Paper Menu >>
Journal Menu >>
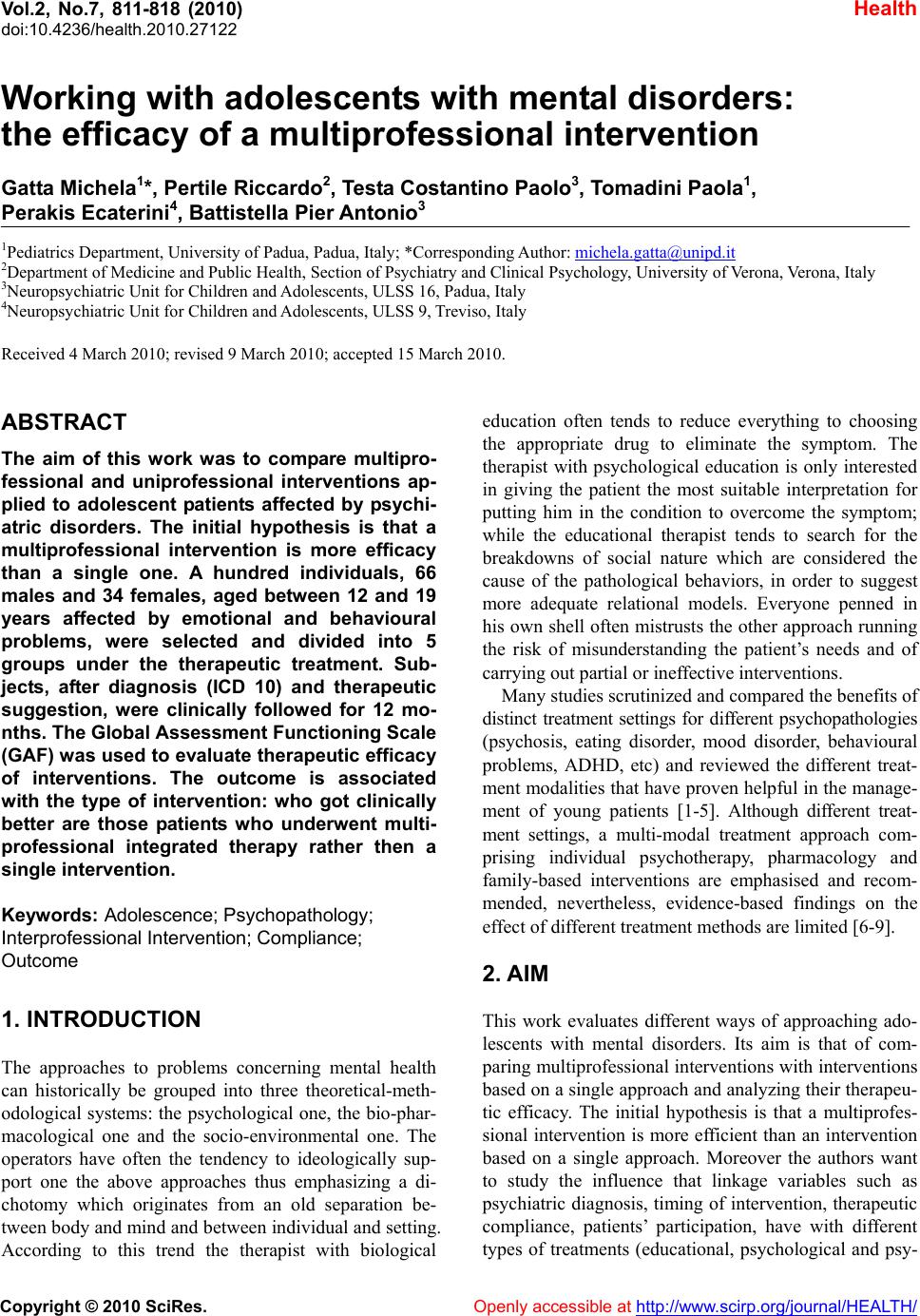 Vol.2, No.7, 811-818 (2010) doi:10.4236/health.2010.27122 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Health Working with adolescents with mental disorders: the efficacy of a multiprofessional intervention Gatta Michela1*, Pertile Riccardo2, Testa Costantino Paolo3, Tomadini Paola1, Perakis Ecaterini4, Battistella Pier Antonio3 1Pediatrics Department, University of Padua, Padua, Italy; *Corresponding Author: michela.gatta@unipd.it 2Department of Medicine and Public Health, Section of Psychiatry and Clinical Psychology, University of Verona, Verona, Italy 3Neuropsychiatric Unit for Children and Adolescents, ULSS 16, Padua, Italy 4Neuropsychiatric Unit for Children and Adolescents, ULSS 9, Treviso, Italy Received 4 March 2010; revised 9 March 2010; accepted 15 March 2010. ABSTRACT The aim of this work was to compare multipro- fessional and uniprofessional interventions ap- plied to adolescent patients affected by psychi- atric disorders. The initial hypothesis is that a multiprofessional intervention is more efficacy than a single one. A hundred individuals, 66 males and 34 females, aged between 12 and 19 years affected by emotional and behavioural problems, were selected and divided into 5 groups under the therapeutic treatment. Sub- jects, after diagnosis (ICD 10) and therapeutic suggestion, were clinically followed for 12 mo- nths. The Global Assessment Functioning Scale (GAF) w as used to evaluate therapeutic efficacy of interventions. The outcome is associated with the type of intervention: who got clinically better are those patients who underwent multi- professional integrated therapy rather then a single intervention. Keywords: Adolescence; Psychopathol ogy; Interprofessional Intervention; Compliance; Outcome 1. INTRODUCTION The approaches to problems concerning mental health can historically be grouped into three theoretical-meth- odological systems: the psychological one, the bio-phar- macological one and the socio-environmental one. The operators have often the tendency to ideologically sup- port one the above approaches thus emphasizing a di- chotomy which originates from an old separation be- tween body and mind and between ind ividual and setting. According to this trend the therapist with biological education often tends to reduce everything to choosing the appropriate drug to eliminate the symptom. The therapist with psychological education is only interested in giving the patient the most suitable interpretation for putting him in the condition to overcome the symptom; while the educational therapist tends to search for the breakdowns of social nature which are considered the cause of the pathological behaviors, in order to suggest more adequate relational models. Everyone penned in his own shell often mistrusts the other approach running the risk of misunderstanding the patient’s needs and of carrying out partial or ineffective interventions. Many studies scrutinized and compared the benefits of distinct treatment settings for different psychopathologies (psychosis, eating disorder, mood disorder, behavioural problems, ADHD, etc) and reviewed the different treat- ment modalities that have proven h elpful in the manage- ment of young patients [1-5]. Although different treat- ment settings, a multi-modal treatment approach com- prising individual psychotherapy, pharmacology and family-based interventions are emphasised and recom- mended, nevertheless, evidence-based findings on the effect of different treatment methods are limited [6-9]. 2. AIM This work evaluates different ways of approaching ado- lescents with mental disorders. Its aim is that of com- paring multiprofessional intervention s with interventions based on a single ap proach and analyzin g their therapeu - tic efficacy. The initial hypothesis is that a multiprofes- sional intervention is more efficient than an intervention based on a single approach. Moreover the authors want to study the influence that linkage variables such as psychiatric diagnosis, timing of intervention, therapeutic compliance, patients’ participation, have with different types of treatments (educational, psychological and psy-  M. Gatta et al. / HEALTH 2 (2010) 811-818 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 812 chiatric ones) and different associations of treatments. 3. METHODOLOGY AND SAMPLE The Neuropsychiatric Unit the patients were referred to, is a second level service which treats medium-severe psychopathological disorders. The structure provides for services characterized by different types of interventions (psychodynamic oriented psychotherapy, educational treatment, pharmacological therapy) chosen according both to the judgment of the specialist who visit the pa- tient and to the service’s vacancy at that moment. To verify the efficacy of different treatments, it has run a retrospective study which has analysed those treated patients for whom one year follow up was available. Patients consecutively undergone one of the three treat- ments (single or in association) during a six months pe- riod were 112 individuals. The period is not very long to limit the unhomogeneity of the sample. One year follow up was available for 100 out of 112 subjects. The psychiatric disorders of the subjects were diag- nosed according to ICD 10 [10]. After diagnosis, patie nt s were suggested to undergo therapeutic treatment, on the basis of the understanding and written consent of each subject and his/her parents. Three kinds of treatment were applied: psychological one (psychotherapy with interviews once a week or twice a month, with psycho- dynamic orientation), psychiatric one (pharmacotherapy antidepressant or atypical antipsychotic drugs and clin- ical monitoring with one to three p sychiatric visits every three months) and educational one (various activities such as theatre/expressive-painting/motility in team and manual laboratories, mediated by educational operators, where the patient can experience his/her abilities and limits individually or in group). These interventions were adopted singularly or in association (two or three of them). Patients were tested before and after the treat- ment. The Global Assessment Functioning Scale (GAF) [11,12] and Youth Self Report (YSR 11-18) [13-15] were used to evaluate therapeutic efficacy of interventions 12 months after the beginning. With respect to the GAF scale, patients were considered clinically improved, worsened or unvaried depending on the scoring reported during the retest (a difference in score of at least 10 points was required to define improvement or aggrava- tion, otherwise the patient was considered unvaried). Clinical evolution was statistically studied in relation to other variables: psychiatric diagnosis, timing of inter- vention, therapeutic compliance, patients’ participation, type of interventio n. Psychiatric diagnosis was formulated according to ICD 10 [10] which is the manual of mental health disor- ders used by clinicians of the Neuropsichiatric Unit of Padua. Timing of intervention considered a period time less then three months, a period time between three and nine months and a period time longer then nine months. Therapeutic compliance was divided and named in ‘adequate’ (when the patient started therapy and main- tain it in accordance with the therapist), ‘discontinuous’ (when the patient was partially compliant, missing at least two sessions consecutively, at least once every three months) and ‘with interruption’ (when the patient dropped out precociously or did not follow the therapeu- tic indications at all). Patient’s participation was evalu- ated on the basis of patient-therapist interaction verified throughout th e analysis of clinical files, reports and min- utes of sessions, interviews and equips: the WAI-O (Working Alliance Inventory-Observer version) trans- lated into Italian language [16-18] was used. WAI-O ratings for each patient were assigned by an external clinician requested to read and scrutinize adolescents’ medical records. Ratings, ranging from a minimum of 120 to a maximum of 168, were split into three groups: 120-132 (which we named as ‘opposition’), 133-145 (which we named as ‘ambivalent participation’), 146- 157 (which we named as ‘passive participation’) and 158-168 (which we named as ‘active participation’). Rating was carried out by a neutral observer during the clinical interviews. The type of intervention was de- scribed on the basis of the single treatment or the asso- ciation of different treatments as explained in the sample section. Data about patients were collected in an anamnesis schedule, then transferred into a computerised database for computation, which is performed using SSPS version 10 and SAS® package, rel. 9.1.3. Statistic Analysis: descriptive analysis, performed with SSPS version 10, first included the frequencies distribu- tion of the main variables collected in the study; then since variables were all expressed in a nominal scale, a Chi-squared test was carried out to identify the relation- ships between therapeutic efficacy and other variables referred to patients. A paired t-test was performed to investigate the differences in YSR’s scores before and after the intervention. Multivariate analysis, performed with SAS® package, rel. 9.1.3, consisted in a multivari- ate logistic regression to identify those variables related to the therapeutic efficacy, while holding the other vari- ables constant in the model. The value of p < 0.05 was considered significant. Among 112 adolescents who were referred in six months time, 100 individuals had been clinically fol- lowed for 12 months. They were 66 males and 34 fe- males, aged between 12 and 19 years, affected by emo- tional and behavioural problems. Their clinical files pro- vided retrospective information about diagnostic and  M. Gatta et al. / HEALTH 2 (2010) 811-818 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 813 813 therapeutic processes. The sample finally taken into consideration was retrospectively divided into 5 groups under therapeutic treatment: 1) psychological treatment 2) educational treatment 3) psychological and educational integrated treatment 4) psychiatric (pharmacological) and psychological integrated treatment 5) psychological, psychiatric and educational integrated treatment 4. RESULTS Results about frequencies analysis of variables are rep- resented in Tables 1-5. Multivariate analysis (carried out with the SAS® pack- age, rel. 9.1.3) was performed using a stepwise logistic regression analysis (significance level for entering = 0.15 and significance level for removing = 0.10) to iden- tify variables related to the therapeutic efficacy, which is the depende nt di ch ot omous variable of the study . Results of Logistic Regression Analysis for patients with an efficient therapy result (cases) compared to pa- tients with a not efficient treatment (controls) are repre- sented in Table 4. Patients with an adequa te therapeutic compliance have a probability 5,762 times higher to present a clinical improvement (p-value = 0.0076) co mpared with patients Table 1. Observed distribution (frequencies and percentages) by age inter vals and sex. Freq % 12-14 yrs 43 43 15-17 yrs 46 46 18-19 yrs 11 11 Age intervals Total 100 100 Male 66 66 Female 34 34 Sex Total 100 100 Age categories by sex Male Female Total 12-14 yrs 32 (74.4) 11 (25.6) 43 (100.0) 15-17 yrs 28 (60.9) 18 (39.1) 46 (100.0) 18-19 yrs 6 (54.5) 5 (45.5) 11 (100.0) Table 2. Observed distribution (frequencies and percentages) by diagnosis ICD 10 and type of treatment. Freq % Diagnosis ICD 10 Psychotic Disorders 18 18 Affective Syndroms 21 21 Neurotic Syndroms 10 10 Personality Disorders 21 21 Soft Mental Retardation 6 6 Behaviour/emotional Disorders 9 9 Eating disorders 4 4 Comorbility (personality dis. + anxiety or mood dis.) 11 11 Total 100 100 Type of treatment Educational Treatment 16 16 Psychological Treatment 15 15 Educational + Psychological Treatment 19 19 Psychological + Psychiatric Treatment 15 15 Educational + Psychiatric Treatment 7 7 Educational + Psychiatric + Psyc ho- logical Treatment 28 28 Total 100 100 who are not compliant. A multiprofessional intervention (p-value = 0.0242) and an active participation of the patient during the treatment (p-value = 0,014) is associ- ated with a probability more than four times higher to obtain a clinical improvement. The last variable entered in the model is ‘timing of therapy’ (p-value = 0.0163): patients whose therapy lasts less than 3 months present a very lower probability (OR = 0.062, CI = 0.009-0.439) to get clinically better compared with patients whose intervention lasts more than 9 months. The p-value of likelihood ratio test < 0.0001 indicates the efficiency of the final model. The percentages of sensitivity and the specificity are respectively 86.2 % and 68.3%. To analyse the differences in Achenbach’s scores (means) before and after the intervention a paired t-test was used. Table 5 shows there was a statistically signifi-  M. Gatta et al. / HEALTH 2 (2010) 811-818 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 814 Table 3. observed distribution (frequencies and percentages) by timing of intervention, patient’s participation, therapy eutic Compliance and clinical outcome (GAF). Freq % Timing of intervention < 3 months 19 19 3-9 months 41 41 > 9 months 40 40 Total 100 100 Patient’s participation Active 53 53 Passive 17 17 Ambivalent 22 22 Total 100 100 Therapeutic compliance Adequate 70 70 Discontinuous 20 20 Early interruption 10 10 Total 100 100 Clinical outcome (GAF) Freq % Improved 58 58 Unchanged 31 31 Got worse 11 11 Total 100 100 cant change (p-value < 0.05) in patients’ Achenbach’s mean scores, most probably due to the treatment efficacy. It is evident, looking at the percentages, that normal scores increased, whereas pathological ones significantly decreased. Using the chi square test a statistically significant re- sult about the relation between type of association of treatments and clinical evolution was obtained: the pa- tients who got clinically better are those who underwent multiprofessional integrated therapy and in particular association between psychological and educational in- tervention, (63%), psychological and psychiatric inter- vention (71%) and the three types together (79%). 5. DISCUSSION The sample is formed by individuals, prevalently boys (66%), basically aged between 12 to 17 years (Table 1). According to literature which shows as in the child- juvenile sectors of psych iatry, bo ys outnumber girls un til the age of 12-14 years and then girls become the major- ity [19], in our sample too the gap between genders de- creases with age, so that after 17 years of age the per- centage of males and females tends to become similar (Table 1). Table 2 shows the diagnosis according to ICD 10 formulated at the end of the psychodiagnostic process. The percentages are quite similar to those of literature about epidemiology of psychiatric disorders in clinic populations of adolescents and young adults [20-22]. The relevant percentage of severe psychopathology as psychosis and personality disorder must be read also within the typology of our service: a second level one which in Italy means a structure functioning in between a outpatients’ and inpatients’ service, where severe psy- chiatric diseases are recovered and treated. Tables 2 shows types of intervention and treatments’ association: the prevalence of multiprofessional interventions (asso- ciation of three different therapies in 28% of cases), be- sides being indicative again of the complexity of pa- tients’ psychopathology, is linked to the general method- ology of our Service where an approach to the adoles- cent that integrates different therapeutic efforts (psychi- atric, psychological and educational ones) is preferred when possible to apply. About the timing of interven- tions, Ta b l e 3 shows that most therapies last more than three months (81%, and 40% more than nine months). Those patients who underwent therapy for less than three months usually are patients that dropped out. Actually, being the Service one which receives individuals af- fected by serious psycho-pathology, suggested therapies habitually last 3 months at least. In Table 3 it is also shown patient’s participation mode in the therapeutic process: active, passive, oppositional or ambivalent. Pa- tient’s way to participate during sessions and activities is significant of the relationship with the therapist and working on the therapeutic allian ce is very imp ortant for a good compliance an d a positive outco me [23-25]. Data about therapeutic compliance and clinical outcome (Ta- ble 3) show that the most of adolescents (70%) followed the therapeutic indicatio ns adequately and nearly 60% of adolescents presented a clinical improvement one year later. Results about outcome obtained using the GAF (filled in by the operators) are confirmed by the ones obtained using the YSR (filled in by the patients) (Table 5). Looking at the scores before and after the treatment it can be noticed that there is an improvement for each syndrome scale, with a statistically significant p-value <  M. Gatta et al. / HEALTH 2 (2010) 811-818 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 815 815 0.05. There are no significant associations between di- agnosis and outcome, suggesting that in developmental age a clinical improvement is more dependent on the therapy and the adherence to it, rather than on the spe- cific psychopathology. Particularly, the results about associations between compliance and outcome (patients who undergo to therapy profiting of it) and between therapy timing and outcome (the longer is the therapy, the more probable is the improvement) suggest that the intervention is efficient when the sessions are attended continuously by the adolescent and for a longer time (Table 4). A brief intervention (19% of adolescents came to the centre for less than 3 months ) is strictly connected with the phenomenon of drop out. This phenomenon turns out to be more frequent at the beginning of the treatment, and particularly in the first 3 months which is the period dedicated to knowledge and definition of the therapeutic project. The problem of early interruption is significant for the relation with patients’ clinical out- come. Between the adolescents who dropped out and those who took part in the whole therapeutic project, there is a statistically relevant difference in terms of clinical evolution, respectively negative and positive. Generally, it must be pointed out the statisticcally rele- vant relation between therapeutic compliance and clini- cal outcome: among patients who are compliant there is a significantly larger rate of adolescents who have showed clinical improvement, compared with the non compliant adolescents. This data, moreover, confirms that patients attending the Neuropsychiatric Unit are affected by a psychological and behavioural disease which needs a moderately long period of time to be worked out. On the basis of this consideration it is possible to interpret the result about the diagnosis (Table 2): such result, actu ally, shows that most adolescents are affected by serious psychiatric disorders (psychosis 18%, depression 21% and personality disorders 21%). These psychopatho- logical conditions are confirmed by the results of YSR: looking at scores (borderline and clinic ones) before in- tervention it can be noticed that the most frequent prob- lems were: withdrawal and social problems (69% and 87%), anxiety and mood disorders (92%), attention problems (97%) (Ta b l e 5 ). Attention problem is proba- bly a symptom of anxious and depressive syndromes rather than a symptom of an ADHD (Attention Deficit and Hyperactivity Disorder). This is supported by the fact that attention problems were reduced after interven- tion (see YSR scores after intervention, Table 5) even if the treatment was not specifically designed for ADHD and the timing of therapy was not long enough for that kind of disorder. Our data suggests that an active participation of the adolescent too contributes to the achievement of a posi- tive result. Table 4, actually, shows that an active par- ticipation of the patient during the treatment implies a higher probability to obtain a clinical improvement. Ac- cording to many authors this result confirms that with adolescents, the therapeutic process must be supported by patient’s motivation and his/her involvement into therapy dynamics [ 26-29]. The association between type of intervention and out- come shows that the subjects who got clinically betterare those patients who underwent multiprofessional therapy (Table 4) and, particularly, the associations between psychological and educational intervention, (63%), psy- chological and psychiatric intervention (71%) and the three types together (79%). It must be pointed out that these three types of multiprofessional intervention have a common element that is the focus on the human rela- tionship: that is the relation between the patient and the clinician/therapist or with the educational professional. Moreover, these types of interventions require an inter- professional team to integrate different therapeutic ac- tions applied to the same patients. Both a multiprofes- sional intervention (giving a specific answer to the indi- vidual and a answer thanks to the intervention of differ- Ta ble 4. Results of logistic regression analysis for patients with therapy effectiveness (cases) compared to patients without therapy effectiveness (controls). Maximum likelihood estimate Standard Errorp-value Odds ratio 95%CI Therapeutic compliance (ref. ‘adequate’) 1.751 0.656 0.0076 5.762 1.594-20.829 Type of intervention (ref. ‘multiprofessional’) 1.432 0.635 0.0242 4.187 1.205-14.544 Timing of intervention (‘< 3 months’ compated to ‘> 9 months’) -1.483 0.617 0.0163 0.062 0.009-0.439 Patient’s participation to the therapy (ref. ‘active’) 1.468 0.597 0.014 4.342 1.346-14.002 Likelihood ratio test: p < 0.0001. Ref, reference category; CI, confidence intervals.  M. Gatta et al. / HEALTH 2 (2010) 811-818 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 816 Table 5. Distribution of patients by Achenbach’s scores before and after the intervention [observed frequencies (%)] and paired t-test value with corresponding p-value. before (100 patients)after (94 patients) paired t-test value p-value normal 31 (31) 66 (70.2) borderline 21 (21) 19 (20.2) Withdrawal clinic 48 (48) 9 (9.6) 5.61 < 0.0001 normal 41 (41) 67 (71.3) borderline 40 (40) 25 (26.6) Somatic complaints clinic 19 (19) 2 (2.1) 5.03 < 0.0001 normal 8 (8) 41 (43.6) borderline 31 (31) 50 (53.2) Anxious-depressive problems clinic 61 (61) 3 (3.2) 9.79 < 0.0001 normal 13 (13) 45 (47.9) borderline 41 (41) 41 (43.6) Social problems clinic 46 (46) 8 (8.5) 6.43 < 0.0001 normal 40 (40) 64 (68.1) borderline 35 (35) 23 (24.5) Thought problem s clinic 25 (25) 7 (7.4) 3.54 < 0.001 normal 30 (30) 65 (69.1) borderline 46 (46) 27 (28.7) Problems of Attention clinic 24 (24) 2 (2.1) 6.45 < 0.0001 normal 80 (80) 84 (89.4) borderline 14 (14) 9 (9.6) Delinquent behaviour clinic 6 (6) 1 (1.1) 2.49 < 0.05 normal 54 (54) 75 (79.8) borderline 27 (27) 17 (18.1) Aggressive behaviour clinic 19 (19) 2 (2.1) 4.58 < 0.0001 ent professionals) and a shared methodology with the possibility of verifying the work done on the individual within a group, contribute to a positive outcome [30,31]. According to that, many studies have just tested the effi- ciency of multimodal interventions on different psycho- pathologies such as ADHD, anxiety disorders, suicidal behaviours, conduct disorders, psychosis etc. [32-35]. 6. CONCLUSIONS This study, with the limitation of being a retrospective research, confirms the major efficacy of a multiprofes- sional integrated approach to the adolescent’s psychopa- thology in comparison with approaches based on a single therapeutic interven tion. A rigid separation among approaches could actually make the operator run the risk of getting a deformed vision of patient’s real needs. This approach does not consider the patient as a complex whole and could easily lead to partial and inefficient interventions. In order to obtain a positive clinical outcome in the treatment of young patients affected by psychiatric dis-  M. Gatta et al. / HEALTH 2 (2010) 811-818 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 817 817 ease, it is essential to organize services for adolescents trying to stimulate and support team work, so as to as- sure a multiprofessional intervention. REFERENCES [1] Bachmann, M., Bachmann, C., Rief, W. and Mattejat, F. (2008) Efficacy of psychiatric and psychotherapeutic in- terventions in children and adolescents with psychiatric disorders—A systematic evaluation of meta-analyses and reviews. Part II: ADHD and conduct disorders. Z Kinder Jugendpsychiatr Psychother, 36(5), 321-333. [2] Bachmann, M., Bachmann, C., Rief, W. and Mattejat, F. (2008) Efficacy of psychiatric and psychotherapeutic in- terventions in children and adolescents with psychiatric disorders-a systematic evaluation of meta-analyses and reviews. Part I: Anxiety disorders and depressive disor- ders. Z Kinder Jugendpsychiatr Psychother, 36(5), 309- 320. [3] Velligan, D.I., Draper, M., Stutes, D., Maples, N., Mintz, J., Tai, S. and Turkington, D. (2009) Multimodal Cogni- tive Therapy: Combining Treatments That Bypass Cog- nitive Deficits and Deal With Reasoning and Appraisal Biases. Schizophrenia Bulletin, 35(5), 884-893. [4] MTA Cooperative Group National Institute of Mental Health (2004) Multimodal Treatment Study of ADHD Follow-up: 24-Month Outcomes of Treatment Strategies for Attention-Deficit/Hyperactivity Disorder. Pediatrics, 113(4), 754-761. [5] Connor, D.F., Carlson, G.A., Chang, K.D., Daniolos, P.T., Ferziger, R., Findling, R.L., Hutchinson, J.G., Malone, R.P., Halperin, J.M., Plattner, B., Post, R.M., Reynolds, D.L., Rogers, K.M., Saxena, K., Steiner, H., Stan- ford/Howard/AACAP Workgroup on Juvenile Impulsiv- ity and Aggression (2006) Juvenile maladaptive aggres- sion: a review of prevention, treatment, and service con- figuration and a proposed research agenda. Journal of Clinical Psychiatry, 67(5), 808-820. [6] Masi, G., Milone, A., Manfredi, A., Pari, C., Paziente, A. and Millepiedi, S. (2008) Conduct disorder in referred children and adolescents: Clinical and therapeutic issues. Comprehensive Psychiatry, 49(2), 146-153. [7] Herpertz-Dahlmann, B. and Salbach-Andrae, H. (2009) Over-view of treatment modalities in adolescent anorexia nervosa. Child and Adolescent Psychiatric Clinics of North America, 18(1), 131-145. [8] Steiner, H. and Remsing, L. (2007) Work Group on Quality Issues Practice parameter for the assessment and treatment of children and adolescents with oppositional defiant disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 46(1), 126-141. [9] Nützel, J., Schmid, M., Goldbeck, L., Fegert, J.M. (2005) Psychiatric support for children and adolescents in resi- dential care in a German sample. Praxis der Kinder- psychologie und Kinderpsychiatrie, 54(8), 627-644. [10] World Health Organization (1992) The ICD-10 Class- ification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. WHO, Geneva. [11] American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders, Axis V. American Psychiatric Associat ion, W ashin gton, D.C. [12] Startup, M., Jackson, M.C., Bendix, S. (2002) The concurrent validity of the Global Assessment of Fun- ctioning (GAF). British Journal of Clinical Psychology, 41(4), 417-422. [13] Achenbach, T.M., Rescorla, L.A. (2001) Manual for the ASEBA School Age-Forms & Profiles. University of Vermont, Research Center for Children, Burlington. [14] Ivanova, M.Y., Achenbach, T.M., Rescorla, L.A., Du- menci, L., Almqvi st, F., Bile nberg, N., Bird, H., Broberg, A.G., Dobrean, A., Döpfner, M., Erol, N., Forns, M., Hannesdottir, H., Kanbayashi, Y., Lambert, M.C., Leung, P., Minaei, A., Mulatu, M.S., Novik, T., Oh, K.J., Rous- sos, A., Sawyer, M., Simsek, Z., Steinhausen, H.C., Weintraub, S., Winkler Metzke, C., Wolanczyk, T., Zilber, N., Zukauskiene, R. and Verhulst, F.C. (2007) The gener- alizability of the Youth Self-Report syndrome structure in 23 societies. Journal of Consulting and Clinical Psy- chology, 75(5), 729-738. [15] Ivanova, M.Y., Dobrean, A., Dopfner, M., Erol, N., Fombonne, E., Fonseca, A.C., Frigerio, A., Grietens, H., Hannesdottir, H., Kanbayashi, Y., Lambert, M., Achenr- bach, T.M., Larsson, B., Leung, P., Liu, X., Minaei, A., Mulatu, M.S., Novik, T.S., Oh, K.J., Roussos, A., Saw- yer, M., Simsek, Z., Dumenci, L., Steinhausen, H.C., Metzke, C.W., Wolanczyk, T., Yang, H.J., Zilber, N., Zu- kauskiene, R., Verhulst, F.C., Rescorla, L.A., Alm-qvist, F., Weintraub, S., Bilenberg, N., Bird, H. and Chen, W.J. (2007) Testing the 8 syndrome structure of the CBCL in 30 societies. Journal of Clinical Child and Adolescent Psychology, 36(3), 405-417. [16] Horvath, A.O. and Greenberg, L.S. (1989) Development and validation of the working alliance inventory. Journal of Counseling Psychology, 36(2), 223-233. [17] Di Giuseppe, R., Linscott, J. and Jilton, R. (1996) De- veloping the therapeutic alliance in children-adolescent psychotherapy. Applied & Preventive Psychology, 5(2), 85-100. [18] Lingiardi, V. (2002) L'alleanza terapeutica. Teoria, clinica, ri cerca. Cortina Raffaello, Mi la no. [19] Cohen, P., Cohen, J., Kasen, S., Velez, C.N., Hartmark, C., Johnson, J., Rojas, M., Brook, J. and Streuning, E.L. (1993) An epidemiological study of disorders in late childhood and adolescence-I. Age- and gender-specific prevalence. Journal of Child Psychology and Psychiatry, 34(6), 851-867. [20] Costello, E.J., Foley, D. and Angold, A. (2006) 10-Year Research Update Review: The Epidemiology of Child and Adolescent Psychiatric Disorders: II. Developmental Epidemiology. Journal of the American Academy of Child & Adolescent Psychia try , 45(1), 8-25. [21] Gabbard, G.O. (2000) Psychodynamic Psychiatry in Clinical Practice, 3rd Edition. American Psychiatric Press, Washington, D.C. [22] Donald, W., Spady, M.D., Donald, P., Schopflocher, Lawrence, W., Svenson, B., Angus and H., Thompson. (2001) Prevalence of mental disorders in children living in Alberta, Canada, as determined from physician billing data. Archives of Pediatrics & Adolescent Medicine, 155, 1153-1159. [23] Horvath, A.O. and Symonds, B.D. (1991) Relation be-  M. Gatta et al. / HEALTH 2 (2010) 811-818 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 818 tween working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counselling Psychology, 38(2), 139-149. [24] Luborsky, L. (2000) A pattern-setting therapeutic alli- ance study revisited: helping alliances in psychotherapy. Psychotherapy Re s e a rch, 10, 17-29. [25] Martin, D.J., Garske, J.P., Davis, M.K. (2000) Relation of the therapeutic alliance with outcome and other varia- bles: A meta-analytic review. Journal of Consulting and Clinical Psycho l o g y, 68(3), 438-450. [26] Horvath, A.O. and Luborsky, L. (1993) The role of thera- peutic alliance in psychotherapy. Journal of Consulting and Clinical Psychology, 61(4), 561-573. [27] Marcelli, D. and Braconnier, A. (1995) Adolescence et Psychopathologie. Masson, Paris. [28] Laufer, M. (1997) Adolescent Breakdown and Beyond. Karnak Books, London. [29] Hintikka, U., Laukkanen, E., Marttunen, M. and Lehto- nen, J. (2006) Good working alliance and psychotherapy are associated with positive changes in cognitive perfor- mance among adolescent psychiatric inpatients. Bulletin of the Menninger Clinic, 70, 316-335. [30] Wachtel, P.L. (1977) Psychoanalysis and behaviour ther- apy: Toward an integration. Guilford Press, New York. [31] Kaneklin, C. and Orsenigo, A. (1992) Il lavoro di Comunità. Nuova Italia Scientifica, Roma. [32] Rea, M., Braccini, L., Laviola, G., Ferri, R. (2006) ADHD and multimodal intervention. Annali dell' Istituto Super- iore di Sanità, 42(2), 231-245. [33] Russell, P.S., Raj, S.E., John, J.K. (1998) Multimodal intervention for selective mutism in mentally retarded children. Journal of the American Academy of Child and Adolescent Psyc h iatry, 37(9), 903-904. [34] Henggeler, S.W., Schoenwald, S.K., Borduin, C.M., Rowland, M.D. and Cunningham, P.B. (1998) Multi-sys- temic treatment of antisocial behaviour in children and adolescents. Guilford Press, New York. [35] Clark, A.F. (2001) Proposed treatment for adolescent psychosis. Schizophrenia and schizophrenia-like psyc- hoses. Advances in Psychiatri c Treatment, 7, 16-23. |

