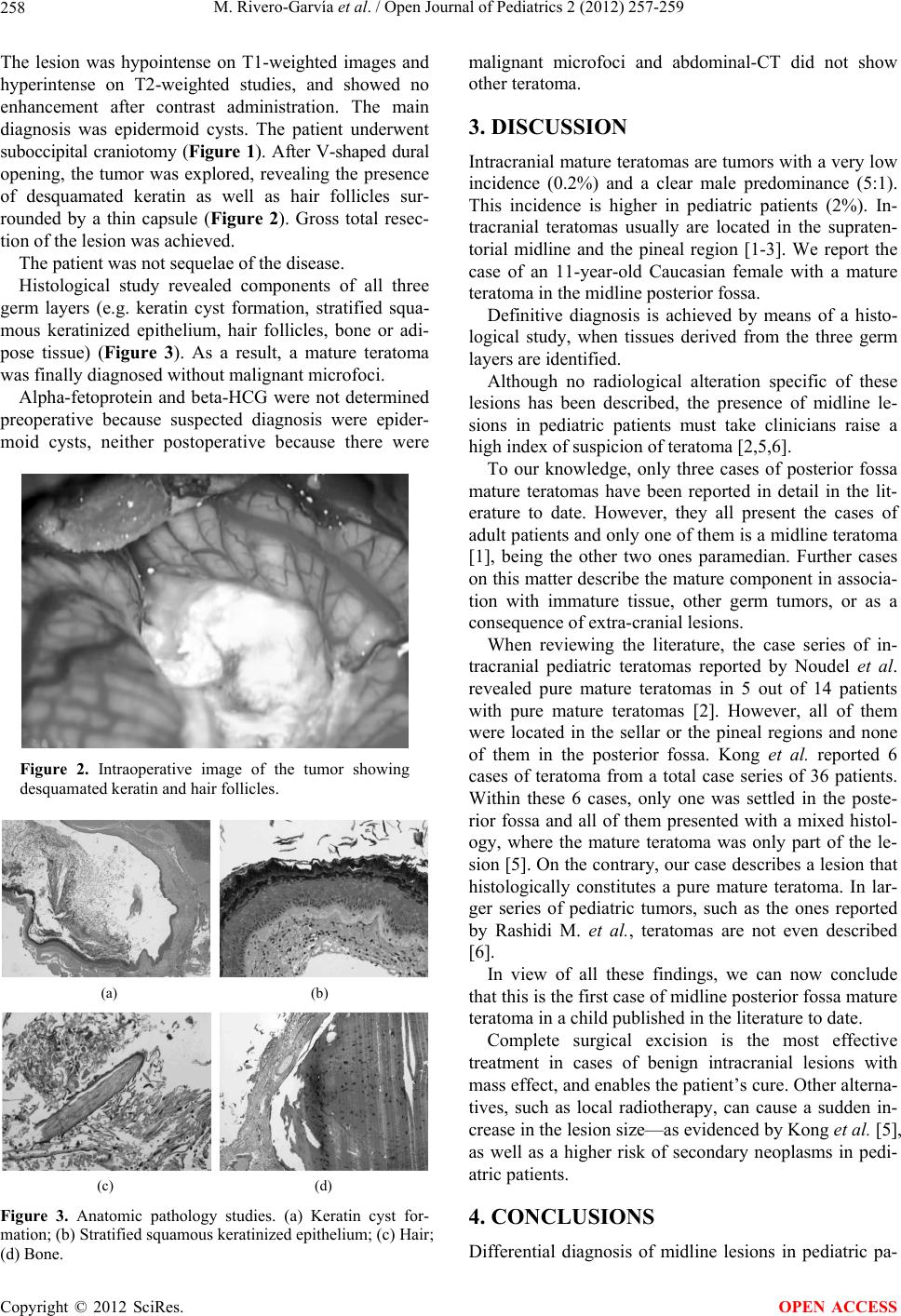
Histological study revealed components of all three
germ layers (e.g. keratin cyst formation, stratified squa-
mous keratinized epithelium, hair follicles, bone or adi-
pose tissue) (Figure 3). As a result, a mature teratoma
was finally diagnosed without malignant microfoci.
Alpha-fetoprotein and beta-HCG were not determined
preoperative because suspected diagnosis were epider-
moid cysts, neither postoperative because there were
Figure 2. Intraoperative image of the tumor showing
desquamated keratin and hair follicles.
(a) (b)
(c) (d)
Figure 3. Anatomic pathology studies. (a) Keratin cyst for-
mation; (b) Stratified squamous keratinized epithelium; (c) Hair;
(d) Bone.
malignant microfoci and abdominal-CT did not show
other teratoma.
3. DISCUSSION
Intracranial mature teratomas are tumors with a very low
incidence (0.2%) and a clear male predominance (5:1).
This incidence is higher in pediatric patients (2%). In-
tracranial teratomas usually are located in the supraten-
torial midline and the pineal region [1-3]. We report the
case of an 11-year-old Caucasian female with a mature
teratoma in the midline posterior fossa.
Definitive diagnosis is achieved by means of a histo-
logical study, when tissues derived from the three germ
layers are identified.
Although no radiological alteration specific of these
lesions has been described, the presence of midline le-
sions in pediatric patients must take clinicians raise a
high index of suspicion of teratoma [2,5,6].
To our knowledge, only three cases of posterior fossa
mature teratomas have been reported in detail in the lit-
erature to date. However, they all present the cases of
adult patients an d only one of them is a midlin e teratoma
[1], being the other two ones paramedian. Further cases
on this matter describe the mature component in associa-
tion with immature tissue, other germ tumors, or as a
consequence of extra-cranial lesions.
When reviewing the literature, the case series of in-
tracranial pediatric teratomas reported by Noudel et al.
revealed pure mature teratomas in 5 out of 14 patients
with pure mature teratomas [2]. However, all of them
were located in the sellar or the pineal regions and none
of them in the posterior fossa. Kong et al. reported 6
cases of teratoma from a total case series of 36 patients.
Within these 6 cases, only one was settled in the poste-
rior fossa and all of them presented with a mixed histol-
ogy, where the mature teratoma was only part of the le-
sion [5]. On the contrary, our case describes a lesion that
histologically constitutes a pure mature teratoma. In lar-
ger series of pediatric tumors, such as the ones reported
by Rashidi M. et al., teratomas are not even described
[6].
In view of all these findings, we can now conclude
that this is the first case of midline posterior fossa mature
teratoma in a child published in the literature to date.
Complete surgical excision is the most effective
treatment in cases of benign intracranial lesions with
mass effect, and enables the patient’s cure. Other alterna-
tives, such as local radiotherapy, can cause a sudden in-
crease in the lesion size—as evidenced by Kong et al. [5],
as well as a higher risk of secondary neoplasms in pedi-
atric patients.
4. CONCLUSIONS
Differential diagnosis of midline lesions in pediatric pa-
Copyright © 2012 SciRes. OPEN ACCESS