Food and Nutrition Sciences
Vol. 3 No. 2 (2012) , Article ID: 17544 , 7 pages DOI:10.4236/fns.2012.32040
Association between the Adherence to AHA Step 1 Nutrition Criteria and the Cardiometabolic Outcome in the General Population—A Two Year Follow-Up Study
![]()
1Center for the Study of Atherosclerosis, SISA Sez Reg Lomb, Bassini Hospital, Cinisello Balsamo, Italy; 2Department of Pharmacological Sciences, Università degli Studi di Milano, Milan, Italy; 3I.R.C.C.S. Multimedica, Milan, Italy.
Email: Danilo.Norata@unimi.it
Received October 14th, 2011; revised December 19th, 2011; accepted December 27th, 2011
Keywords: AHA Step 1; MUFA; PUFA; Cholesterol
ABSTRACT
Introduction: The National Cholesterol Education Program and the American Heart Association considered a dietary therapy as a primary approach to prevent and treat hyperlipemia and hypertension. Mediterranean diet has been promoted as a model of healthy eating and widely recognized for favorable effects on lipid profile. Objective: We investigated whether the adherence to dietary recommendations have any significant benefit on cardiovascular risk factors. A cohort of 2141 of subjects attending our center was recruited by collaborating General Practitioners who participate in the PLIC Study. Methods: Participants completed a week quantitative food questionnaire, which was analized on a subgroup of 338 subjects at enrolment (V1) and after two years of follow up (V2). Daily energy intake in Kcal, lipid, protein, carbohydrates in percentage of total energy, monounsatured (MUFA), saturated (SFA), polyunsaturated fatty acids (PUFA) in g/die, cholesterol in mg/die was calculated from the food questionnaires. Cardiovascular risk (CVR) was estimated according Framingham algorithm. Results: Subjects which adhered to AHA step 1 diet showed a significantly lower total cholesterol, 213.88 ± 43.00 vs 220.19 ± 39.3 mg/dL, LDL-cholesterol, 139.80 ± 76.36 vs 142.75 ± 35.60 mg/dL (p < 0.01 for both) as compared to subjects with an impaired dietary pattern while no differences were observed for HDL cholesterol. Conclusions: Changes in dietary profiles are associated with an improved lipid profile and therefore remain one of the more favorable nutritional models in the primary prevention of cardiovascular disease.
1. Introduction
Cardiovascular disease (CVD) is the main cause of premature death in Western countries [1,2]. In the past years population-based surveys and large-scale clinical trials have provided scientific evidences that some nutritional patterns are associated with lower incidence of various chronic conditions, including cardiovascular disease and cancer. The effect of a diet on human health has already been underlined in many studies [3-8].
Dietary advice is the first step in reducing cholesterol level. The National Cholesterol Education Program and the American heart Association considered a dietary therapy or medical nutrition the primary approach to prevent and treat hyperlipidemia and hypertension.
According to the original definition of Keys [9], a diet rich in fruits, vegetables, legumes, whole grain products, with olive oil as the principal source of fat, moderate consumption of red wine especially during meals, and low consumption of red meat reduces all cause and cardioscular mortality, lipid levels, blood pressure, and overweight. Based on these observations, health policies have been focused on reducing traditional risk factors through nutritional approaches [2].
Despite this, the adherence of general population to dietary recommendations for preventing CVD and the influence of dietary habits on lipid profile and cardioscular risk factors are far from being complete. In this study we investigated whether the adherence to dietary recommendation results in a significant benefit on cardiovascular risk factors and impacts on intima-media thickness (IMT) of the common carotid artery in a prospective study in a cohort selected from the general population.
2. Materials and Methods
2.1. Study Design
A cohort of 2141 subjects attending the Atherosclerosis Center at Bassini Hospital, was recruited for the PLIC (Progressione Lesione Intimale Carotidea) study. This project is a study designed to verify the presence and progression of atherosclerotic lesions and intima-media thickness (IMT) in the common carotid artery, and how IMT relates to major risk factors for cardiovascular diseases (CVD) such as plasma lipids, lifestyle habits, blood pressure and other markers of atherosclerosis in the general population [10-12]. The recruitment, resulting from the collaboration with general practitioners, who enrolled their ambulatory subjects in the study. The study was approved by the ethical committee of the centre. The participating subjects signed an informed consent to participate in the survey. A complete medical history and physical examination, including evaluation of concomitant medication and diagnoses, was carried out. Blood pressure, body weight and height were measured while body mass index (BMI) was calculated. During the visit, alcohol consumption, smoking habits and physical activity were recorded. Amoung the participants, 338 subjects completed a semi-quantitative food questionnaire in visit 1 and visit 2. In a first meeting with the dietician, subjects were instructed on how to record food intakes and for each specific food on a daily base for a week, a commonly used portion size shown in colour photographs was specified. After a week, the dietitian carefully reviewed with the subjects the dietary questionnaires, methods of preparation of the food, types of fat used and brand names of food items and, if appropriate relevant information was introduced.
In this study we classified our population according to the American Heart Association (AHA) criteria. Subjects were categorized on the basis of the cholesterol intake below or above than 300 mg/day, total fat 30%, protein 15%, carbohydrate 55%, saturated fatty acids (SFA) between 7% - 10%, MUFA 15%, polyunsatureted fatty acids (PUFA) 10%.
2.2. Clinical Outcome Measures
After an overnight fast, blood was collected into tubes containing NaEDTA (0.1 mg mL–1), and plasma was separated by low-speed centrifugation at 4 C. The measurament of plasma lipids was performed by standard enzymatic techniques (ABX for Cobas Mira Plus, Montpellier, France); high-density lipoprotein cholesterol (HDLC) was determined after precipitation of apoB-containing lipoproteins and LDL cholesterol (LDL-C) was calculated by using the Friedewald formula. Ultrasonography of the common carotid artery wall reveals two parallel ecogenic lines separated by an anecoid space: the distance between these two lines constitutes a reliable index of IMT complex.
Ultrasound scanning and reading of carotid arteries were performed by a single expert sonographer, using an 8 MHz transducer (Biosound 2000 II sa, Indianapolis, IN, USA) with an axial and lateral resolution of 0.385 and 0.500 mm, respectively. B-mode evaluations were obtained from echographic images of the far wall in the first centimetre of common carotid arteries, proximal to the bulb dilatation, in lateral projection. Five standardized points 5, 10, 20, 25 and 30 mm from bulb were measured in both arteries and averaged to calculate the mean IMT (IMTm) for each subject. In two scans performed on 75 subjects by the same operator the mean difference in IMTm was 0.005 ± 0.0022 mm and the varation coefficient equal to 1.93%. The correlation between two scan was significant with r = 0.96 (p < 0.0001).
Cardiovascular risk (CVR) was calculated according to the Framingham algorithm. The PLIC population was divided in quartiles according to the CVR.
We calculated daily energy intake (in Kcal), lipid, protein, carbohydrates in % of total energy, monounsatured, saturated, polyunsaturaded fatty acids (in g/die), cholesterol (mg/die) from the dietary questionnaires using a specific softwere derived from the Italian standard food composition tables [13]. Every subject was asked to carefully record the whole daily food intake for 7 consecutive days, expressed in terms of weight units, or other domestic units of measure. The subject was asked also to specify the recipes, listing the ingredients.
2.3. Statistical Analysis
Data were analysed using SPSS 16.0 for windows (Chicago, IL, USA). Results are reported as mean ± SD, if not otherwise stated. Group differences were determined by using ANOVA analysis followed by Bonferroni postHOC analysis. Group differences with p < 0.05 were deemed as statistically significant.
3. Results
The clinical parameters of subjects enrolled in the study are reported in Table 1. In general the subjects are slightly overweight and hypercholesterolemic (Table 1). The dietary pattern for visit 1 and visit 2 are described in Table 2.
Contribution of total fats was above the threshold of 30% of caloric intake in all subjects, and similarly SFA intake in higher and PUFA intake lower compared to the AHA step 1 indications. All subjects were given dietary indication according to the AHA guidelines, (step I) and the dietary pattern was reassessed after 2 years (Table 2, visit 2). Subjects were then classified according to the presence of an improved, unmodified or worsened dietary pattern profile (Table 3). Subjects which moved from a level above to a level below the threshold for a
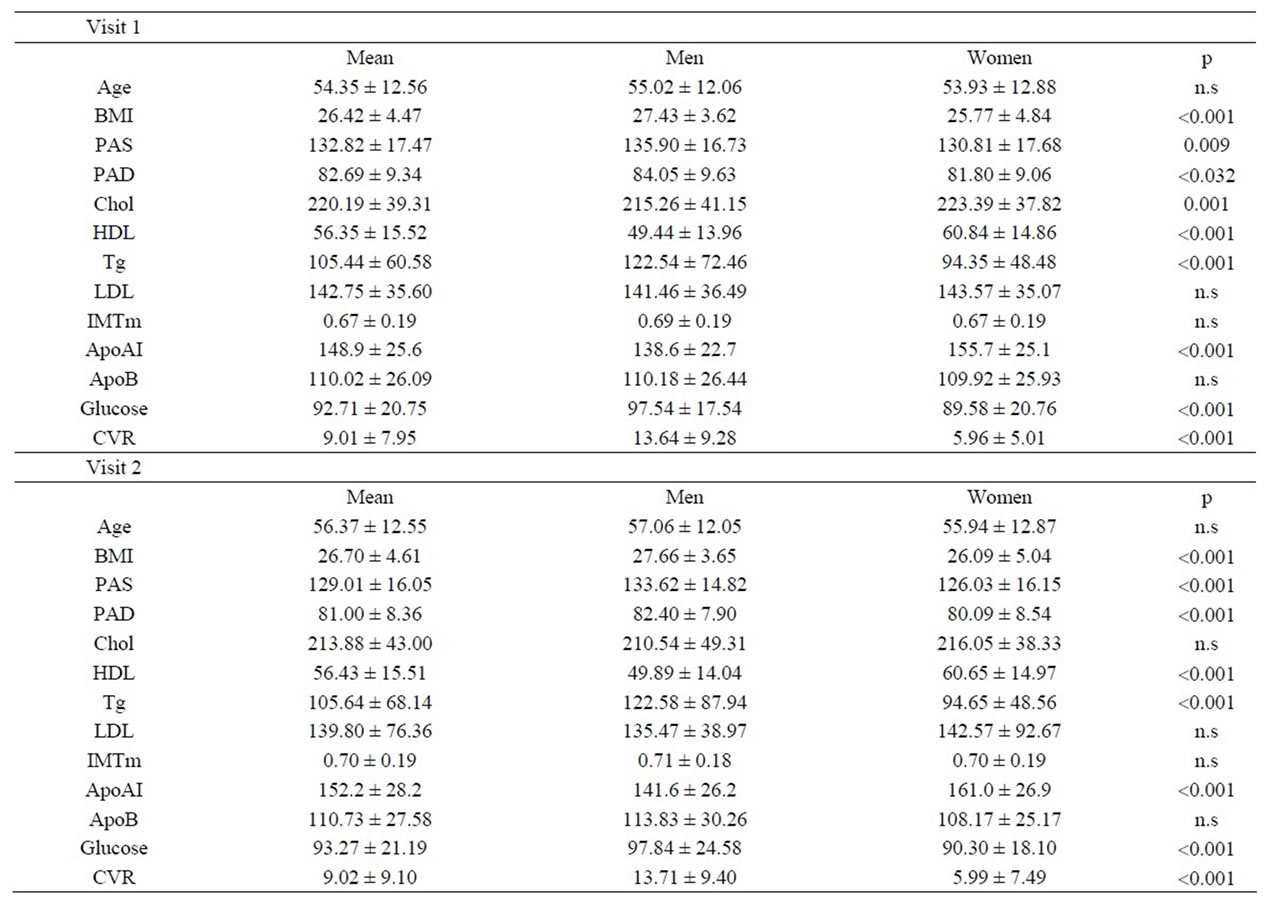
Table 1. Clinical and Anthropometrical parameters, difference between visit 1 and 2 (Mean ± SD).
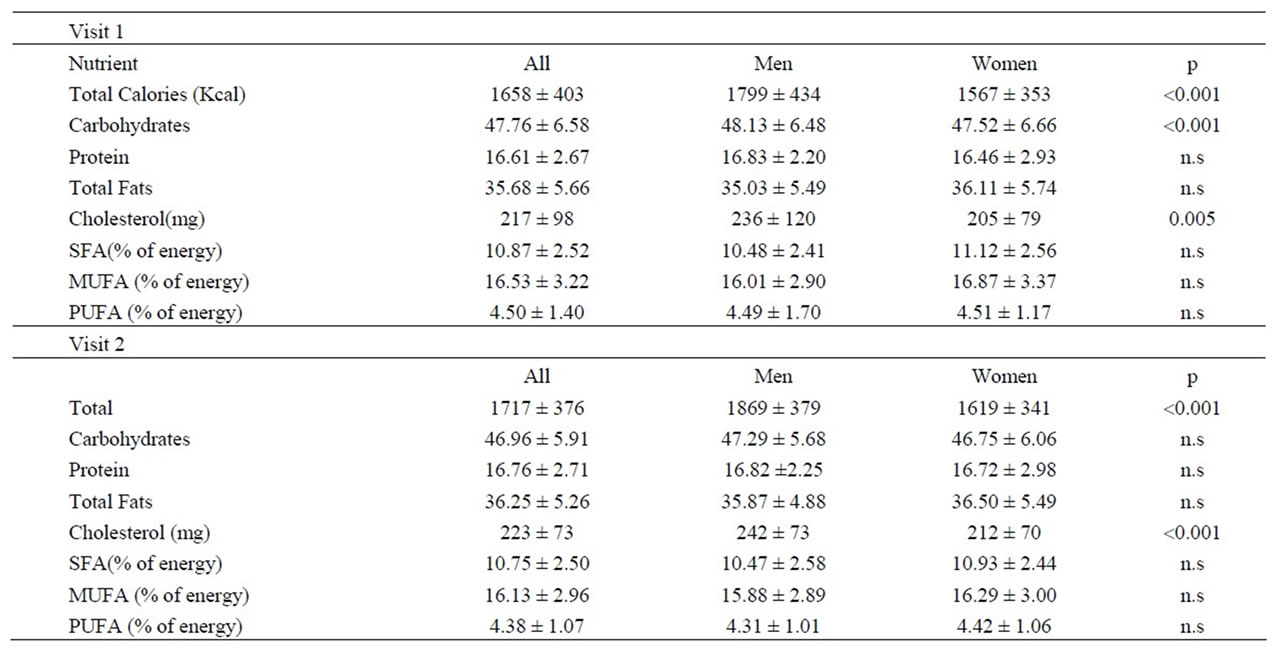
Table 2. Nutrient intake of PLIC population obtained from an analysis of a semi-quantitative food questionnaire (Mean ± SD) (Carbohydrates, Protein, Total Fats are expressed as % of energy).
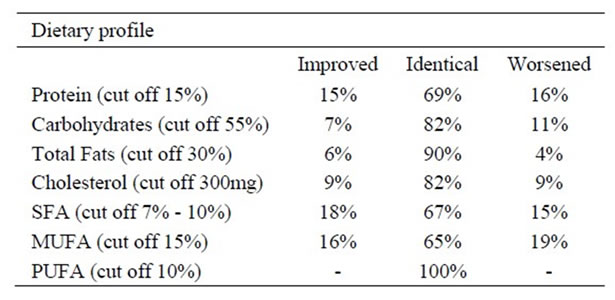
Table 3. Percentage of subjects with different behaviours between visit 1 and visit 2 according to AHA criteria (after hypocholesterolemic dietary prescription).
specific diet component were classified as those with improved dietary profile (group A) (i.e. subjects that at visit 1 had a diet lipid consumption above 30% of total calories intake and at visit 2 had a lipid consumption below 30% of total calories intake).
Similarly, subjects which moved from a level below to a level above the threshold for a specific diet component were classified as those with deteriorated dietary profile (group D) (i.e. subjects that at visit 1 had a diet lipid consumption below 30% of total calories intake and at visit 2 had a lipid consumption above 30% of total calories intake).
Finally the subjects maintaining the same dietary pattern were subclassified in those with desiderable profile (group B) or not (group C) the threshold. Therefore, considering the lipid consumption, of the 338 subjects invited to adhere to AHA step 1 criteria, 256 (76%) did not change their habits while only 25 subjects (7%) had an improved profile and 20 subjects (6%) continued to adhere to the AHA criteria. Of note 37 subjects (11%) moved to a worse dietary profile according to the criteria used. Overall, despite at visit 1 all subjects received information about proper dietary habits, after two years, most of them (87%) failed to adhere to AHA step 1 indi cations. A decrease in lipid consumption that was significantly associated with a decrease in total plasma cholesterol and triglyceride levels was observed (Spearman correlation coefficient = 0.12, p < 0.05 for both). Subjects which continued to adhere to AHA step 1 criteria or moved to AHA step 1 criteria (group A and B) showed a significant reduction from visit 1 to visit 2 in total cholesterol, LDL-cholesterol, triglyceride plasma levels, glycemia and BMI compared to subjects with a worsening of the lipid consumption profile (group D), Figure 1. No differences were observed for HDL this profile was associated also with an improvement in the calculated CVR. Next we investigated the contribution of changes in fatty acids (FA) intake, called saturated FA (SFA), monounsaturated FA (MUFA) and polyunsaturated FA (PUFA) on cardiometabolic parameters (Figure 2).
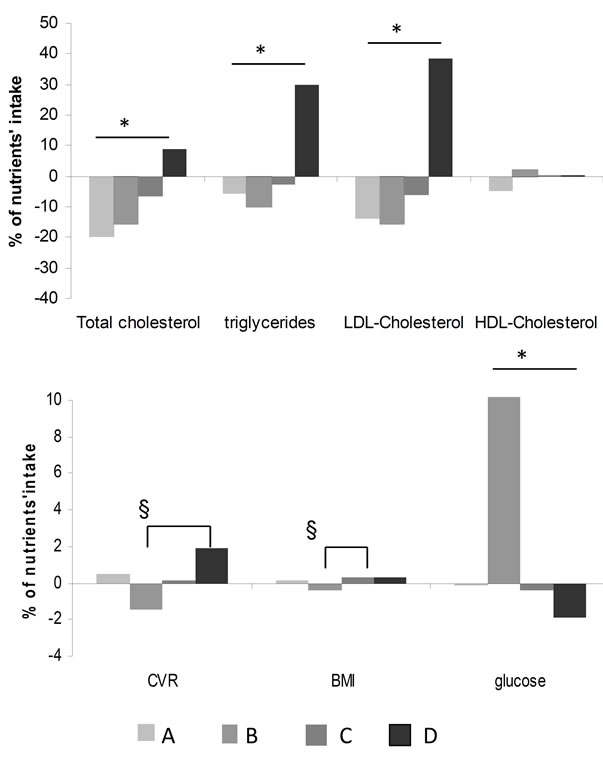
Figure 1. Change in serum lipid levels and cardiometabolic profile according to lipid consumption (*p for trend < 0.05; §p < 0.05, post hoc analysis).
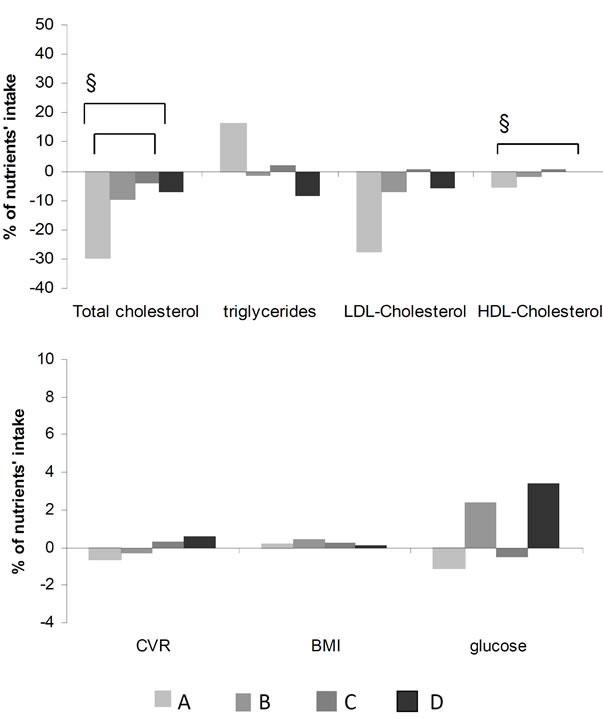
Figure 2. Changes of lipid parameters and cardiometabolic profile according to saturated fatty acids intake (*p for trend < 0.05; §p < 0.05, post hoc analysis).
Of note, the decreased SFA consumption was not directly correlated with a decrease in total cholesterol, LDLcholesterol, triglyceride plasma levels. Subjects with optimal MUFA consumption showed a significant reduction in plasma total cholesterol and triglycerides levels (Figure 3).
PUFA consumption in all subjects was below 10% thus hampering any further analysis. Finally, changes in cholesterol consumption were not correlated with plasma lipids. When protein consumption was analyzed, among 338 subjects invited to adhere to AHA step 1 criteria, 179 (53%) did not change their habits (group C) while only 50 subjects (15%) had an improved profile (group B) and 57 subjects (17%) (group A) continued to adhere to the AHA criteria. 52 (15%) subjects (group D) moved to a poor adherence to the AHA criteria. Overall, despite at visit 1 all subjects received information about proper dietary habits after two years, most of them (68%) failed to adhere to AHA step 1 indications. However a decrease in protein consumption, as determined by the analysis of the dietary questionnaires was associated with a significant decrease in LDL cholesterol levels and CVR (Spearman correlation coefficient = 0.12, p < 0.05 for both) (Figure 4). Finally, when carbohydrate consumption, was investigated of the 338 subjects invited to adhere to AHA step 1 criteria, most of them, 305 subjects (90%) (group A), continued to adhere to the AHA criteria, 19 subjects (6%) had an improved profile (group B)
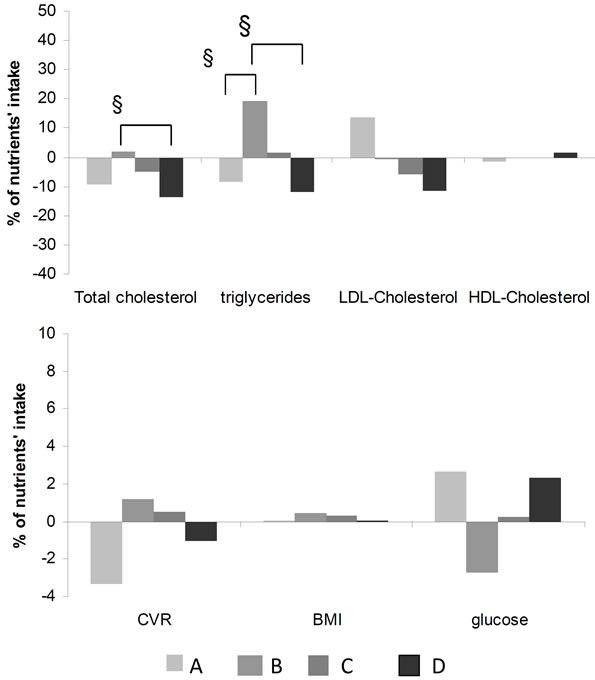
Figure 3. Changes of lipid parameters and cardiometabolic profile according to MUFA intake. (*p for trend < 0.05; §p < 0.05, post hoc analysis).
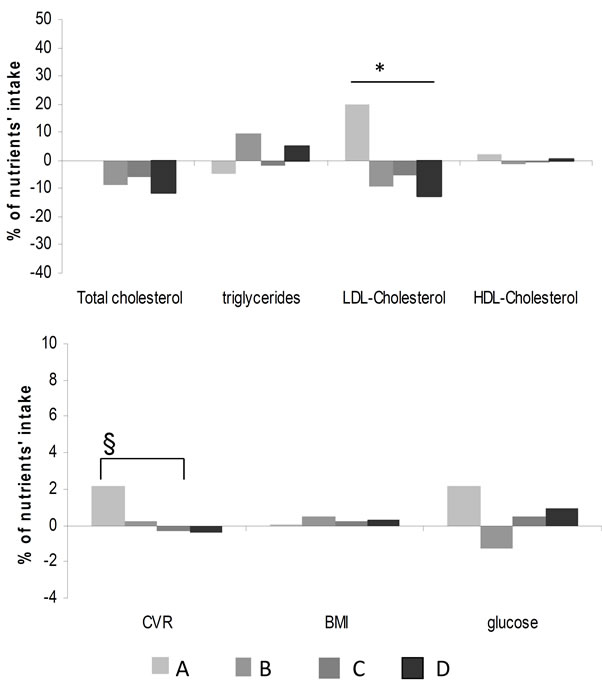
Figure 4. Changes of lipid parameters and cardiometabolic profile according to protein intake. (§p < 0.05, post hoc analysis).
while only 2 subjects (0.5%) did not changed their habits (group C). Finally 12 (3.5%) subjects (group D) moved to a poor adherence to the criteria. Overall after two years only 4% of subjects failed to adhere to AHA step 1 indications on carbohydrate consumption thus resulting in low statistical power to detect significant differences in cardiometabolic variables. Finally, despite the lack of adherence to AHA step 1 criteria for lipid or protein consumption resulted in the worsening of plasma lipid profile, no differences were observed for IMT progresssion in the two years follow up period.
4. Discussion
In this paper we report the effects of the adherence to AHA Step1 nutrition criteria in relation to the cardiometabolic profile in the general population following a two year period. Previous studies reviewed by Caggiula et al. [14] showed that total and saturated fat intake are positively correlated with coronary artery disease and serum total cholesterol while data on correlation with tryglicerides or HDL are less consistent.
Available evidence from cross-population studies showed a large difference among dietary habits and cardiovascular risk thus hampering the likelihood of finding significant associations [8]. These groups may differ in a number of aspects which could in turn affect cardiovascular risk (genetic factors, lifestyle, environment) and although several attempts to control statistically for these differences were performed, it is still difficult to equalize for all these factors in the analysis. This represents the main limitation in the interpretation of the associations observed in cross-population studies. Nevertheless current dietary recommendations are based also on these findings and therefore the validation of the nutrition criteria in a prospective population study is of great interest. We therefore collected dietary habits in free living subjects and instructed them to follow the dietary indications proposed in the AHA step 1 diet. After two years subjects were reassessed for dietary habits and physical and biochemical examination were performed.
During the follow-up, despite the suggestions of the dietician, not surprising most of the subjects continued on the same dietary habits; indeed, considering the lipid consumption, most of the subjects did not adhere to AHA step 1 criteria. This resulted in an increased total cholesterol, LDL-cholesterol, triglyceride plasma levels and glycemia profile, thus supporting a worsening of the cardiometabolic profile. However the two years follow up period was not enough to appreciate an increased IMT progression associated with the worsening of the cardiometabolic profile and probably longer prospective analysis are warranted to appreciate whether adherence to dietary habits would be reflected in changes in pre-clinical atherosclerosis.
Among different fatty acids, only changes in MUFA consumption resulted in a significant effect on plasma total cholesterol and triglycerides, while no major effects in the two years follow-up were observed with increased SFA consumption. Similarly, in those subjects which adhered to AHA step 1 guidelines, reduced protein consumption was associated with an improved profile.
Our data demonstrate that in an Italian population the general outlines of prudent diet are not properly followed, in particular concerning total fat, SFA and PUFA consumption. In both sexes, the contribution of total fat is over 30%, the recommended cut-off for the healthy diet, especially the contribution of PUFA is extremely low compared to recommended values (10% of energy).
We have to acknowledge some limitations of our study; first, as for all the studies available, we can not exclude a bias in the filling of the food questionaries. Second, energy intake of our population is lower than the average values of the other studies, even though it fits with the wide daily energy intake ranges obtained from the other dietary surveys carried out in European countries. Indeed, Karamanos et al. [15] showed a very wide range of energy intake among countries of the Mediterranean area, with an average value for Italy similar to ours. In conclusion our data demonstrate that dietary habits of the general population, despite dietician suggestions, remain associated with a high contribution from total fat with a prevalence of SFA and a limited contribution of polyunsaturated fats. Of note, changes in dietary profile, continue to be associated with an improved cardiometabolic profile and therefore remain one of the nutritional models more favorable for cardiovascular disease primary prevention.
5. Acknowledgements
This work was supported by a grant from SISA (Italian Society for the Study of Atherosclerosis) Lombardia Chapter.
REFERENCES
- A. Keys, “Coronary Heart Disease in Seven Countries,” Circulation, Vol. 41, 1974, pp. 1-211.
- F. Sofi, S. Vecchio, G. Giuliani, F. Martinelli, R. Marcucci, A. M. Gori, S. Fedi, A. Casini, C. Surrenti, R. Abbate and G. F. Gensini, “Dietary Habits, Lifestyle and Cardiovascular Risk Factors in a Clinically Healthy Italian Population: The ‘Florence’ Diet Is Not Mediterranean,” European Journal of Clinical Nutrition, Vol. 4, No. 59, 2005, pp. 584-591. doi:10.1038/sj.ejcn.1602112
- Expert Panel on Detection, Evaluation and Treatment of high blood cholesterol in adults, et al., “Executive Summery of the Third Report of the National Cholesterol Educational Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III),” Journal American Medical Association, Vol. 285, No. 19, 2001, pp. 2486- 2497.
- V. Ganji, M. R. Kafai, Third National Health and Nutrition Examination Survey, “Demographic, Health, Lifestyle, and Blood Vitamin Determinants of Serum Total Homocysteine Concentrations in the Third National Health and Nutrition Examination Survey, 1988-1994,” American Journal Clinical Nutrition, Vol. 4, No. 77, 2003, pp. 826-833.
- A. Ascherio, E. B. Rimm and E. L. Giovannucci, “A Prospective Study of Nutritional Factors and Hypertension among US Men,” Circulation, Vol. 5, No. 86, 1992, pp. 1475-1484.
- L. Appel, T. Moore, E. Obarzanek, W. Vollmer, L. Svetkey and F. Sacks, “A Clinical Trial of the Effect of Dietary Patterns on Blood Pressure,” New England Journal Medicine, Vol. 336, No. 16, 1997, pp. 1117-1124. doi:10.1056/NEJM199704173361601
- J. F. Price and F. G. R. Fowkes, “Antioxidant Vitamins in the Prevention of Cardiovascular Disease,” European Heart Journal, Vol. 18, No. 5, 1997, pp. 719-727.
- L. B. Bunyard, K. E. Dennis and B. J. Nicklas, “Dietary Intake and Changes in Lipoprotein Lipids in Obese, Postmenopausal Women Placed on an American Heart Association Step 1 Diet,” Journal American Diet Association, Vol. 1, 2002, pp. 2-7.
- A. Keys, A. Menotti, M. J. Karvonen, C. Aravanis, H. Blackburn, R. Buzina, B. S. Djordevic, A. S. Dontas, F. Fidanza, M. H. Keys, D. Kromhout, S. Nedeljkovic, S. Punsar, F. Seccareccia and H. Toshima, “The Diet and 15-Year Death Rate in the Seven Countries Study,” American Journal of Epidemiology, Vol. 124, No. 6, 1986, pp. 903-915.
- G. D. Norata, I. Baragetti, S. Raselli, A. Stuc chi, K. Garlaschelli, S. Vettoretti, G. Piloni, G. Buccianti and A. L. Catapano, “Plasma Adiponectin Levels in Chronic Kidney Disease Patients: Relation with Molecular Inflammatory Profile and Metabolic Status,” Nutrition Metabolism Cardiovascular Disease, Vol. 20, No. 1, 2010, pp. 56-63.
- G. D. Norata, S. Raselli, L. Grigore, K. Garlaschelli, E. Dozio, P. Magni and A. L. Catapano, “Leptin: Adiponectin Ratio Is an Independent Predictor of Intima Media Thickness of the Common Carotid Artery,” Stroke, Vol. 38, No. 10, 2007, pp. 2844-2846. doi:10.1161/STROKEAHA.107.485540
- G. D. Norata, M. Ongari, K. Garlaschelli, S. Raselli, L. Grigore and A. L. Catapano, “Plasma Resistin Levels Correlate with Determinants of the Metabolic Syndrome,” European Journal Endocrinology, Vol. 156, No. 2, 2007, pp. 279-284. doi:10.1530/eje.1.02338
- E. Carnevale and F. Miuccio, “Tabelle di Composizione Degli Alimenti,” Istituto Nazionale della Nutrizione, Via Ardeatina, 1989.
- A. W. Caggiula and V. A. Mustad, “Effects of Dietary Fats and Fatty Acids on Coronary Artery Disease Risk and Total and Lipoprotein Cholesterol Concentration: Epidemiological Studies,” American Journal Clinical Nutrition, Vol. 65, No. 5, 1997, pp. 1597S-1610S.
- B. Karamanos, A. Thanopoulou, F. Angelico, S. AssaadKhalil, A. Barbato, M. Del Ben, V. Dimitrijevic-Sreckovic, P. Djordjevic, C. Gallotti, N. Katsilsambros, I. Migdalis, M. Mrabet, M. Petkova, D. Roussi and M. T. Tenconi, “Nutritional Habits in the Mediterranean Basin. The Macronutrient Composition of Diet and Its Relation with the Traditional Mediterranean Diet. Multi-Centre Study of the Mediterranean Group for the Study of Diabetes (MGSD),” European Journal Clinical Nutrition, Vol. 56, No. 10, 2002, pp. 983-991. doi:10.1038/sj.ejcn.1601413

