Health
Vol.6 No.10(2014), Article ID:44903,8 pages DOI:10.4236/health.2014.610129
Dyslipidaemias and Physical Activity in Children with Cerebral Palsy
Maciste Habacuc Macías-Cervantes1, Martha Susana Arriola-Nuñez2, Francisco J. Díaz-Cisneros3, Antonio E. Rivera-Cisneros4, José María de la Roca-Chiapas5, Victoriano Pérez-Vázquez1*
1Departamento de Ciencias Médicas, División de Ciencias de la Salud, Universidad de Guanajuato, León, México
2Universidad del Valle de Atemajac, Guadalajara, México
3Departamento de Ciencias Aplicadas al Trabajo, División de Ciencias de la Salud, Universidad de Guanajuato, León, México
4División de Ciencias de la Salud, Universidad de Guanajuato, León, México
5Departamento Psicología, División de Ciencias de la Salud, Universidad de Guanajuato, León, México
Email: *vpvazquez@ugto.mx
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 2 March 2014; revised 5 April 2014; accepted 12 April 2014
ABSTRACT
Cerebral palsy people present movement difficulty and are liable to develop disorders associated with sedentary lifestyles such as dyslipidaemias and cardiovascular diseases. This study aimed to assess physical activity and the prevalence of lipid abnormalities in 29 children with cerebral palsy who were being treated in two care centers in the state of Guanajuato, Mexico. Physical activity was calculated using a survey. Blood glucose, total cholesterol, HDL-C, LDL-C, and triglycerides were determined. Forty-eight percent had at least one dyslipidaemia. The most frequent lipid abnormalities were hypertriglyceridaemia and low HDL-C. High prevalence of the atherogenic index was found. The physical activity of children was lower than recommended for their age. Sixty-two percent attended rehabilitation sessions, 10% attended sports classes, 14% rehabilitation plus sports and 14% did not engage in intentional physical activity. There is high frequency of lipid disorders in children with cerebral palsy. Greater participation in physical activity should be promoted in children to improve their metabolic status and quality of life, especially those suffering from cerebral palsy.
Keywords
Hypertriglyceridaemia, HDL-C, Atherogenic Index

1. Introduction
Increased life expectancy and increasing non-transmittable diseases will raise demand for care services and programs for certain populations [1] . Cerebral palsy (CP) is a static encephalopathy defined as a non-progressive disorder of posture and movements, often accompanied by epilepsy and language disorders, vision and intelligence disorders. This condition is due to a defect or injury in the developing brain [2] . People with CP present health complications such as neurological, digestive, vision, hearing and locomotor system difficulties. Feeding problems are the most common in children with cerebral palsy, which causes an inadequate energy intake [3] . In assessing children with CP a high prevalence of chronic malnutrition manifested by growth retardation is common, as are deficiencies in the intake of micronutrients [4] . Although the relationship between CP and proteincalorie malnutrition is known, there is little information about the reality of this relationship in developing countries.
Muscle contractures are the most common alteration in people with CP causing a decrease in their mobility [2] . Young people with disabilities do not realize the amount of exercise recommended for the healthy young, thereby increasing their risk of developing disorders associated with a sedentary lifestyle [5] . McMurray conducted a longitudinal study in which healthy adolescents showed that low physical activity increases their risk of developing metabolic disorders [6] .
In the last ten years an increase in the prevalence of obesity in children with cerebral palsy has been observed [7] . There is scanty information on metabolic disorders in people with CP. Some authors have reported the presence of osteoporosis [8] [9] . Dyslipidaemia is a set of alterations, which include high levels of total cholesterol, LDL-C and triglycerides and low levels of HDL-C. Dyslipidaemia is associated with obesity. However, not only obese people have dyslipidaemia. The literature describes this syndrome as affecting people who are “metabolically obese with normal weight”. In laboratory tests increased glucose, total cholesterol, triglycerides and decreased HDL-C levels have been found. This syndrome is present in 5% to 45% of the general population [10] . Mexico has shown a high prevalence of dyslipidaemia in adults [11] . In 2004 Moran reported 9.5% of hypertriglyceridaemia and 20% of low HDL-C in a group of adolescents in Mexico [12] . Because people with CP have difficulty to move they are prone to dyslipidaemia. The aim of this study was to evaluate the lifestyle in children with cerebral palsy and its impact on health.
2. Methods
2.1. Subjects
We evaluated the state of health, nutrition and physical activity in 29 children with CP diagnosis in two multiple care centers in the state of Guanajuato between January and July 2011. Twelve children went to the Multiple Assistance Center rural area, San Felipe Torres Mochas, and 58.7% (17 children) from the urban area of Leon City. Children from 2 to 13 years of both genders (13 men, 16 women) were included.
2.2. Procedure
Permission from managers to carry out the study in multiple centers in the municipalities of San Felipe and León, Guanajuato was required. Family members or tutors of children were fully informed of the purpose and procedure of the study. Parents signed an informed consent form, and verbal consent was also sought from participants. The protocol was adhered to established ethical guidelines for persons with mental or physical disability.
At the first visit, a complete medical history, 24-hour recall and physical assessment were performed. Anthropometric evaluation was performed by a certified anthropometrist following the recommendations of the International Society for the Advance of Kinanthropometry (ISAK). When the children were unable to stand, the length of the tibia (LT) of the right leg was measured, the height was obtained using the formula (3.26 × LT) + 8.30 [13] . In order to classify the BMI, were used the cut off points suggested for children with CP [14] .
2.3. Classification of Motor Function
The severity of CP was classified according to the classification system for gross motor function (GMFCS) and the capacity for selective motor control (SCM) [15] . The GMFCS is a classification system with 5 levels according to age. Distinction between the levels of motor function is based on functional limitations, the need for supportive devices, and the quality of movement. Level 1) Children that walk in and out of home, climb stairs without limitations. Level 2) Children, who walk in and out of home, climb stairs with support, but experience difficulty walking on irregular surfaces and slopes. Level 3) Children that walks with the assistance of a device inside and out of home, but do not climb stairs. Level 4) Children who travel in wheelchairs before the age of six. Level 5) Children physically restrained to maintain the posture of the trunk and head. To determine the degree of SCM participants were sat and asked to extend the knee and then perform a dorsiflexion, the evaluation was conducted on both legs. The score was assigned according to van Eck and the result is expressed in categories of poor, moderate and good selective control [16] .
2.4. Physical Activity
The information was obtained using a questionnaire. For the present study intentional physical activity in a sport or rehabilitation assistance program was considered. Relatives of the participants were asked the number of sessions conducted per week for children taking into account the rehabilitation and sports attendance, and the duration of each session. We report the average number of minutes of these activities per week. Then we subdivided the group into appropriate frequency of physical activity if the child performed at least 3 sessions of 30 minutes a week.
2.5. Metabolic Evaluation
We checked children at their rehabilitation centers and asked parents not to give any food after 21:00 hours the day before the review. It took 12 ml of blood from the antecubital vein. The samples were refrigerated for transport and all tests were performed before 10:00 hours. The blood chemistry tests were performed at Department of Applied Work Sciences. Glucose was measured using glucose oxidase/peroxidase method (Spinreact, interassay CV 1.2%, interassay CV 2.7%), and the total cholesterol and triglycerides by enzymatic colorimetric method (CV Spinreact interaensayo 0.71%, CV interassay CV 1.4% and interaenssay 0.6%, interassay CV 1.8% respectively). HDL fraction was determined by spectrophotometry at 505 nM (CV Spinreact interassay 1.1%, interassay CV 2.72%). LDL fraction was calculated according to the Friedewald formula. The classification of dyslipidaemias was performed based on the age and sex cutoff points, according to the American Academy of Pediatrics [17] . In addition, the atherogenic index was calculated by dividing the total cholesterol/HDL-C. This index is considered a cardiovascular risk estimator, and it was interpreted as high when the score was 4.5 or 5.0 for women and men, respectively.
2.6. Statistical Analysis
The analysis was performed in Stat soft look 7.0. A comparison of continuous variables was performed using a Student’s T test. The data was presented in tables and figures, reporting percentages, mean and standard deviation.
3. Results
Twenty nine participants (13 male and 16 women) were evaluated and 100% had bilateral motor condition. A child was fed through a gastrostomy tube, whilst the rest of the children were able to swallow.
The general characteristics of the participants are shown in Table 1. The average age was 8. The group from Leon was older and taller compared to the group of children from San Felipe (p < 0.05).
3.1. Motor Function
Table 2 shows the characteristics of the gross and selective motor function. Seventeen participants had the maximum degree of disability of the gross motor function (level 5). Seven participants depended on some form of mobilization (levels 3 and 4), and 5 were able to walk without difficulty (level 2). Forty eight percent of the population studied presented poor selective motor control, 25% moderate and only 27% had adequate selective control.
3.2. Anthropometric Measure
Anthropometric measurements were conducted under ISAK rules. The technical error rate was 2.6%. Most participants were classified as underweight (59%). Overweight children were a minority (3%) and the rest had normal weight (38%).
Taking into account the triceps skinfold, 7% had mild deficits, 45% moderate deficiency and 45% severe deficit. Only 3% were classified as normal weight according to triceps skinfold. When comparing groups from Leon and San Felipe no significant differences in BMI, weight, and triceps skinfold thickness were found (Table 1).
3.3. Physical Activity
Sixty two percent of children evaluated went to rehab sessions, 10% to sports lessons, 14% to rehabilitation sessions in addition to sports classes and 14% did no intentional physical activity. Only 21% of subjects tested did more than 3 workouts per week. The most frequent activities were rehabilitation, walking and swimming. Three children have participated in Special Olympics Games. The group averaged 135.3 ± 79.6 total min/week of intentional physical activity, no difference was found when comparing the time of activity between the groups (Table 1).
Table 1. General characteristics of participants.
PTC, triceps skinfold. BMI, body mass index. AI, atherogenic index.
Table 2. Classification of motor function in participants.
Classification of motor function as described in methods.
3.4. Biochemical Evaluation
The results of the hematic biometry were within normal ranges. Two children had glucose levels higher than 126 mg/dL confirmed on 2 occasions. Lipid levels are described in Table 1. When comparing groups, children from San Felipe showed higher levels of HDL-C (p = 0.03), the remaining variables showed no difference. The classification of dyslipidaemias is shown in Figure 1. Fifty two percent of the children studied did not have dyslipidaemia, 22% had a dyslipidaemia, 17% two and 9% had 3 dyslipidaemias. The most frequent dyslipidaemias were low HDL-C and triglycerides (Table 3). In analyzing the atherogenic index we found that 5 (22%) children have higher risk of developing cardiovascular disease in the future.
4. Discussion
The results of this study showed a high prevalence of dyslipidaemias and low levels of intentional physical activity in children with CP. Cardiovascular disease prevention should begin in childhood because lipid levels in childhood are associated with intima-media thickness in the carotid arteries in adulthood so that the higher the level of lipids the greater the risk of developing cardiovascular disease [18] . In this study, the population diagnosed with dyslipidaemia was 48% of children, higher than 37% of dyslipidaemia in Mexican adolescents. Marcos-Daccarett studied the prevalence of dyslipidaemias in adolescents with normal weight (20.8%) and obese (56.6%) separately. It is noteworthy that studied children with CP showed double the prevalence of dyslipidaemia compared to normal weight children studied by Marcos-Daccarett in the north of México [19] . In calculating the atherogenic index, which is an estimate of cardiovascular risk, we found that 22% of the population in the study was at increased risk, in line with what has been reported for Colombian children. However, 14% of the population studied by Uscategui in Colombia had higher weight (overweight or obesity) and thus we believe that children with CP present prevalence of dyslipidaemia similar to those from children who are overweight or obese [20] .
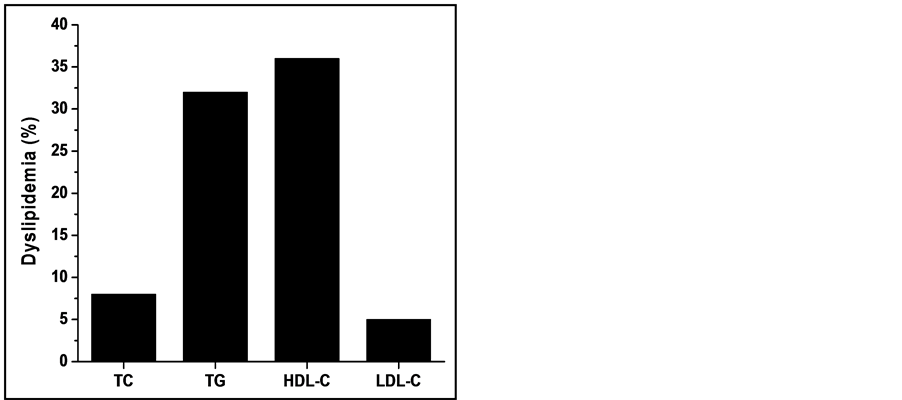
Figure 1. Prevalence of dyslipidaemias in participants. TC, total cholesterol. TG, Triglycerides.
Table 3. Distribution of dyslipidaemias.
Data are expressed in numbers of cases. *Not enough sample data.
Dyslipidaemia involves risk factors for developing hypertension [21] , specifically elevated triglyceride levels that increase the risk of developing cardiovascular disease [22] . Hypertriglyceridaemia was one of the most prevalent lipid abnormalities in children with CP. This is in line with those reported by Buchaka et al., who studied a group of diabetic children with low physical activity [23] . In a group of children studied in Guadalajara a positive association between triglycerides levels and serum insulin was found. HDL levels were also associated inversely with serum insulin levels [24] . Previous studies lay the groundwork for a potential development of hypertension and endothelial injury through the phenomenon of insulin resistance in children with CP and dyslipidaemia.
Low levels of HDL-C increased the prevalence of cardiovascular diseases, the above becomes an important therapeutic target in early prevention of diseases [25] . A review showed that aerobic exercise in adults promotes the reduction of triglycerides and total cholesterol while increasing HDL-C [26] . Serum lipid levels can be modified through diet or exercise; however, a randomized clinical study showed that HDL-C levels are increased in children when they have changes in diet and exercise programs, but they do not increase if only diet is used [27] . It has also been shown that physical activity, even low-intensity, decreases non-HDL cholesterol and triglycerides, and increases HDL cholesterol levels in animal models and humans [26] [28] .
58% of children studied had high dependency for mobility (level V GSMCS), so dependent on help from relatives for their activities. On average these children spent 135 minutes/week doing physical activity. “The Declaration of Acapulco” suggests that Mexican children to do at least 150 minutes/week of physical activity [29] . Children from the Leon city group met the average recommended time, unlike the children from San Felipe. It is worth clarifying that the “Declaration of Acapulco” sets the minimum time recommended to preserve the health of a child without limiting mobility. A recent study showed that training 210 minutes/week, combining aerobic and anaerobic activities, improved maximum oxygen consumption (VO2 max) and mobility thick (GSMCS) in adolescents with CP [30] . Therefore more research should be conducted to determine if training for 210 minutes/week can improve the metabolic profile in children with CP and dyslipidaemia. Exercise programs in children with CP have been shown to improve physical ability, level of participation and quality of life for participants [30] -[32] . In this sense we should emphasize the importance of promoting physical activity in children with CP and low HDL-C. One of the most common lipid abnormalities in children with CP was low HDL-C. Children with CP may benefit from an appropriate exercise program to improve neuromuscular coordination and potentially improve metabolic control. For future researches it is recommended to include a high number of facilities in order to have a representative sample. Add the nutrition habits of children should be evaluated to design best interventions and improvement the quality of life in children with CP.
5. Conclusion
The results of this study show a high prevalence of dyslipidaemias and little time spent doing intentional physical activity in children with cerebral palsy. Greater participation in physical activity should be promoted for children with CP to improve their metabolic state and quality of life.
Acknowledgements
This research was funded by the State Committee for Sports and Youth Care of the State of Guanajuato and the Department of Medical Science of the University of Guanajuato. The authors acknowledge the Office of Research and Postgraduate Support (Dirección de Apoyo a la Investigación y Posgrado, DAIP) of the University of Guanajuato for the editing of the English-language version of this paper.
References
- Organización Panamericana de la Salud (OPS) y Organización Mundial de la Salud (OMS) (2006) 138a sesión del comité ejecutivo. www.amro.who.int
- Krigger, K.W. (2006) Cerebral Palsy: An Overview. American Family Physician, 73, 91-100.
- Hogan, S.E. (2004) Energy Requirements of Children with Cerebral Palsy. Canadian Journal of Dietetic Practice and Research, 65, 124-130. http://dx.doi.org/10.3148/65.3.2004.124
- Hillesund, E., Skranes, J., Trygg, K.U. and Bohmer, T. (2007) Micronutrient Status in Children with Cerebral Palsy. Acta Paediatrica, 96, 1195-1198. http://dx.doi.org/10.1111/j.1651-2227.2007.00354.x
- Rimmer, J.A. and Rowland, J.L. (2008) Physical Activity for Youth with Disabilities: A Critical Need in an Underserved Population. Developmental Neurorehabilitation, 11, 141-148. http://dx.doi.org/10.1080/17518420701688649
- McMurray, R.G., Bangdiwala, S.I., Harrell, J.S. and Amorim, L.D. (2008) Adolescents with Metabolic Syndrome Have a History of Low Aerobic Fitness and Physical Activity Levels. Dynamic Medicine, 7, 5. http://dx.doi.org/10.1186/1476-5918-7-5
- Rogozinski, B.M., Davids, J.R., Davis, R.B., Christopher, L.M., Anderson, J.P., Jameson, G.G. and Blackhurst, D.W. (2007) Prevalence of Obesity in Ambulatory Children with Cerebral Palsy. The Journal of Bone and Joint Surgery, 89, 2421-2426. http://dx.doi.org/10.2106/JBJS.F.01080
- Turk, M.A., Scandale, J., Rosenbaum, P.F. and Weber, R.J. (2001) The Health of Women with Cerebral Palsy. Physical Medicine and Rehabilitation Clinics of North America, 12, 153-168.
- Plotkin, H. and Sueiro, R. (2007) Osteoporosis in Children with Neuromuscular Diseases and Inborn Errors of Metabolism. Minerva Pediatrica, 59, 129-135.
- Conus, F., Rabasa-Lhoret, R. and Peronnet, F. (2007) Characteristics of Metabolically Obese Normal-Weight (MONW) Subjects. Applied Physiology, Nutrition, and Metabolism, 32, 4-12. http://dx.doi.org/10.1139/h06-092
- Aguilar-Salinas, C.A., Gomez-Perez, F.J., Rull, J., Villalpando, S., Barquera, S. and Rojas, R. (2010) Prevalence of Dyslipidemias in the Mexican National Health and Nutrition Survey 2006. Salud Publica de Mexico, 52, S44-S53. http://dx.doi.org/10.1590/S0036-36342010000700008
- Rodriguez-Moran, M., Salazar-Vazquez, B., Violante, R. and Guerrero-Romero, F. (2004) Metabolic Syndrome among Children and Adolescents Aged 10 - 18 Years. Diabetes Care, 27, 2516-2517. http://dx.doi.org/10.2337/diacare.27.10.2516
- Stevenson, R.D. (1995) Use of Segmental Measures to Estimate Stature in Children with Cerebral Palsy. Archives of Pediatrics & Adolescent Medicine, 149, 658-662. http://dx.doi.org/10.1001/archpedi.1995.02170190068012
- Day, S.M., Strauss, D.J., Vachon, P.J., Rosenbloom, L., Shavelle, R.M. and Wu, Y.W. (2007) Growth Patterns in a Population of Children and Adolescents with Cerebral Palsy. Developmental Medicine and Child Neurology, 49, 167-171. http://dx.doi.org/10.1111/j.1469-8749.2007.00167.x
- Palisano, R., Rosenbaum, P., Walter, S., Russell, D., Wood, E. and Galuppi, B. (1997) Development and Reliability of a System to Classify Gross Motor Function in Children with Cerebral Palsy. Developmental Medicine and Child Neurology, 39, 214-223. http://dx.doi.org/10.1111/j.1469-8749.1997.tb07414.x
- van Eck, M., Dallmeijer, A.J., Beckerman, H., van den Hoven, P.A., Voorman, J.M. and Becher, J.G. (2008) Physical Activity Level and Related Factors in Adolescents with Cerebral Palsy. Pediatric Exercise Science, 20, 95-106.
- Daniels, S.R., Greer, F.R. and the Committee on Nutrition (2008) Lipid Screening and Cardiovascular Health in childhood. Pediatrics, 122, 198-208. http://dx.doi.org/10.1542/peds.2008-1349
- Raitakari, O.T., Juonala, M., Kahonen, M., Taittonen, L., Laitinen, T., Maki-Torkko, N., Jarvisalo, M.J., Uhari, M., Jokinen, E., Ronnemaa, T., Akerblom, H.K. and Viikari, J.S. (2003) Cardiovascular Risk Factors in Childhood and Carotid Artery Intima-Media Thickness in Adulthood: The Cardiovascular Risk in Young Finns Study. The Journal of the American Medical Association, 290, 2277-2283. http://dx.doi.org/10.1001/jama.290.17.2277
- Marcos-Daccarett, N.J., Nunez-Rocha, G.M., Salinas-Martinez, A.M., Santos-Ayarzagoitia, M. and Decanini-Arcaute, H. (2007) Obesity as Risk Factor for Metabolic Disorder in Mexican Adolescents, 2005. Revista de Salud Publica, 9, 180-193. http://dx.doi.org/10.1590/S0124-00642007000200003
- Uscátegui Peáuela, R.M., Álvarez Uribe, M.C., Laguado Salinas, I., Soler Terranova, W., Martinez Maluendas, L., Arias Arteaga, R., Duque Jaramillo, B., Pérez Giraldo, J. and Camacho Pérez, J.A. (2003) Cardiovascular Risk Factors in Children and Teenagers Aged 6-18 Years Old from Medellin (Colombia). Anales de Pediatria, 58, 411-417. http://dx.doi.org/10.1016/S1695-4033(03)78086-2
- Takase, H., Dohi, Y., Toriyama, T., Okado, T., Tanaka, S., Sato, K. and Kimura, G. (2008) Metabolic Disorders Predict Development of Hypertension in Normotensive Japanese Subjects. Hypertension Research, 31, 665-671. http://dx.doi.org/10.1291/hypres.31.665
- Shimano, H., Arai, H., Harada-Shiba, M., Ueshima, H., Ohta, T., Yamashita, S., Gotoda, T., Kiyohara, Y., Hayashi, T., Kobayashi, J., Shimamoto, K., Bujo, H., Ishibashi, S., Shirai, K., Oikawa, S., Saito, Y. and Yamada, N. (2008) Proposed Guidelines for Hypertriglyceridemia in Japan with Non-HDL Cholesterol as the Second Target. Journal of Atherosclerosis and Thrombosis, 15, 116-121. http://dx.doi.org/10.5551/jat.E560
- Muchacka-Bianga, M., Deja, G., Jarosz-Chobot, P., Malecka-Tendera, E., Kalina, M. and Grychtol, M. (2006) Evaluation of Selected Risk Factors of Atherosclerosis in Children with Type 1 Diabetes Mellitus and Hypercholesterolemia. Endokrynologia, 12, 25-30.
- Ramirez-Lopez, G., Gonzalez-Villalpando, C., Salmeron, J., Gonzalez-Ortiz, M. and Valles-Sanchez, V. (2006) Triglycerides and High-Density Lipoprotein Cholesterol Are Associated with Insulinemia in Adolescents. Salud Pública de México, 48, 293-299. http://dx.doi.org/10.1590/S0036-36342006000400003
- Langslet, G. and Reikvam, A. (2008) Can Cardiovascular Events Be Prevented by Raising HDL Cholesterol? Tidsskrift for den Norske Laegeforening, 128, 1519-1523.
- Kelley, G.A., Kelley, K.S. and Tran, Z.V. (2005) Walking and Non-HDL-C in Adults: A Meta-Analysis of Randomized Controlled Trials. Preventive Cardiology, 8, 102-107. http://dx.doi.org/10.1111/j.1520-037X.2005.3474.x
- Parente, E.B., Guazzelli, I., Ribeiro, M.M., Silva, A.G., Halpern, A. and Villares, S.M. (2006) Obese Children Lipid Profile: Effects of Hypocaloric Diet and Aerobic Physical Exercise. Arquivos Brasileiros de Endocrinologia e Metabologia, 50, 499-504. http://dx.doi.org/10.1590/S0004-27302006000300013
- Sun, M.W., Qian, F.L., Wang, J., Tao, T., Guo, J., Wang, L., Lu, A.Y. and Chen, H. (2008) Low-Intensity Voluntary Running Lowers Blood Pressure with Simultaneous Improvement in Endothelium-Dependent Vasodilatation and Insulin Sensitivity in Aged Spontaneously Hypertensive Rats. Hypertension Research, 31, 543-552. http://dx.doi.org/10.1291/hypres.31.543
- Aguilar-Salinas, C.A. and Gomez-Perez, F.J. (2006) The Acapulco Declaration: A Proposal to Reduce Incidence of Diabetes in Mexico. Revista de Investigacion Clinica, 58, 71-77.
- Unnithan, V.B., Katsimanis, G., Evangelinou, C., Kosmas, C., Kandrali, I. and Kellis, E. (2007) Effect of Strength and Aerobic Training in Children with Cerebral Palsy. Medicine and Science in Sports and Exercise, 39, 1902-1909. http://dx.doi.org/10.1249/mss.0b013e3181453694
- Verschuren, O., Ketelaar, M., Gorter, J.W., Helders, P.J., Uiterwaal, C.S. and Takken, T. (2007) Exercise Training Program in Children and Adolescents with Cerebral Palsy: A Randomized Controlled Trial. Archives of Pediatrics & Adolescent Medicine, 161, 1075-1081.
- Verschuren, O., Maltais, D.B., Douma-Van Riet, D., Kruitwagen, C. and Ketelaar, M. (2013) Anaerobic Performance in Children with Cerebral Palsy Compared to Children with Typical Development. Pediatric Physical Therapy, 25, 409-413. http://dx.doi.org/10.1097/PEP.0b013e3182a47022
Abbreviations
AI: atherogenic index
BMI: body mass index
CP: cerebral palsy
GMFCS: classification system for gross motor function
HDL-C: high-density lipoprotein cholesterol
LDL-C: low-density lipoprotein cholesterol
PTC: triceps skinfold
NOTES

*Corresponding author.


