Paper Menu >>
Journal Menu >>
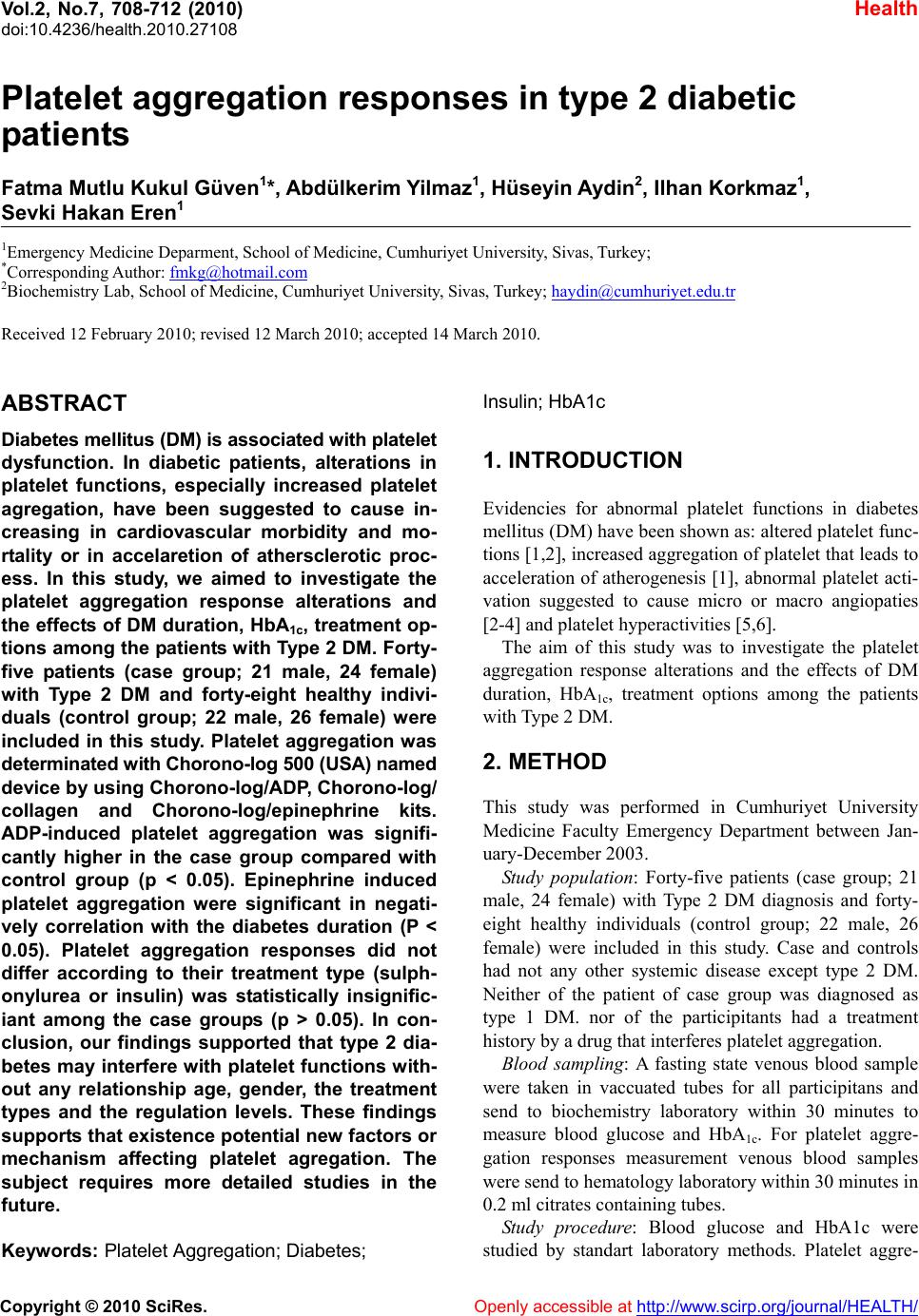 Vol.2, No.7, 708-712 (2010) doi:10.4236/health.2010.27108 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Health Platelet aggregation responses in type 2 diabetic patients Fatma Mutlu Kukul Güven1*, Abdülkerim Y ilmaz1, Hüseyin Aydin2, Ilhan Korkmaz1, Sevki Hakan Eren1 1Emergency Medicine Deparment, School of Medicine, Cumhuriyet University, Sivas, Turkey; *Corresponding Author: fmkg@hotmail.com 2Biochemistry Lab, School of Medicine, Cumhuriyet University, Sivas, Turkey; haydin@cumhuriyet.edu.tr Received 12 February 2010; revised 12 March 2010; accepted 14 March 2010. ABSTRACT Diabetes mellitus (DM) is associated with platelet dysfunction. In diabetic patients, alterations in platelet functions, especially increased platelet agregation, have been suggested to cause in- creasing in cardiovascular morbidity and mo- rtality or in accelaretion of athersclerotic proc- ess. In this study, we aimed to investigate the platelet aggregation response alterations and the effects of DM duration, HbA1c, treatment op- tions among the patients with Type 2 DM. Forty- five patients (case group; 21 male, 24 female) with Type 2 DM and forty-eight healthy indivi- duals (control group; 22 male, 26 female) were included in this study. Platelet aggregation was determinated with Chorono-log 500 (USA) named device by using Chorono-log/ADP, Chorono-log/ collagen and Chorono-log/epinephrine kits. ADP-induced platelet aggregation was signifi- cantly higher in the case group compared with control group (p < 0.05). Epinephrine induced platelet aggregation were significant in negati- vely correlation with the diabetes duration (P < 0.05). Platelet aggregation responses did not differ according to their treatment type (sulph- onylurea or insulin) was statistically insignific- iant among the case groups (p > 0.05). In con- clusion, our findings supported that type 2 dia- betes may interfere with platelet functions with- out any relationship age, gender, the treatment types and the regulation levels. These findings supports that existence potential new factors or mechanism affecting platelet agregation. The subject requires more detailed studies in the future. Keywords: Platelet Aggregation; Diabetes; Insulin; HbA1c 1. INTRODUCTION Evidencies for abnormal platelet functions in diabetes mellitus (DM) have been shown as: altered platelet func- tions [1,2], increased aggregation of platelet that leads to acceleration of atherogenesis [1], abnormal platelet acti- vation suggested to cause micro or macro angiopaties [2-4] and platelet hyperactivities [5,6]. The aim of this study was to investigate the platelet aggregation response alterations and the effects of DM duration, HbA1c, treatment options among the patients with Type 2 DM. 2. METHOD This study was performed in Cumhuriyet University Medicine Faculty Emergency Department between Jan- uary-December 2003. Study population: Forty-five patients (case group; 21 male, 24 female) with Type 2 DM diagnosis and forty- eight healthy individuals (control group; 22 male, 26 female) were included in this study. Case and controls had not any other systemic disease except type 2 DM. Neither of the patient of case group was diagnosed as type 1 DM. nor of the participitants had a treatment history by a drug that interferes platelet aggregation. Blood sampling: A fasting state venous blood sample were taken in vaccuated tubes for all participitans and send to biochemistry laboratory within 30 minutes to measure blood glucose and HbA1c. For platelet aggre- gation responses measurement venous blood samples were send to hematology laboratory within 30 minutes in 0.2 ml citrates containing tubes. Study procedure: Blood glucose and HbA1c were studied by standart laboratory methods. Platelet aggre-  F. M. K. Güven et al. / HEALTH 2 (2010) 708-712 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 709 709 gation was determinated with Chorono-log 500 (USA) named device by using Chorono-log/ADP, Chorono-log/ collegen and Chorono-log/epinephrine kits. Statistical analysis: Data analysis were performed on SPSS (Ver 13.0) software by using chi-square, studen-t, Mann-Whitney U tests and correlation analysis. 3. RESULTS The mean age was 58.68 ± 1.37 years in the case group and 53.72 ± 2.10 years in the control group. When case and control groups were statistically compared upon to their mean age and gender the difference was insig- nificant (P > 0.05) (Table 1). The mean glucose levels in the case and control groups were as 224.44 ± 15.95 mg/dl and 99.16 ± 11.84 mg/dl. The mean HbA1c level in the case group was 9.59 ± 0.38 mg/dl. The mean duration of diabetes in the case group was 8.06 ± 0.83 years. Sulfo- nylurea drugs were used in 44.45% [20] patient and insulin was preferred in 55.5% [25] patient for treatment. Platelet aggregation responses induced with epinep- hrine, collagen and adenosine diphosphate (ADP) were measured and mean results were recorded as percen- tage(%) for both groups. The difference between the case and control groups were statistically insignificiant in terms of platelet aggregation responses induced with epinephrine and collagen (p > 0.05). Whereas; ADP-ind- uced platelet aggregation was significantly higher in the case group compared with control group. (Table 2). Platelet aggregation responses induced with all three activators were not in correlation with the ages in the both groups. (Table 3). Platelet aggregation responses induced with all three activators were in negatively correlation with the diabetes duration. However, the correlation were significant for only epinephrine (P < 0.05). (Table 4). When the platelet aggregation responses induced with three activators in the case groups were compared with HbA1c levels and the difference were not significant in statistical analysis (p > 0.05). (Table 5). Platelet aggregation responses did not differ according to their treatment type (sulphonylurea or insulin) and statistically it was insignificiant among the case groups (p > 0.05). (Table 6). 4. DISCUSSION Platelets functions are significant to understanding the pathophysiology of vascular disease in diabetes. The role of hyperglycemia is not clear in platelet hyperactivity in diabetic patients [7]. Platelet dysfunction may develop before vessel wall damage in diabetes [8,9]. Platelet dysfunction in diabetes, including altered adhesion and aggregation, is hypersen- sitivity to agonists [10]. Patient with type 2 DM had altered platelet functions and increased platelet aggregation responses with agon- ists [11,12]. Table 1. Epidemiological and laboratory properties of case and control groups. Cases x ± Se Controls x ± Se P n (f/m) 45 (24/21) 48 (26/22) p > 0.05 Mean Age (year) 58.68 ± 1.37 53.72 ± 2.10 p > 0.05 Mean time of DM (year) 8.06 ± 0.83 - - Treatment (OAD/ins)20/25 - - HbA1c(mg/dL) 9.59 ± 0.38 - - Blood glucose (mg/dL) 224.44 ± 15.95 99.16 ± 11.84 P < 0.05 Table 2. Comparison of platelet aggregation responses in the case and control groups. Groups Epinephrine induced platelet aggregation (%) Collagen induced platelet aggregation (%) ADP induced platelet aggregation (%) Case 45.75 ± 2.26 54.82 ± 2.76 74.91 ± 3.61 Control 42.43 ± 2.78 51.39 ± 2.00 55.72 ± 1.77 p t = 0.91 p > 0.05t = 1.01 p > 0.05 t = 4.85 p < 0.05 Table 3. Correlation between the age and platelet aggregation in the case and control groups. Age Epinephrine (%) collagen (%) ADP (%) Case 58.68 ± 1.37 r = 0.11 p > 0.05 r = 0.03 p > 0.05 r = 0.13 p > 0.05 Control 53.72 ± 2.10 r = −0.11 p > 0.05 r = −0.09 p > 0.05 r = −0.07 p > 0.05 Table 4. Correlation between Diabetes duration and platelet aggregation in the case group. Epinephrine (%) Collagen (%) ADP (%) r = −0.31 r = −0.23 r = 0.11 Diabetes duration 8.06 ± 0.83 p < 0.05 p > 0.05 p > 0.05 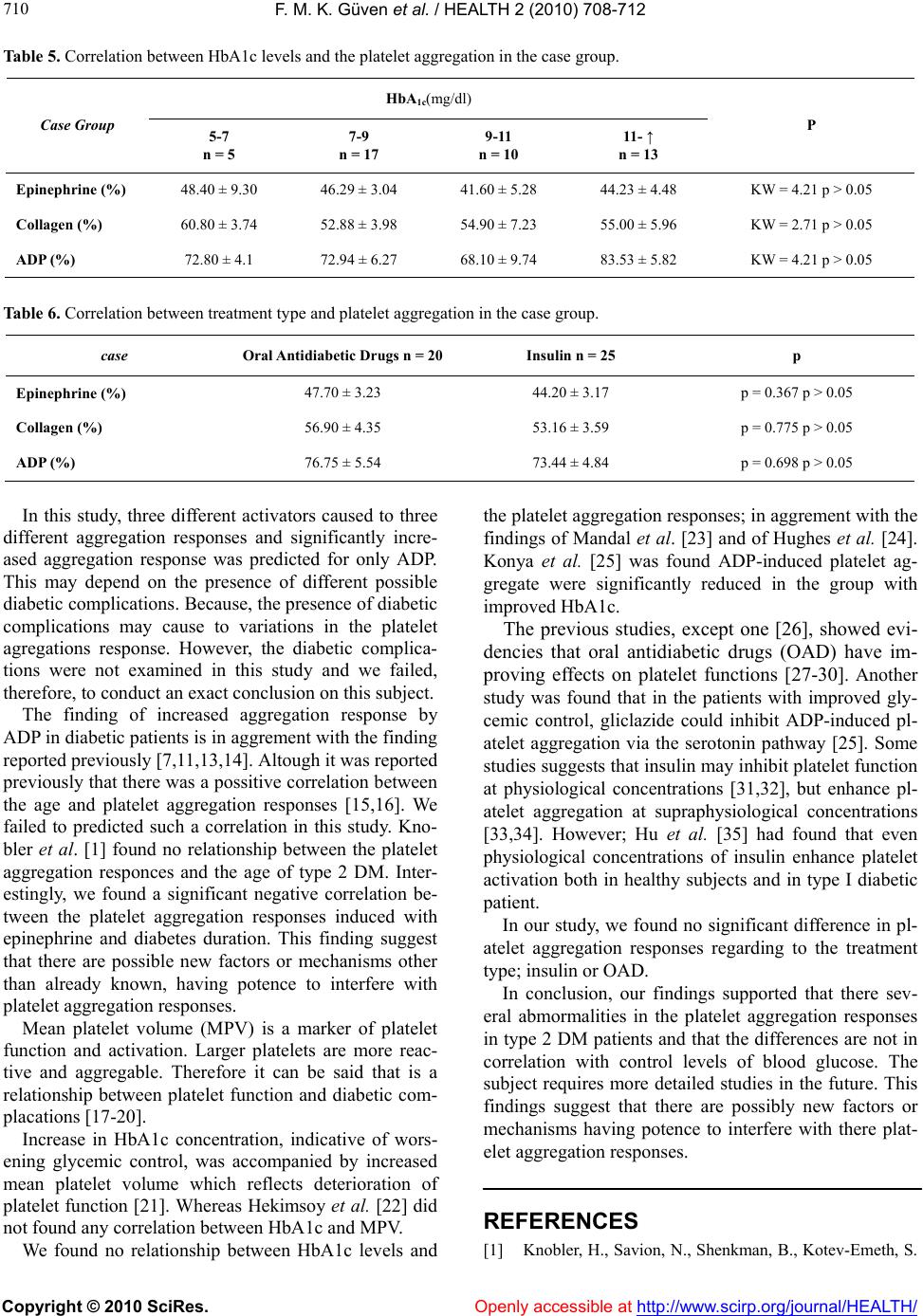 F. M. K. Güven et al. / HEALTH 2 (2010) 708-712 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/ 710 Table 5. Correlation between HbA1c levels and the platelet aggregation in the case group. HbA1c(mg/dl) Case Group 5-7 n = 5 7-9 n = 17 9-11 n = 10 11- ↑ n = 13 P Epinephrine (%) 48.40 ± 9.30 46.29 ± 3.04 41.60 ± 5.28 44.23 ± 4.48 KW = 4.21 p > 0.05 Collagen (%) 60.80 ± 3.74 52.88 ± 3.98 54.90 ± 7.23 55.00 ± 5.96 KW = 2.71 p > 0.05 ADP (%) 72.80 ± 4.1 72.94 ± 6.27 68.10 ± 9.74 83.53 ± 5.82 KW = 4.21 p > 0.05 Table 6. Correlation between treatment type and platelet aggregation in the case group. case Oral Antidiabetic Drugs n = 20 Insulin n = 25 p Epinephrine (%) 47.70 ± 3.23 44.20 ± 3.17 p = 0.367 p > 0.05 Collagen (%) 56.90 ± 4.35 53.16 ± 3.59 p = 0.775 p > 0.05 ADP (%) 76.75 ± 5.54 73.44 ± 4.84 p = 0.698 p > 0.05 In this study, three different activators caused to three different aggregation responses and significantly incre- ased aggregation response was predicted for only ADP. This may depend on the presence of different possible diabetic complications. Because, the presence of diabetic complications may cause to variations in the platelet agregations response. However, the diabetic complica- tions were not examined in this study and we failed, therefore, to conduct an exact conclusion on this subject. Openly accessible at The finding of increased aggregation response by ADP in diabetic patients is in aggrement with the finding reported previously [7,11,13,14]. Altough it was reported previously that there was a possitive correlation between the age and platelet aggregation responses [15,16]. We failed to predicted such a correlation in this study. Kno- bler et al. [1] found no relationship between the platelet aggregation responces and the age of type 2 DM. Inter- estingly, we found a significant negative correlation be- tween the platelet aggregation responses induced with epinephrine and diabetes duration. This finding suggest that there are possible new factors or mechanisms other than already known, having potence to interfere with platelet aggregation responses. Mean platelet volume (MPV) is a marker of platelet function and activation. Larger platelets are more reac- tive and aggregable. Therefore it can be said that is a relationship between platelet function and diabetic com- placations [17-20]. Increase in HbA1c concentration, indicative of wors- ening glycemic control, was accompanied by increased mean platelet volume which reflects deterioration of platelet function [21]. Whereas Hekimsoy et al. [22] did not found any correlation between HbA1c and MPV. We found no relationship between HbA1c levels and the platelet aggregation responses; in aggrement with the findings of Mandal et al. [23] and of Hughes et al. [24]. Konya et al. [25] was found ADP-induced platelet ag- gregate were significantly reduced in the group with improved HbA1c. The previous studies, except one [26], showed evi- dencies that oral antidiabetic drugs (OAD) have im- proving effects on platelet functions [27-30]. Another study was found that in the patients with improved gly- cemic control, gliclazide could inhibit ADP-induced pl- atelet aggregation via the serotonin pathway [25]. Some studies suggests that insulin may inhibit platelet function at physiological concentrations [31,32], but enhance pl- atelet aggregation at supraphysiological concentrations [33,34]. However; Hu et al. [35] had found that even physiological concentrations of insulin enhance platelet activation both in healthy subjects and in type I diabetic patient. In our study, we found no significant difference in pl- atelet aggregation responses regarding to the treatment type; insulin or OAD. In conclusion, our findings supported that there sev- eral abmormalities in the platelet aggregation responses in type 2 DM patients and that the differences are not in correlation with control levels of blood glucose. The subject requires more detailed studies in the future. This findings suggest that there are possibly new factors or mechanisms having potence to interfere with there plat- elet aggregation responses. REFERENCES [1] Knobler, H., Savion, N., Shenkman, B., Kotev-Emeth, S.  F. M. K. Güven et al. / HEALTH 2 (2010) 708-712 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 711 711 and Varon, D. (1998) Shear-induced platelet adhesion and aggregation on subendothelium are increased in diabetic patients. Thrombosis Research, 90(4), 181-190. [2] Li, Y., Woo, V. and Bose, R. (2001) Platelet hyperactivity and abnormal Ca2+ homeasis in diabetes mellitus. Amer- ican Journal of Physiol Heart Circ Physiol, 280(4), 1480-1489. [3] Ross, R. (1986) The pathogenesis of atherosclerosis. The New England Journal of Medicine, 314(8), 488-500. [4] Sinzinger, H. (1986) Role of platelets in atherosclerosis. Semin Thromb Haemostasis, 2(12), 124-133. [5] Bern, M.M. (1978) Platelet functions in diabetes mell- itus. Diabetes, 27(3), 342-350. [6] Colwell, J.A., Lopes-Virella, M. and Halushka, P.V. (1981) Pathogenesis of atherosclerosis in diabetes mell- itus. Diabetes Care, 4(1), 121-133. [7] Vinik, A.I., Erbas, T., Park, T.S., Nolan, R. and Pittenger, G.L. (2001) Platelet Dysfunction in Type 2 Diabetes. Diabetes Care, 24(8), 1476-1485. [8] Davi, G., Gresele, P., Violi, F., Basili, S., Catalano, M., Giammarresi, C., Volpato, R., Nenci, G. G., Ciabattoni, G. and Patrono, C. (1997) Diabetes mellitus, hypercho- lesterolemia, and hypertension but not vascular disease per se are associated with persistent platelet activation in vivo. Evidence derived from the study of peripheral arterial disease. Circulation, 96(1), 69-75. [9] Colwell, J.A., Winocour, P.D. and Halushka, P.V. (1983) Do platelets have anything to do with diabetic micro- vascular disease? Diabetes, 32(2), 14-19. [10] Natarajan, A., Zaman, A.G. and Sally, M.M. (2008) Platelet hyperactivity in type 2 diabetes: Role of antip- latelet agents. Diabetes and Vascular Disease Research, 5(2), 138-144. [11] Tóth, L., Szénási, P., Jámbor, G., Kammerer, L. and Romics, L. (1992) Platelet Function in Male Diabetic With and Without Macrovascular Complications. Diabetes Res Clin Pract, 15(2), 143-148. [12] Hajek, A.S. and Joist, J.H. (1992) Platelet insulin re- ceptor. Methods Enzymol, 215, 399-403. [13] Trovati, M., Anfossi, G., Cavalot, F., Massucco, P., Mularoni E. and Emanuelli, G. (1988) Insulin directly reduces platelet sensivity to aggregating agents. Diabetes, 37(6), 780-786. [14] DeFronzo, R.A. (1992) Insulin resistance, hyperinsuline- mia and coronary artery disease, a complex metabolic web. Journal of Cardiovascular Pharmacology, 20(11), 1-16. [15] Terres, W., Weber, K., Kupper, W. and Bleifeld, W. (1991) Age, cardiovascular risk factors and coronary heart disease as determinants of platelet function in men. A multivariate approach. Thrombosis Research, 62(6), 649- 661. [16] O’Donnell, C.J., Larson, M.G., Feng, D., Sutherland, P. A., Lindpaintner, K., Myers R.H., D’Agostino, R.A., Levy, D. and Tofler, G.H. (2001) Genetic and Enviro- nmental Contributions to Platelet Aggregation: Framing- ham Heart Study. Circulation, 103(25), 3051-3056. [17] Bath,, P.M. and Butterworth, R.J. (1996) Platelet size: Measurement, physiology and vascular disease. Blood Coagulation and Fibrinolysis, 7(2), 157-161. [18] Kim, S.W., Ryu, G.H., Lee, I., Koh, J.J., Min, B.G. and Lee, H.K. (1995) Adhered platelet morphology in dia- betes mellitus. Diabetes and Metabolism, 21(1), 50-53. [19] Mazzanfi, L. and Mutus, B. (1997) Diabetes-induced alterations in platelet metabolism. Clinical Biochemistry, 30(7), 509-515. [20] Srivastava, S., Joshi, C.S., Sethi , P.P., Agrawal, A.K., Srivastava, S.K. and Seth, P.K. (1994) Altered platelet functions in non-insulin-dependent diabetes mellitus (NIDDM). Thrombosis Research, 76(5), 451-461. [21] Demirtunc, R., Duman, D., Basar, M., Bilgi, M., Teomete, M. and Garip, T. (2009) The relationship between glyc- emic control and platelet activity in type 2 diabetes mell- itus. Journal of Diabetes and its Complications, 23(2), 89-94. [22] Hekimsoy, Z., Payzin, B., Ornek, T. and Kandoğan, G. (2004) Mean platelet volume in Type 2 diabetic patients. Journal of Diabetes and its Complications, 18(3), 173- 176. [23] Mandal, S., Sarode, R., Dash, S. and Dash, R.J. (1993) Hyperaggregation of platelets detected by whole blood platelet aggregometry in newly diagnosed noninsulin- dependent diabetes mellitus. American Journal of Cl ini cal Pathology, 100(2), 103-107. [24] Hughes, A., McVerry, B.A., Wilkinson, L., Goldstone, A. H., Lewis, D. and Bloom, A. (1983) Diabetes, a hyper- coagulable state? Hemostatic variables in newly diagn- osed type 2 diabetic patients. Acta Haematol, 69(4), 254- 259. [25] Konya, H., Hasegawa, Y., Hamaguchi, T., Satani, K., Umehara, A., Katsuno, T., Ishikawa, T., Miuchi, M., Kohri, K., Suehiro, A., Kakishita, E., Miyagawa, J.I. and Namba, M. (2010) Effects of gliclazide on platelet aggregation and the plasminogen activator inhibitor type 1 level in patients with type 2 diabetes mellitus. Metabo- lism, Epub ahead of print. [26] Larkins, R.G., Jerums, G., Taft, J.L., Godfrey, H., Smith, I. L. and Martin, T.J. (1988) Lack of effect of gliclazide on platelet aggregation in insulin-treated and non-insulin- treated diabetes: A two-year controlled study. Diabetes Research and Clinical Practice, 4(2), 81-87. [27] Losert, V.W., Scholz, C. and Hoder, A. (1975) Mechan- isms of platelet aggregation inhibition caused by sulfony- lurea compounds. Arzneimittelforschung, 25(4), 547-560. [28] Klaff, L.J., Vinik, A.I., Jackson, W.P., Malan, E., Kernoff, L. and Jacobs, P. (1979) Effects of the sulphonylurea drugs gliclazide and glibenclamide on blood glucose control and platelet function. South African Medical Journal, 56(7), 247-250. [29] Siluk, D., Kaliszan, R., Haber, P., Petrusewicz, J., Brz- ozowski, Z. and Sut, G. (2002) Antiaggregatory activity of hypoglycaemic sulphonylureas. Diabetologia, 45(7), 1034-1037. [30] Qi, R., Ozaki, Y., Satoh, K., Kurota, K., Asazuma, N., Yatomi, Y. and Kume S. (1995) Sulphonylurea agents inhibit platelet aggregation and [Ca2+]i elevation indu- ced by arachidonic acid. Biochemical Pharmacology, 49(12), 1735-1739. [31] Westerbacka, J., Yki-Järvinen, H., Turpeinen, A., Riss- anen, A., Vehkavaara, S., Syrjälä, M. and Lassila, R. (2002) Inhibition of platelet-collagen interaction: An in vivo action of insulin abolished by insulin resistance in obesity. Arteriosclerosis, Thrombosis, and Vascular Bio- logy, 22(1), 167-172.  F. M. K. Güven et al. / HEALTH 2 (2010) 708-712 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 712 [32] Trovati, M. and Anfossi, G. (1998) Insulin, insulin resis- tance and platelet function: Similarities with insulin effects on cultured vascular smooth muscle cells. Dia- betologia, 41(6), 609-622. [33] Murer, E.H., Gyda, M.A. and Martinez, N.J. (1994) Insulin increases the aggregation response of human platelets to ADP. Thrombosis Research, 73(1), 69-74. [34] Anfossi, G., Massucco, P., Mattiello, L., Piretto, V., Mular- oni, E., Cavalot, F., Paoletti, G. and Trovati, M. (1996) Insulin exerts opposite effects on platelet function at physiological and supraphysiological concentrations. Thrombosis Research, 82(1), 57-68. [35] Hu, H., Hjemdahl, P. and Li, N. (2002) Effects of insulin on platelet and leukocyte activity in whole blood. Throm- bosis Research, 107(5), 209-215. |

