Scleredema Diabeticorum in a Patient with the Normal Range of the Hemoglobin A1c Level
and Impaired Glucose Tolerance
142
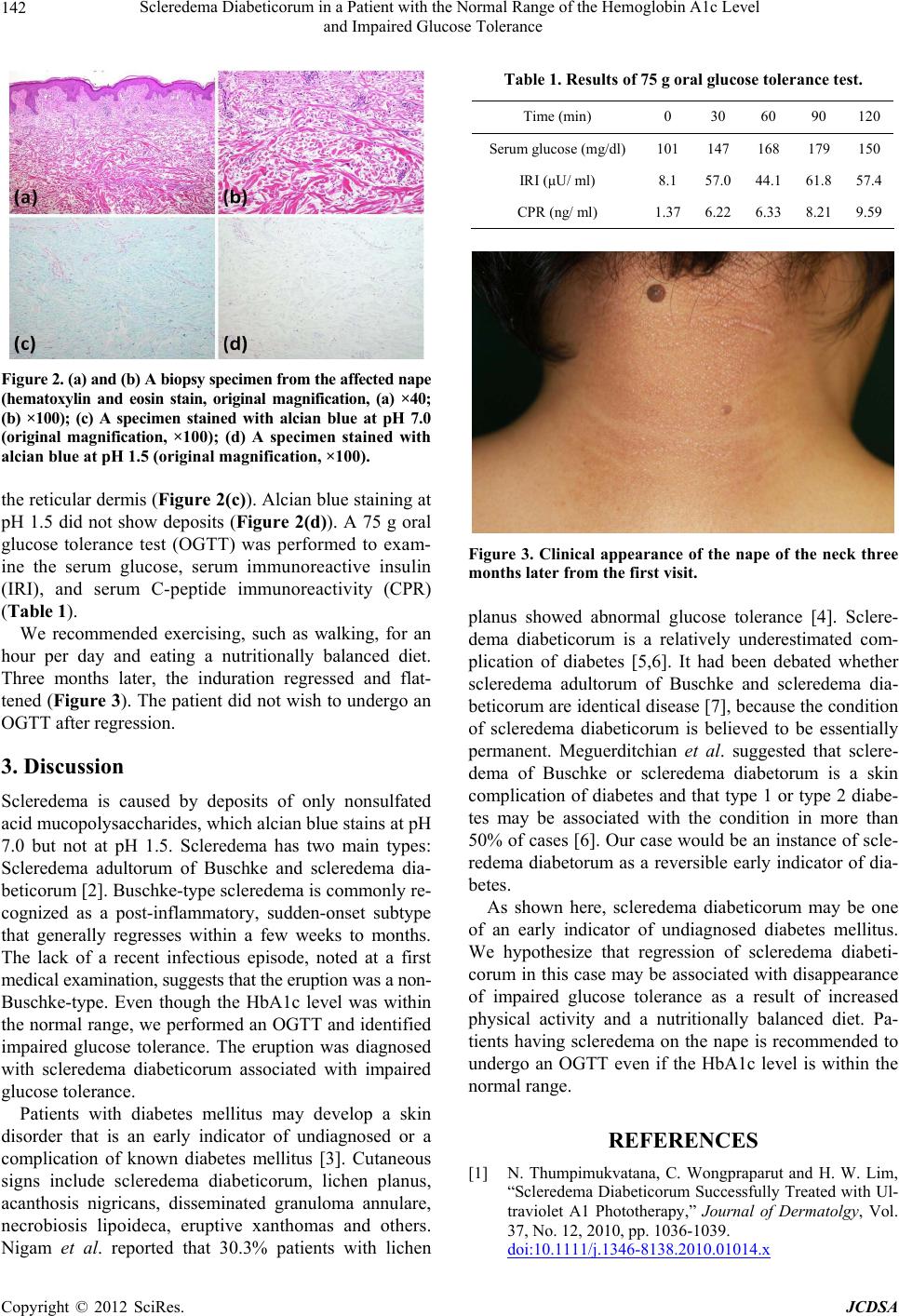
Figure 2. (a) and (b) A biopsy specimen from the affected nape
(hematoxylin and eosin stain, original magnification, (a) ×40;
(b) ×100); (c) A specimen stained with alcian blue at pH 7.0
(original magnification, ×100); (d) A specimen stained with
alcian blue at pH 1.5 (original magnification, ×100).
the reticular dermis (Figure 2(c)). Alcian blue staining at
pH 1.5 did not show deposits (Figure 2(d)). A 75 g oral
glucose tolerance test (OGTT) was performed to exam-
ine the serum glucose, serum immunoreactive insulin
(IRI), and serum C-peptide immunoreactivity (CPR)
(Table 1).
We recommended exercising, such as walking, for an
hour per day and eating a nutritionally balanced diet.
Three months later, the induration regressed and flat-
tened (Figure 3). The patient did not wish to undergo an
OGTT after regression.
3. Discussion
Scleredema is caused by deposits of only nonsulfated
acid mucopolysaccharides, which alcian blue stains at pH
7.0 but not at pH 1.5. Scleredema has two main types:
Scleredema adultorum of Buschke and scleredema dia-
beticorum [2]. Buschke-type scleredema is commonly re-
cognized as a post-inflammatory, sudden-onset subtype
that generally regresses within a few weeks to months.
The lack of a recent infectious episode, noted at a first
medical examination, suggests that the eruption was a non-
Buschke-type. Even though the HbA1c level was within
the normal range, we performed an OGTT and identified
impaired glucose tolerance. The eruption was diagnosed
with scleredema diabeticorum associated with impaired
glucose tolerance.
Patients with diabetes mellitus may develop a skin
disorder that is an early indicator of undiagnosed or a
complication of known diabetes mellitus [3]. Cutaneous
signs include scleredema diabeticorum, lichen planus,
acanthosis nigricans, disseminated granuloma annulare,
necrobiosis lipoideca, eruptive xanthomas and others.
Nigam et al. reported that 30.3% patients with lichen
Table 1. Results of 75 g oral glucose tolerance test.
Time (min) 0 30 60 90 120
Serum glucose (mg/dl) 101 147 168 179150
IRI (μU/ ml) 8.1 57.0 44.1 61.857.4
CPR (ng/ ml) 1.37 6.22 6.33 8.219.59
Figure 3. Clinical appearance of the nape of the neck three
months later from the first visit.
planus showed abnormal glucose tolerance [4]. Sclere-
dema diabeticorum is a relatively underestimated com-
plication of diabetes [5,6]. It had been debated whether
scleredema adultorum of Buschke and scleredema dia-
beticorum are identical disease [7], because the condition
of scleredema diabeticorum is believed to be essentially
permanent. Meguerditchian et al. suggested that sclere-
dema of Buschke or scleredema diabetorum is a skin
complication of diabetes and that type 1 or type 2 diabe-
tes may be associated with the condition in more than
50% of cases [6]. Our case would be an instance of scle-
redema diabetorum as a reversible early indicator of dia-
betes.
As shown here, scleredema diabeticorum may be one
of an early indicator of undiagnosed diabetes mellitus.
We hypothesize that regression of scleredema diabeti-
corum in this case may be associated with disappearance
of impaired glucose tolerance as a result of increased
physical activity and a nutritionally balanced diet. Pa-
tients having scleredema on the nape is recommended to
undergo an OGTT even if the HbA1c level is within the
normal range.
REFERENCES
[1] N. Thumpimukvatana, C. Wongpraparut and H. W. Lim,
“Scleredema Diabeticorum Successfully Treated with Ul-
traviolet A1 Phototherapy,” Journal of Dermatolgy, Vol.
37, No. 12, 2010, pp. 1036-1039.
doi:10.1111/j.1346-8138.2010.01014.x
Copyright © 2012 SciRes. JCDSA