Penile Epidermoid Cyst Consisted of Multiple Foci: A Case Report 215
peared to be full of a cheese-like material and the cyst
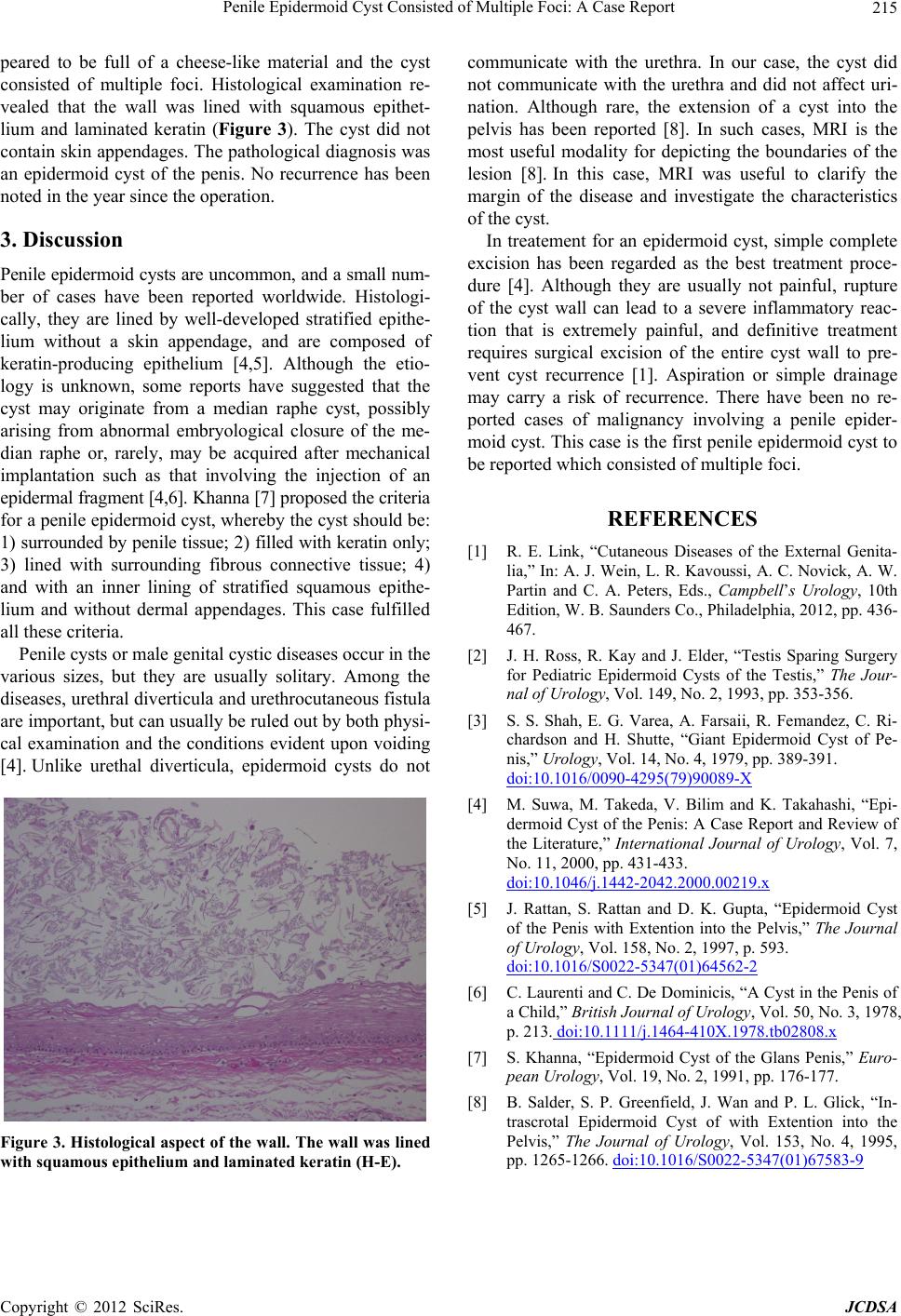
consisted of multiple foci. Histological examination re-
vealed that the wall was lined with squamous epithet-
lium and laminated keratin (Figure 3). The cyst did not
contain skin appendages. The pathological diagnosis was
an epidermoid cyst of the penis. No recurrence has been
noted in the year since the operation.
3. Discussion
Penile epidermoid cysts are uncommon, and a small num-
ber of cases have been reported worldwide. Histologi-
cally, they are lined by well-developed stratified epithe-
lium without a skin appendage, and are composed of
keratin-producing epithelium [4,5]. Although the etio-
logy is unknown, some reports have suggested that the
cyst may originate from a median raphe cyst, possibly
arising from abnormal embryological closure of the me-
dian raphe or, rarely, may be acquired after mechanical
implantation such as that involving the injection of an
epidermal fragment [4,6]. Khanna [7] proposed the criteria
for a penile epidermoid cyst, whereby the cyst should be:
1) surrounded by penile tissue; 2) filled with keratin only;
3) lined with surrounding fibrous connective tissue; 4)
and with an inner lining of stratified squamous epithe-
lium and without dermal appendages. This case fulfilled
all these criteria.
Penile cysts or male genital cystic diseases occur in the
various sizes, but they are usually solitary. Among the
diseases, urethral diverticula and urethrocutaneous fistula
are important, but can usually be ruled out by both physi-
cal examination and the conditions evident upon voiding
[4]. Unlike urethal diverticula, epidermoid cysts do not
Figure 3. Histological aspect of the wall. The wall was lined
with squamous epithelium and laminated keratin (H-E).
communicate with the urethra. In our case, the cyst did
not communicate with the urethra and did not affect uri-
nation. Although rare, the extension of a cyst into the
pelvis has been reported [8]. In such cases, MRI is the
most useful modality for depicting the boundaries of the
lesion [8]. In this case, MRI was useful to clarify the
margin of the disease and investigate the characteristics
of the cyst.
In treatement for an epidermoid cyst, simple complete
excision has been regarded as the best treatment proce-
dure [4]. Although they are usually not painful, rupture
of the cyst wall can lead to a severe inflammatory reac-
tion that is extremely painful, and definitive treatment
requires surgical excision of the entire cyst wall to pre-
vent cyst recurrence [1]. Aspiration or simple drainage
may carry a risk of recurrence. There have been no re-
ported cases of malignancy involving a penile epider-
moid cyst. This case is the first penile epidermoid cyst to
be reported which consisted of multiple foci.
REFERENCES
[1] R. E. Link, “Cutaneous Diseases of the External Genita-
lia,” In: A. J. Wein, L. R. Kavoussi, A. C. Novick, A. W.
Partin and C. A. Peters, Eds., Campbell’s Urology, 10th
Edition, W. B. Saunders Co., Philadelphia, 2012, pp. 436-
467.
[2] J. H. Ross, R. Kay and J. Elder, “Testis Sparing Surgery
for Pediatric Epidermoid Cysts of the Testis,” The Jour-
nal of Urology, Vol. 149, No. 2, 1993, pp. 353-356.
[3] S. S. Shah, E. G. Varea, A. Farsaii, R. Femandez, C. Ri-
chardson and H. Shutte, “Giant Epidermoid Cyst of Pe-
nis,” Urology, Vol. 14, No. 4, 1979, pp. 389-391.
doi:10.1016/0090-4295(79)90089-X
[4] M. Suwa, M. Takeda, V. Bilim and K. Takahashi, “Epi-
dermoid Cyst of the Penis: A Case Report and Review of
the Literature,” International Journal of Urology, Vol. 7,
No. 11, 2000, pp. 431-433.
doi:10.1046/j.1442-2042.2000.00219.x
[5] J. Rattan, S. Rattan and D. K. Gupta, “Epidermoid Cyst
of the Penis with Extention into the Pelvis,” The Journal
of Urology, Vol. 158, No. 2, 1997, p. 593.
doi:10.1016/S0022-5347(01)64562-2
[6] C. Laurenti and C. De Dominicis, “A Cyst in the Penis of
a Child,” British Journal of Urology, Vol. 50, No. 3, 1978,
p. 213. doi:10.1111/j.1464-410X.1978.tb02808.x
[7] S. Khanna, “Epidermoid Cyst of the Glans Penis,” Euro-
pean Urology, Vol. 19, No. 2, 1991, pp. 176-177.
[8] B. Salder, S. P. Greenfield, J. Wan and P. L. Glick, “In-
trascrotal Epidermoid Cyst of with Extention into the
Pelvis,” The Journal of Urology, Vol. 153, No. 4, 1995,
pp. 1265-1266. doi:10.1016/S0022-5347(01)67583-9
Copyright © 2012 SciRes. JCDSA