Paper Menu >>
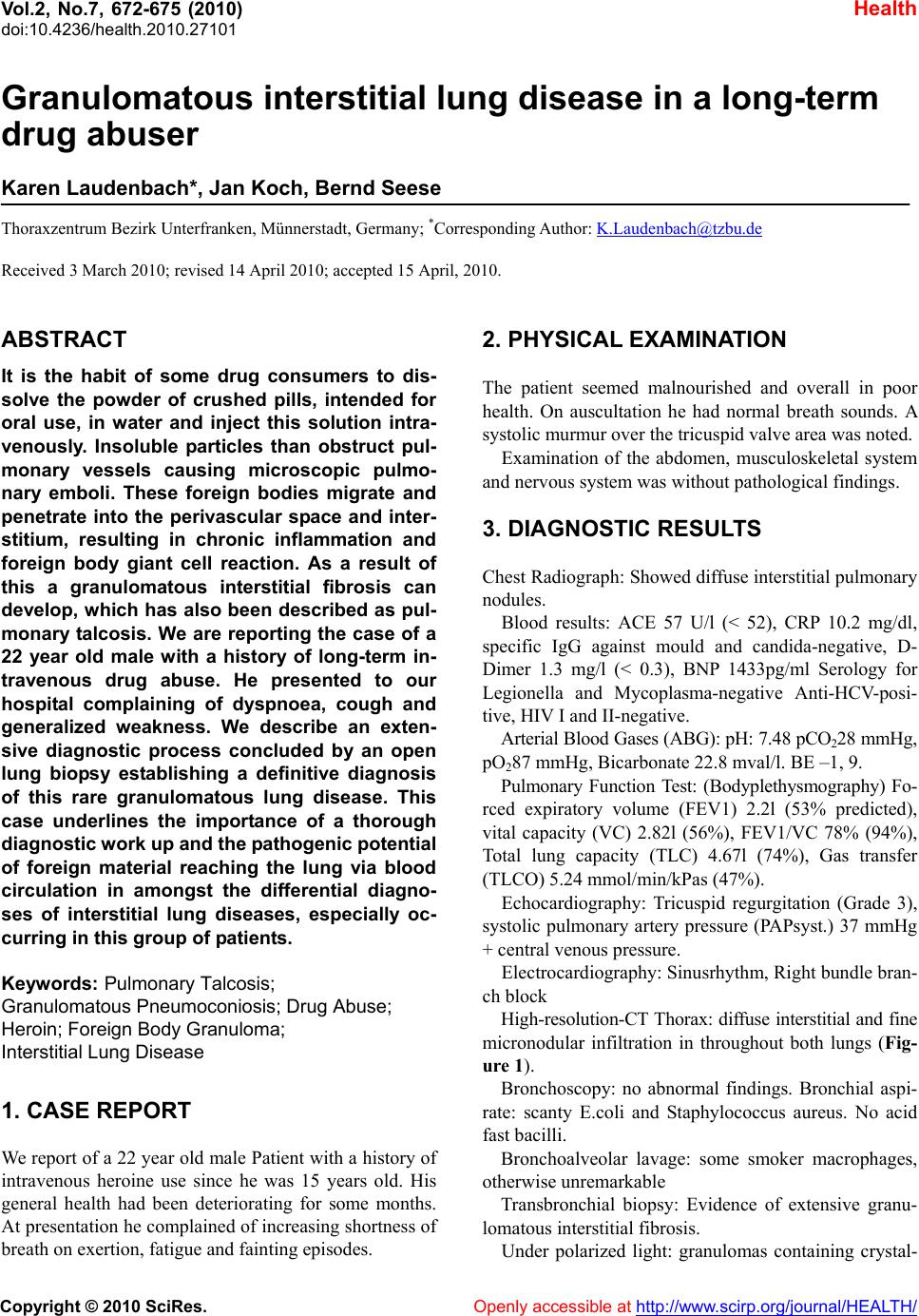
Journal Menu >>
 Vol.2, No.7, 672-675 (2010) doi:10.4236/health.2010.27101 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Health Granulomatous interstitial lung disease in a long-term drug abuser Karen Laudenbach*, Jan Koch, Bernd Seese Thoraxzentrum Bezirk Unterfranken, Münnerstadt, Germany; *Corresponding Author: K.Laudenbach@tzbu.de Received 3 March 2010; revised 14 April 2010; accepted 15 April, 2010. ABSTRACT It is the habit of some drug consumers to dis- solve the powder of crushed pills, intended for oral use, in water and inject this solution intra- venously. Insoluble particles than obstruct pul- monary vessels causing microscopic pulmo- nary emboli. These foreign bodies migrate and penetrate into the perivascular space and inter- stitium, resulting in chronic inflammation and foreign body giant cell reaction. As a result of this a granulomatous interstitial fibrosis can develop, which has also been described as pul- monary talcosis. We are reporting the case of a 22 year old male with a history of long-term in- travenous drug abuse. He presented to our hospital complaining of dyspnoea, cough and generalized weakness. We describe an exten- sive diagnostic process concluded by an open lung biopsy establishing a definitive diagnosis of this rare granulomatous lung disease. This case underlines the importance of a thorough diagnostic work up and the pathogenic potentia l of foreign material reaching the lung via blood circulation in amongst the differential diagno- ses of interstitial lung diseases, especially oc- curring in this group of patients. Keywords: Pulmonary Talcosis; Granuloma tous Pneumoconiosis; Dr u g Abuse; Heroin; Foreign Body Granuloma; Interstitial Lung Disease 1. CASE REPORT We report of a 22 year old male Patient with a history of intravenous heroine use since he was 15 years old. His general health had been deteriorating for some months. At presentation he complained of increasing shortness of breath on exertion, fatigue and fainting episodes. 2. PHYSICAL EXAMINATION The patient seemed malnourished and overall in poor health. On auscultation he had normal breath sounds. A systolic murmur over the tricuspid valve area was noted. Examination of the abdomen, musculoskeletal system and nervous system was without pathological findings. 3. DIAGNOSTIC RESULTS Chest Radiograph: Showed diffuse interstitial pulmonary nodules. Blood results: ACE 57 U/l (< 52), CRP 10.2 mg/dl, specific IgG against mould and candida-negative, D- Dimer 1.3 mg/l (< 0.3), BNP 1433pg/ml Serology for Legionella and Mycoplasma-negative Anti-HCV-posi- tive, HIV I and II-negative. Arterial Blood Gases (ABG): pH: 7.48 pCO228 mmHg, pO287 mmHg, Bicarbonate 22.8 mval/l. BE –1, 9. Pulmonary Function Test: (Bodyplethysmography) Fo- rced expiratory volume (FEV1) 2.2l (53% predicted), vital capacity (VC) 2.82l (56%), FEV1/VC 78% (94%), Total lung capacity (TLC) 4.67l (74%), Gas transfer (TLCO) 5.24 m m ol /m i n/ kPas (47% ). Echocardiography: Tricuspid regurgitation (Grade 3), systolic pulmonary artery pressure (PAPsyst.) 37 mmHg + central venous pre ssure. Electrocardiography: Sinusrhythm, Right bundle bran- ch block High-resolution-CT Thorax: diffuse interstitial and fine micronodular infiltration in throughout both lungs (Fig- ure 1). Bronchoscopy: no abnormal findings. Bronchial aspi- rate: scanty E.coli and Staphylococcus aureus. No acid fast bacilli. Bronchoalveolar lavage: some smoker macrophages, otherwise unremarkable Transbronchial biopsy: Evidence of extensive granu- lomatous interstitial fibro sis. Under polarized light: granulomas containing crystal- 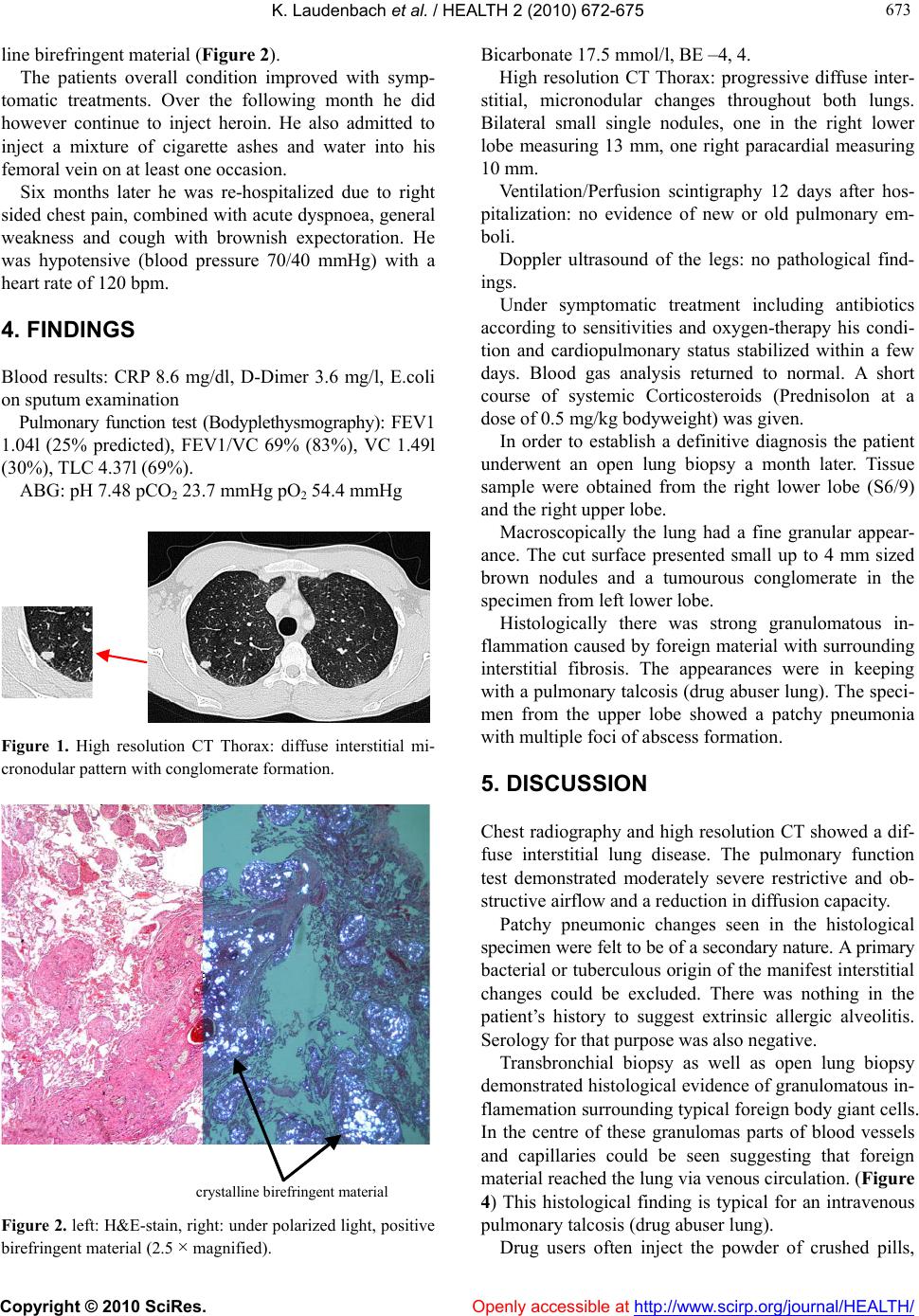 K. Laudenbach et al. / HEALTH 2 (2010) 67 2-675 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 673 673 line birefringent material (Figure 2). The patients overall condition improved with symp- tomatic treatments. Over the following month he did however continue to inject heroin. He also admitted to inject a mixture of cigarette ashes and water into his femoral vein on at least one occasion. Six months later he was re-hospitalized due to right sided chest pain, combined with acute dyspnoea, general weakness and cough with brownish expectoration. He was hypotensive (blood pressure 70/40 mmHg) with a heart rate of 12 0 bpm. 4. FINDINGS Blood results: CRP 8.6 mg/dl, D-Dimer 3.6 mg/l, E.coli on sputum examination Pulmonary function test (Bodyplethysmography): FEV1 1.04l (25% predicted), FEV1/VC 69% (83%), VC 1.49l (30%), TL C 4.37l (69%). ABG: pH 7.48 pCO2 23.7 mmHg pO2 54.4 mmHg Figure 1. High resolution CT Thorax: diffuse interstitial mi- cronodular pattern with conglomerate formation. crystalline bi refri ngent materi al Figure 2. left: H&E-stain, right: under polarized light, positive birefringent material (2.5 × magnified). Bicarbonate 17.5 mmol/l, BE –4, 4. High resolution CT Thorax: progressive diffuse inter- stitial, micronodular changes throughout both lungs. Bilateral small single nodules, one in the right lower lobe measuring 13 mm, one right paracardial measuring 10 mm. Ventilation/Perfusion scintigraphy 12 days after hos- pitalization: no evidence of new or old pulmonary em- boli. Doppler ultrasound of the legs: no pathological find- ings. Under symptomatic treatment including antibiotics according to sensitivities and oxygen-therapy his condi- tion and cardiopulmonary status stabilized within a few days. Blood gas analysis returned to normal. A short course of systemic Corticosteroids (Prednisolon at a dose of 0.5 mg/ kg b odyweight) was gi ven . In order to establish a definitive diagnosis the patient underwent an open lung biopsy a month later. Tissue sample were obtained from the right lower lobe (S6/9) and the right uppe r l obe. Macroscopically the lung had a fine granular appear- ance. The cut surface presented small up to 4 mm sized brown nodules and a tumourous conglomerate in the specimen from left lower lobe. Histologically there was strong granulomatous in- flammation caused by foreign material with surrounding interstitial fibrosis. The appearances were in keeping with a pulmonary talcosis (drug abuser lung). The speci- men from the upper lobe showed a patchy pneumonia with multiple foci of abscess formation. 5. DISCUSSION Chest radiography and high resolution CT showed a dif- fuse interstitial lung disease. The pulmonary function test demonstrated moderately severe restrictive and ob- structive airflow and a reduction in diffusion capacity. Patchy pneumonic changes seen in the histological specimen were felt to be of a secondary nature. A primary bacterial or tuberculous origin of the manifest interstitial changes could be excluded. There was nothing in the patient’s history to suggest extrinsic allergic alveolitis. Serology for that purpose was also negative. Transbronchial biopsy as well as open lung biopsy demonstrated histological evidence of granulomatous in- flamemation surrounding typical foreign body giant cells. In the centre of these granulomas parts of blood vessels and capillaries could be seen suggesting that foreign material reached the lung via venous circulation. (Figure 4) This histological finding is typical for an intravenous pulmonary talcosis (drug abuser lung). Drug users often inject the powder of crushed pills, 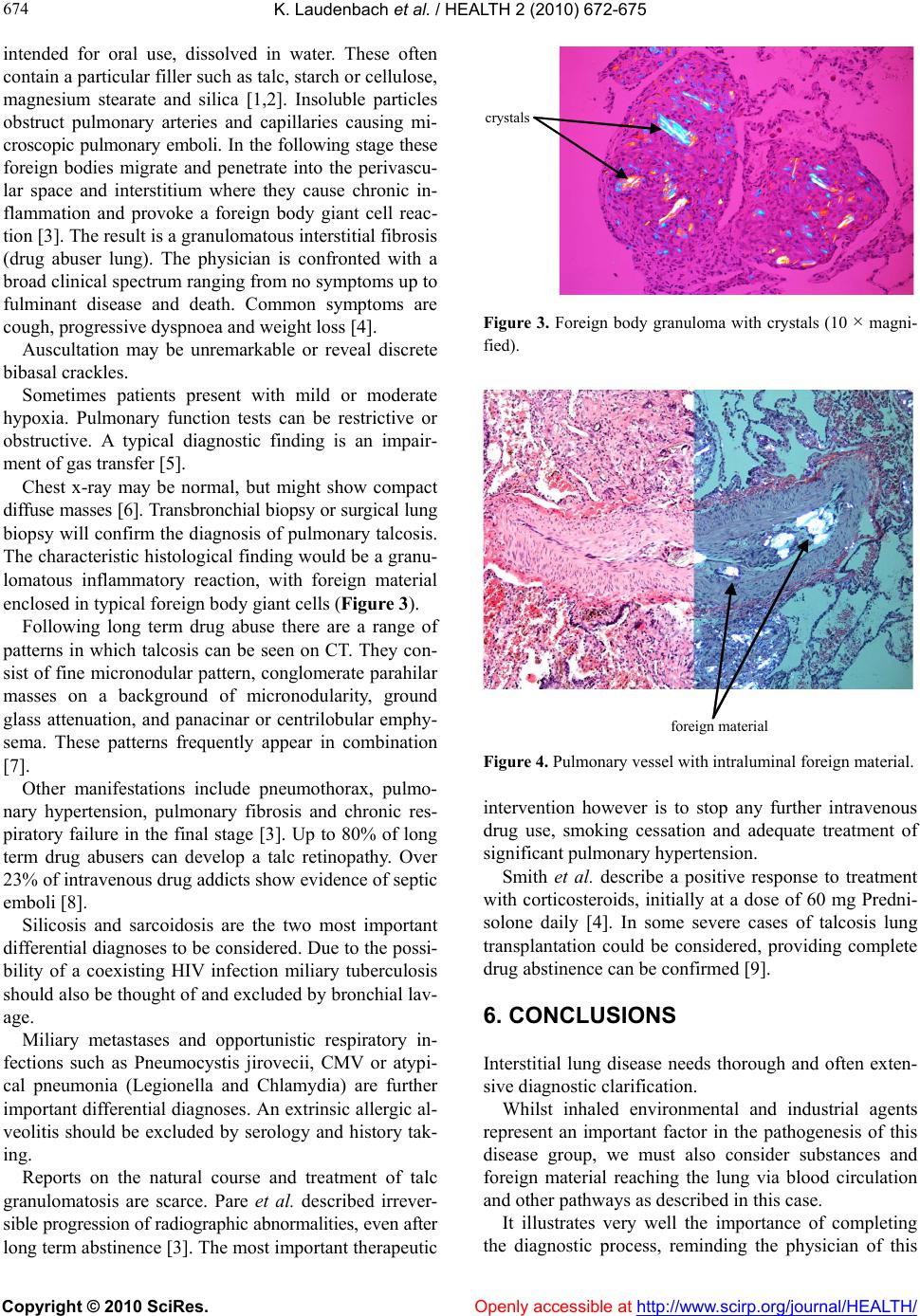 K. Laudenbach et al. / HEALTH 2 (2010) 67 2-675 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 674 intended for oral use, dissolved in water. These often contain a particular filler such as talc, starch o r cellulose, magnesium stearate and silica [1,2]. Insoluble particles obstruct pulmonary arteries and capillaries causing mi- croscopic pulmonary emboli. In the following stage these foreign bodies migrate and penetrate into the perivascu- lar space and interstitium where they cause chronic in- flammation and provoke a foreign body giant cell reac- tion [3]. The result is a gr anu lo matous in terstitial fib r o sis (drug abuser lung). The physician is confronted with a broad clinical spectrum ranging from no symptoms up to fulminant disease and death. Common symptoms are cough, progressive dyspnoea and weight loss [4]. Auscultation may be unremarkable or reveal discrete bibasal crackles. Sometimes patients present with mild or moderate hypoxia. Pulmonary function tests can be restrictive or obstructive. A typical diagnostic finding is an impair- ment of gas transfer [5]. Chest x-ray may be normal, but might show compact diffuse masses [6]. Transbronchial biopsy or surgical lung biopsy will confirm the diagno sis of pulmonary talcosis. The characteristic histological finding would be a granu- lomatous inflammatory reaction, with foreign material enclosed in typical foreign body giant cells (Figure 3). Following long term drug abuse there are a range of patterns in which talcosis can be seen on CT. They con- sist of fine micronodular pattern, conglomerate parahilar masses on a background of micronodularity, ground glass attenuation, and panacinar or centrilobular emphy- sema. These patterns frequently appear in combination [7]. Other manifestations include pneumothorax, pulmo- nary hypertension, pulmonary fibrosis and chronic res- piratory failure in the final stage [3]. Up to 80% of long term drug abusers can develop a talc retinopathy. Over 23% of intrav en ou s drug add icts show evid en ce of sep tic emboli [8]. Silicosis and sarcoidosis are the two most important differential diagno ses to be considered . Due to the po ssi- bility of a coexisting HIV infection miliary tuberculosis should also be thought of and excluded by bronchial lav- age. Miliary metastases and opportunistic respiratory in- fections such as Pneumocystis jirovecii, CMV or atypi- cal pneumonia (Legionella and Chlamydia) are further important differential diagnoses. An extrinsic allergic al- veolitis should be excluded by serology and history tak- ing. Reports on the natural course and treatment of talc granulomatosis are scarce. Pare et al. described irrever- sible progression of radiographic abnormalities, even after long term abstinence [3]. The most important therap eutic crystals Figure 3. Foreign body granuloma with crystals (10 × magni- fied). forei g n material Figure 4. Pulmonary vessel with intraluminal foreign material. intervention however is to stop any further intravenous drug use, smoking cessation and adequate treatment of significant pu lmonary hypertension. Smith et al. describe a positive response to treatment with corticosteroids, initially at a dose of 60 mg Predni- solone daily [4]. In some severe cases of talcosis lung transplantation could be considered, providing complete drug abstinence can be confirmed [9]. 6. CONCLUSIONS Interstitial lung disease needs thorough and often exten- sive diagnostic clarification. Whilst inhaled environmental and industrial agents represent an important factor in the pathogenesis of this disease group, we must also consider substances and foreign material reaching the lung via blood circulation and other pathways as described in this case. It illustrates very well the importance of completing the diagnostic process, reminding the physician of this 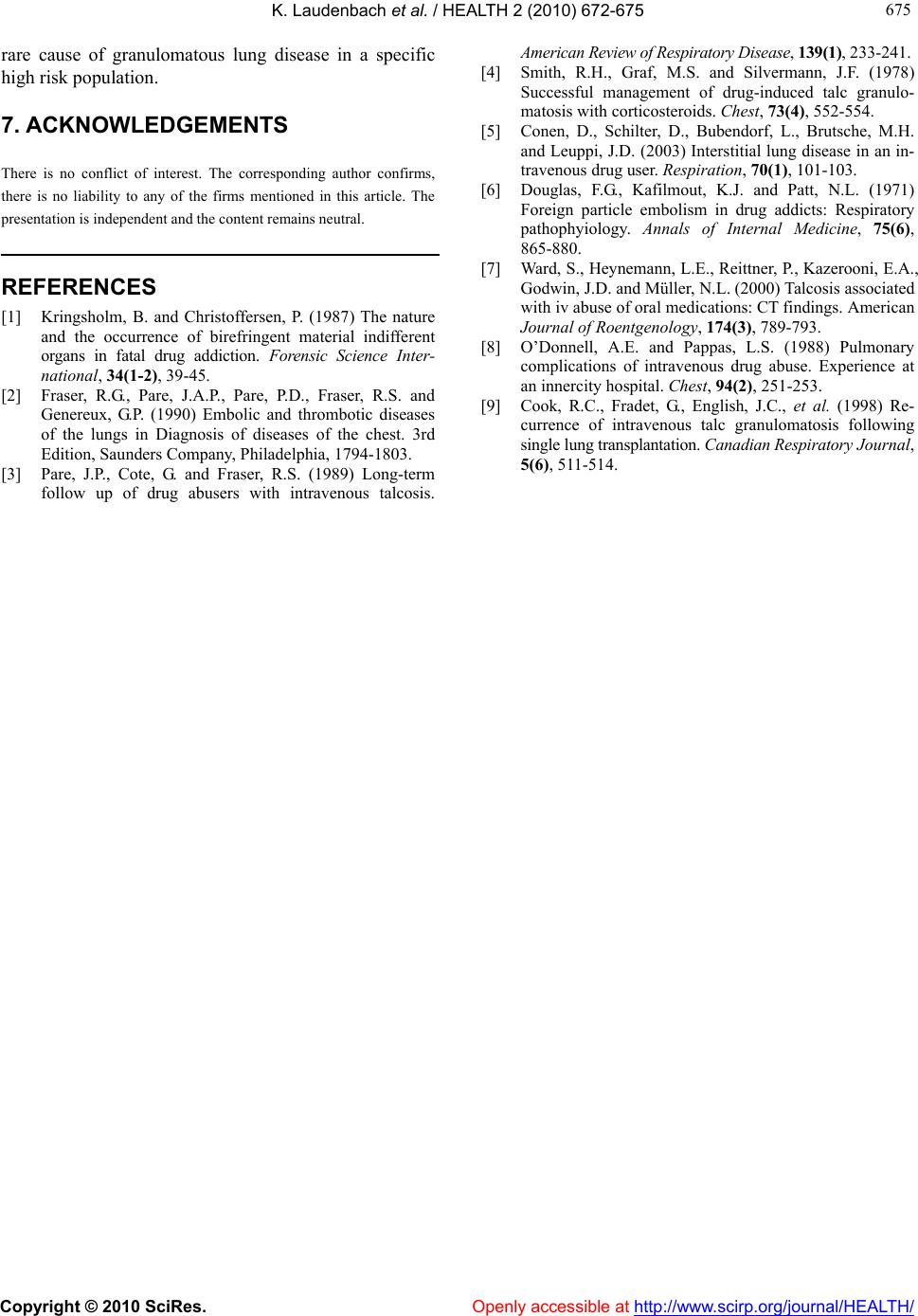 K. Laudenbach et al. / HEALTH 2 (2010) 67 2-675 Copyright © 2010 SciRes. http://www.scirp.org/journal/HEALTH/ 675 675 rare cause of granulomatous lung disease in a specific high risk population. Openly accessible at 7. ACKNOWLEDGEMENTS There is no conflict of interest. The corresponding author confirms, there is no liability to any of the firms mentioned in this article. The presentation is independent and the conten t remains neutral. REFERENCES [1] Kringsholm, B. and Christoffersen, P. (1987) The nature and the occurrence of birefringent material indifferent organs in fatal drug addiction. Forensic Science Inter- national, 34(1-2), 39-45. [2] Fraser, R.G., Pare, J.A.P., Pare, P.D., Fraser, R.S. and Genereux, G.P. (1990) Embolic and thrombotic diseases of the lungs in Diagnosis of diseases of the chest. 3rd Edition, Saunders Company, Philadelphia, 1794-1803. [3] Pare, J.P., Cote, G. and Fraser, R.S. (1989) Long-term follow up of drug abusers with intravenous talcosis. American Review of Respiratory Disease, 139(1), 233-241. [4] Smith, R.H., Graf, M.S. and Silvermann, J.F. (1978) Successful management of drug-induced talc granulo- matosis with corticosteroids. Chest, 73(4), 552-554. [5] Conen, D., Schilter, D., Bubendorf, L., Brutsche, M.H. and Leuppi, J.D. (2003) Interstitial lung disease in an in- travenous drug user. Respiration, 70(1), 101-103. [6] Douglas, F.G., Kafilmout, K.J. and Patt, N.L. (1971) Foreign particle embolism in drug addicts: Respiratory pathophyiology. Annals of Internal Medicine, 75(6), 865-880. [7] Ward, S., Heynema nn, L.E., Reittner, P. , Kazerooni, E.A., Godwin, J.D. and Müller, N.L. (2000) Talcosis associated with iv abuse of oral medications: CT findings. American Journal of Roentgenology, 174(3), 789-793. [8] O’Donnell, A.E. and Pappas, L.S. (1988) Pulmonary complications of intravenous drug abuse. Experience at an innercity hospital. Chest, 94(2), 251-253. [9] Cook, R.C., Fradet, G., English, J.C., et al. (1998) Re- currence of intravenous talc granulomatosis following single lung transplantation. Canadian Respiratory Journal, 5(6), 511-514. |

