Journal of Cancer Therapy
Vol.06 No.12(2015), Article ID:60949,9 pages
10.4236/jct.2015.612114
Treatment of Non Melanoma Skin Cancers: An Intra-Comparison Study of CuradermBEC5 and Various Established Modalities
K. Cham, A. Cham, T. Chase, V. Zhou, B. Cham*
Australasian Medical Research, Port Vila, Republic of Vanuatu

Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).


Received 8 October 2015; accepted 6 November 2015; published 9 November 2015

ABSTRACT
Dermatologists, surgeons, oncologists and radiotherapists usually jointly manage skin cancers. The strengths and limitations of the established procedures are known. A new naturally derived topical cream, CuradermBEC5, for the treatment of non melanoma skin cancers has previously been described. In this communication, intra-comparison treatments of skin cancer between Cura- dermBEC5 therapy and the established treatments, surgery, radiation therapy, laser therapy, photo- dynamic therapy, imiquimod cream and cryosurgery are presented. Non melanoma skin cancer cases that had previously been treated unsuccessfully with the established procedures were sub- sequently treated successfully with CuradermBEC5. These observations are interesting because the identical lesions were treated by various modalities. In addition to the superior efficacious out- come of CuradermBEC5 therapy versus the established treatments, the cosmetic end results with CuradermBEC5 treatment are remarkable.
Keywords:
Skin Cancer, Curaderm, Surgery, Radiation, Laser, Cryosurgery, PDT, Imiquimod

1. Introduction
Most sick people go to any lengths to get better. To date, this translates to the sick person engaging a healthcare professional resulting in dependency of the patient on the healthcare professional. In turn, the healthcare professional relies and depends on medical information for the particular disease, which is obtained from pharmaceutical companies.
Herewith lies the dilemma. The healthcare professional has the wellbeing of the patient at heart, but due to his/her medical training with pharmaceuticals, the healthcare professional is largely dependent on information from the pharmaceutical industry.
Other than questionable efficacy of some medications, the fact remains that the cost of innovative, patent protected drugs from pharmaceutical companies is becoming increasingly difficult for patients and cash-strapped healthcare systems [1] . This phenomenon has recently been highlighted [2] [3] .
Regarding the disease cancer, the pharmaceutical industry has little to offer, as proven by the overall very limited successes, achieved by “established” procedures.
It is only after the established drugs and/or other established treatment regimes fail, which in the case of cancer, is often inevitable, the patient is faced with seeking other possible treatments. At this stage the disease would have progressed to a possible life threatening path and the valuable time for recovery is lost. Furthermore, the current established treatments for cancer are expensive, very toxic to the body and complicate any further alternative therapy.
It can be argued that the established therapies for cancer have had a fair go, and unfortunately, are suboptimal and are reaching a dead end despite of the further research and development.
It is also interesting to note that when the pharmaceutical industry develops a drug, either synthetic or natural, it is branded as an “established conventional” drug. If that same drug is developed by a small institution, using the same development procedures as the large pharmaceutical companies, the drug is branded as an “alternative” drug that exists outside the established society.
The time is now overdue to try “proven” safe alternatives for the treatment of cancer. The natural approach to treat cancer should be given an opportunity to be the first, not the last method of treatment in order for the patient to have a reasonable chance to overcome the medical condition without prior induced toxicity. Critical evaluation of the alternative treatments will determine whether this approach will produce an acceptable therapy or not.
To show the potential of this concept, clinical cases of skin cancers comparing accepted “established” treatment procedures as opposed to a novel naturally derived topical “alternative” treatment are presented.
CuradermBEC5 cream for topical application contains the established antineoplastic agents solasodine rhamnosides which are composed of solamargine and solasonine. Specific endogenous endocytic lectins (EELs) have been identified on cancer cells [4] . These EELs have been further characterized as rhamnose binding protein (RBP) receptors [5] . RBP receptors are present on cancer cells but not normal cells [6] . RBP receptors bind the solasodine rhamnosides (BEC) which are then internalized into the cancer cells by receptor-mediated endocytosis. BEC interacts with the lysosomes and mitochondria resulting in the triggering of intrinsic and extrinsic apoptotic pathways in the cancer cells by up-regulating the expression of external death receptors, such as tumor necrosis factor receptor 1 (TNF-1), Fas receptor, TNF-1 associated death domain and Fas-associated death domain [6] . BEC enhances the intrinsic ratio of Bax to Bcl-2 by up-regulating Bax and down-regulating Bcl-2 and Bcl-x expressions. These effects result in activation of Caspase-8, -9 and -3 leading to apoptosis in cancer cells [6] [7] .
This communication describes the results of intra-comparison treatments, of the same non melanoma skin cancers, by established procedures compared with a treatment using CuradermBEC5, a topical cream formulation containing naturally derived solasodine rhamnosides.
The non melanoma skin cancer cases presented in this communication are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
BCC is a nonmelanocytic skin cancer that arises from basal cells which are small round cells found in the lower layer of the epidermis. BCC is the most common skin cancer in humans. BCC typically appears on sun- exposed skin, and is slow growing and rarely metastasize. BCC usually appears as a flat, firm, pale area that is small, raised, pink or red, translucent, shiny, waxy and the area may bleed following minor injury. Tumor size can vary from a few millimeters to several centimeters in diameter. BCC is diagnosed with a skin biopsy.
Cutaneous squamous cell carcinoma (c SCC) is the second most common human cancer. c SCC typically manifests as a spectrum of progressively advanced malignancies, ranging from a precursor actinic keratosis (AK) to SCC in situ (SCC is), invasive c SCC, and finally metastatic SCC.
Like BCC, SCC is associated with sun damage. Unlike BCC, SCC can metastasize and is potentially deadly. The classic presentation of a c SCC is that of a shallow ulcer with heaped-up edges, often covered by a plaque. Typical surface changes may include, scaling, ulceration, crusting or a cutaneous horn. Like BCC, c SCC can vary in size from a few millimeters to several centimeters in diameter. SCC is also diagnosed with a skin biopsy.
2. Treatments Administered
Unbiased selection of study population: only patients with confirmed histological diagnoses were selected. Two patients with c SCC and 4 patients with BCC were treated by the various procedures.
Procedures used to treat the patients:
Surgical Excision
The skin cancer was surgically excised by a surgeon followed by skin grafting [8] .
Radiation Therapy
Radiation therapy uses high-energy rays (X-rays) or particles (photons, electrons or protons) to kill cancer cells [9] .
Laser Therapy
Laser therapy uses an intense, focused beam of light to destroy skin cancer tissue [10] .
Photodynamic Therapy (PDT)
PDT uses special drugs, called photosensitizing agents, along with light to kill cancer cells [11] .
Imiquimod Cream
Imiquimod cream works by modifying the immune response to treat superficial skin cancers [12] .
Cryosurgery
Cryosurgery (also called cryotherapy) is the use of extreme cold produced by liquid nitrogen (or argon gas) to destroy abnormal tissue. Cryosurgery is used to treat external tumours, such as those on the skin [13] .
CuradermBEC5 Cream
This cream is available to patients in several countries. CuradermBEC5 cream contains antineoplastic solasodine rhamnosides (BEC), which are extracted from the fruit of Solanum linnaeanum [14] .
All procedures were performed by specialists (dermatologists, surgeons and oncologists). The topical applications with the cream formulations were adhered to according to their treatment instructions [15] .
None of the photographs were adulterated.
All treatment procedures applied to the patients are clinically available and no Approval by the Ethics Committee was necessary.
3. Results
CuradermBEC5 versus surgical excision (Patient 1)
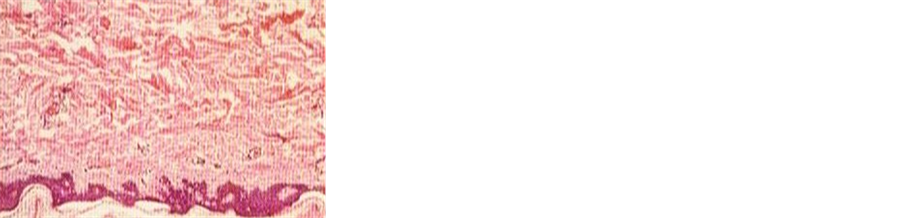
A 55-year-old male had an SCC, for over a year, on his head. Figure 1 shows a clinical diagnosed SCC of approximately 2.5 cm in diameter (a), two weeks during CuradermBEC5 therapy there was erosion of the tumour (b), and after 8 weeks of treatment the lesion was clinically ablated (c). Histological analysis confirmed the clinical diagnosis that the lesion was an SCC before treatment (d) and that after treatment there was no evidence of residual tumour cells (e). An independent dermatologist of this patient did not accept CuradermBEC5 therapy and insisted to surgically remove the same area where the original lesion was, but had previously been treated with CuradermBEC5. Figure 1(f) illustrates the end result after surgery and skin grafting. Importantly, histological analyses of the entire area of the surgically removed tissue revealed that there were no traces of cancer cells. So, CuradermBEC5 therapy had already successfully removed all the cancer cells confirming Figure 1(e) and the surgery was not necessary. Nevertheless, in this case, the difference between surgical excision and CuradermBEC5 therapy is clearly shown. The difference in cosmetic outcome is immense.
CuradermBEC5 versus radiation therapy (Patient 2)
Figure 2(a) illustrates a BCC after radiation therapy, it is clear that there was a recurrence. Several months after the recurrence, the lesion was treated with CuradermBEC5. Figures 2(b)-(d) show the appearances of the lesion during CuradermBEC5 therapy. Some inflammation is observed surrounding the lesion. The lesion progressively reduced in size. After 8 weeks treatment with CuradermBEC5, the lesion was completely ablated (Figure 2(d)). The cosmetic result after CuradermBEC5 therapy was remarkable, despite the previous relapsed radiotherapy treatment.
CuradermBEC5 versus laser therapy (Patient 3)
A 24-year-old female patient was treated with laser therapy for a BCC close to the right eye. The BCC recurred after laser therapy (Figure 3(a)). The patient then had CuradermBEC5 therapy for 8 weeks. The BCC re-
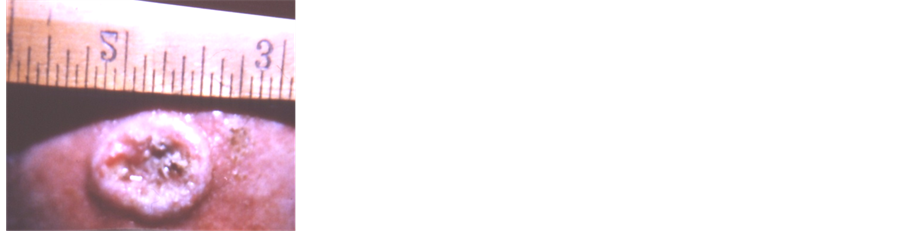
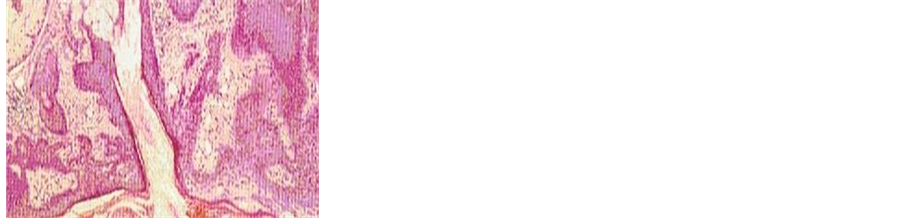
Figure 1. Clinical diagnosed SCC before CuradermBEC5 therapy (a), two weeks during CuradermBEC5 therapy (b), and after 8 weeks treatment (c). Histological analysis of lesion before (d) and after (e) treatment. Unnecessary surgery of the already ablated lesion resulted in skin grafting (f).
Figure 2. Recurrent BCC after radiation therapy but before CuradermBEC5 therapy (a), during treatment with CuradermBEC5 (b, c) and after 8 weeks treatment (d).
Figure 3. Recurrent BCC close to the eye after laser therapy but before CuradermBEC5 therapy (a) during treatment with CuradermBEC5 (b, c) and after 8 weeks treatment (d).
sponded rapidly toward CuradermBEC5 treatment. Figure 3(b), Figure 3(c) show the appearances during treatment and Figure 3(d) shows the end result after 8 weeks of CuradermBEC5 therapy. There was some scarring at the end of the treatment that may have been caused by the unsuccessful laser treatment.
CuradermBEC5 versus photodynamic therapy (Patient 4)
Figure 4(a) illustrates a relapsed BCC on the cheek of a female patient after PDT treatment. Figure 4(b) shows that CuradermBEC5 therapy caused massive erosion of the treated lesion. Continual CuradermBEC5 therapy resulted in diminishing sizes of the tumor (Figure 4(c), Figure 4(d)), ultimately resulting in complete removal of the tumor after 10 weeks of treatment (Figure 4(e)). There was moderate scarring at the completion of the CuradermBEC5 therapy.
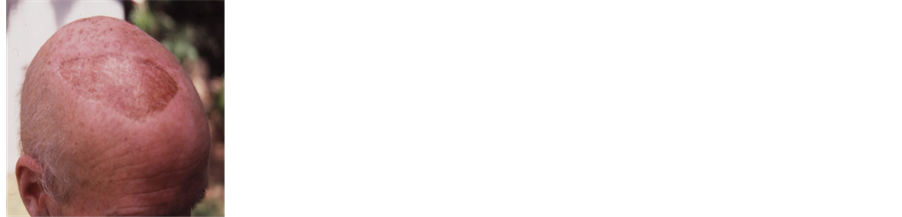
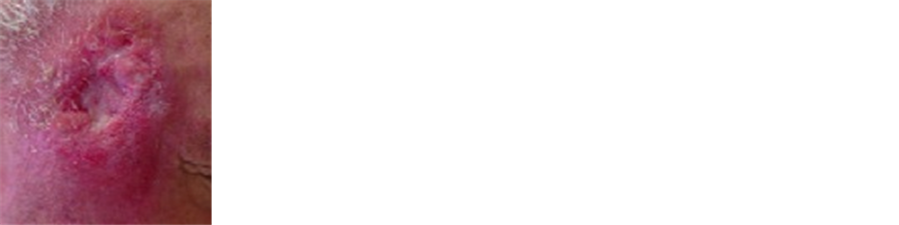
CuradermBEC5 versus cryosurgery (Patient 5)
This male patient had previously undergone cryosurgery for a BCC on the right temporal region. Figure 5(a) shows that there was a recurrence of the BCC after cryosurgery. Several months after the recurrence of the BCC, the patient was treated with CuradermBEC5. Figure 5(b) shows that the CuradermBEC5 therapy exposed deep seated tumor cells. Total required treatment period for the complete removal of the entire lesion was 9 weeks (Figure 5(c)). This patient had dyed his hair after completion of CuradermBEC5 therapy.
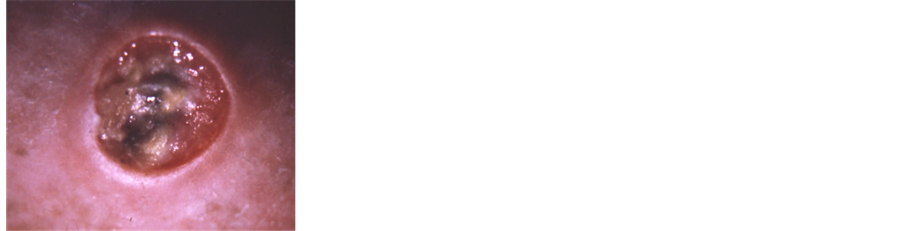
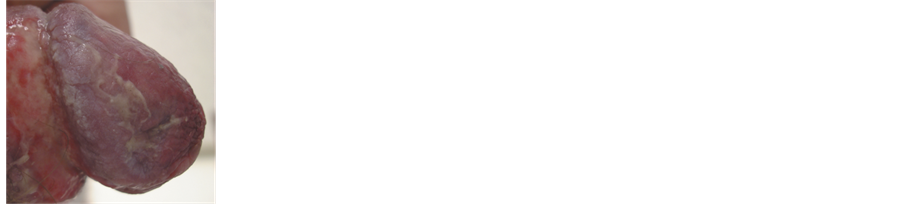
CuradermBEC5 versus imiquimod cream (Patient 6)
This patient had treated Bowen’s Disease (SCC in situ) on the penis for over 2 years with 5% Imiquimod cream; response appeared initially satisfactory, but the lesion was still present after 2 courses of Imiquimod treatments. Subsequently, the patient elected to treat his Bowen’s Disease with CuradermBEC5. Figure 6(a) shows an in situ SCC (Bowen’s Disease) on the penis that had not been successfully treated with imiquimod cream. Two months after starting CuradermBEC5 therapy the lesion showed minimal response (Figure 6(b)). Marked
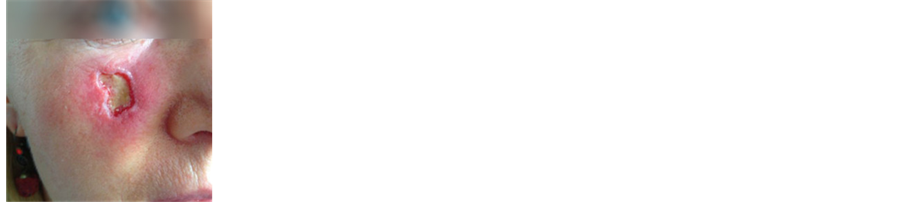
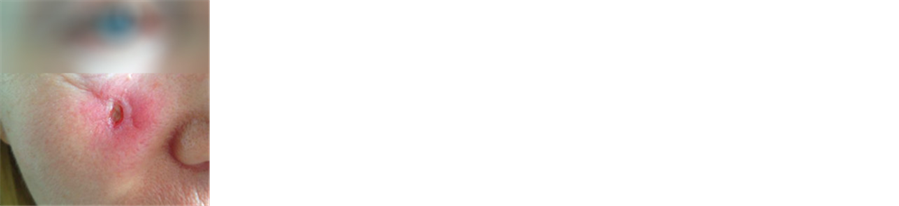
Figure 4. Relapsed BCC on cheek after PDT but before CuradermBEC5 therapy (a), during CuradermBEC5 treatment (b, c, d) and after 10 weeks of treatment (e).
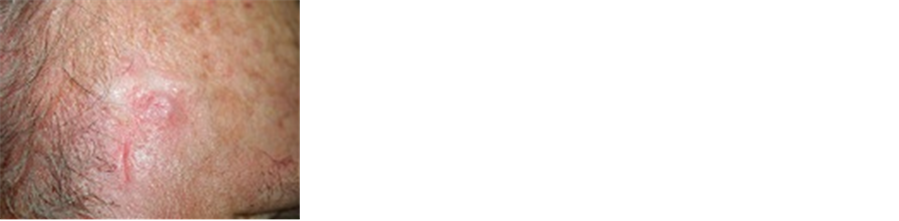
Figure 5. Recurrent BCC after cryosurgery but before CuradermBEC5 therapy (a), during CuradermBEC5 treatment (b) and 9 weeks of treatment (c).
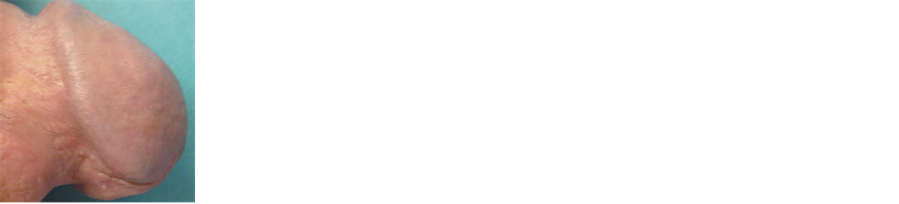
Figure 6. Recurrent in situ SCC on the penis after treatment with imiquimod cream but before CuradermBEC5 therapy (a), during CuradermBEC5 treatment for two months (b), four months (c) and 10 months (d)
clinical improvement was observed after 4 months (Figure 6(c)), and by his 9th month follow-up visit, even greater regression of the lesion was noted. At 10 months, the lesion was no longer clinically apparent, and the CuradermBEC5 treatment was stopped. The endpoint of therapy coincided with regrowth of skin at the treatment site (Figure 6(d)). The tissue-sparing technique of CuradermBEC5 preserved functionality of the patient’s penis. The cosmetic end result was incredible.
Overall observations with CuradermBEC5 therapy
During CuradermBEC5 therapy, initially, the lesions appear to become larger, but this is only transient. Continuous treatments result in diminishing of the size of the tumor until the tumor is completely ablated and is replaced with normal tissue. During treatment with CuradermBEC5 the cancer cells are killed and replaced with normal cells, CuradermBEC5 does not kill normal cells. In the initial stages of CuradermBEC5 therapy some patients experience local irritation, even a burning sensation, for several minutes after application of the cream to the lesion, but again, this is transient. Depending on the size of the tumor, some ulceration does occur. Follow- up with all of the patients for at least one year after CuradermBEC5 treatment showed no recurrences of the treated lesions.
4. Discussion
To compare different modality treatments of a disease, large numbers of patients are required to establish possible statistical significant differences. Even so, the inter variability of the disease makes it more scientifically acceptable to conduct cross-over clinical trials which are only applicable with certain diseases. In the case of treating skin cancer this approach is not possible.
One way to compare the efficacy of treatment procedures is by performing an intra patient disease approach. This approach has been applied with the current studies and can be considered as preliminary only. Nevertheless, it is quite clear that CuradermBEC5 therapy is at least equally effective or more effective than other well ‘established’ treatment modalities.
The reported skin cancer patients in this communication were not cherry-picked. All patients, except the patient represented in Figure 1 presented themselves to clinics to seek further treatments for their failed previous therapies. Subsequently, these patients were treated with CuradermBEC5.
These patients presented an opportunity to compare and contrast the various treatment procedures on identical lesions in terms of safety, efficacy, ease of treatment, cosmetic outcomes and costs of treatment.
This report identifies that, due to specificity, the efficacy of CuradermBEC5 is superior compared to the other procedures. To the best of our knowledge, at this stage, we are unaware of cases where CuradermBEC5 therapy has failed and other treatments have been successful for treating the same lesions.
Most of the other described procedures are much more complicated and costly compared with CuradermBEC5 therapy. It is also beneficial that CuradermBEC5 therapy does not require continuous physician or hospital attendance.
The cosmetic outcomes with CuradermBEC5 therapy are far superior and confirm previous studies [16] - [29] . In addition, the functionality of the skin cancer affected tissue is completely restored after successful removal of the cancer with CuradermBEC5 therapy [21] , an observation not obtained by any established therapy.
The need for a new treatment of skin cancer is warranted. Skin cancer is the most common form of human cancer. Over the past three decades, more people have had skin cancer than all other cancers combined. BCC is the most common form of skin cancer, an estimated 2.8 million BCCs are diagnosed annually in the USA. BCCs are rarely fatal, but can be highly disfiguring if allowed to grow. Over three thousand deaths from advanced BCCs occur annually in the USA [29] . SCC is the second most common form of skin cancer. An estimated 700,000 cases of SCCs are diagnosed each year in the USA. Between 3900 and 8800 died from this disease in the USA in 2012. Organ transplant patients are up to 250 times more likely than the general public to develop SCC [29] .
This article describes the superiority of CuradermBEC5 therapy compared with other widely used modalities, both in efficacy and cosmesis, on the most prevalent skin cancers, BCCs and SCCs.
CuradermBEC5 offers an exceptional safe treatment that selectively eliminates skin cancer without disturbing the healing process.
Finally, this communication exemplifies that ‘alternative’ natural treatments should be seriously considered for a wide range of diseases with appropriate stringent evaluation. It is interesting to note that currently, approximately 50% of patients who had previously used laser, surgery or cryotherapy for their skin cancers now prefer CuradermBEC5 (personal communication, Institute of Clinical Oncology, Russian Cancer Research Centre).
5. Conclusions
Patients included in this study presented exceptional circumstances whereby direct treatment comparisons of identical BCCs and SCCs could be assessed by various widely used skin cancer therapies and CuradermBEC5 topical therapy.
The relative merits of CuradermBEC5 therapy over the described other established modalities are specificity, superior efficacy, superior cosmesis, low toxicity, non continuous physician or hospital attendance and low cost.
Skin cancer is by far the most common form of human cancer and the incidence of skin cancer is increasing. It is fortunate that a simple but very effective and safe therapy for skin cancer is now available. For the benefit of the patient, CuradermBEC5 is the therapy that should be considered as the method of choice for treating non melanoma skin cancers. Finally, here it is shown that not all-outstanding therapeutics comes from multi-billion pharmaceutical companies.
Acknowledgements
The following Dermatologists and Oncologists supervised the treatments of the patients: Dr. R. Theile―Patient 1, Figure 1(f), Dr. A. Batsev―Patients 2 - 5, Dr. L.H. Goldberg―Patient 6.
Cite this paper
K.Cham,A.Cham,T.Chase,V.Zhou,B.Cham, (2015) Treatment of Non Melanoma Skin Cancers: An Intra-Comparison Study of CuradermBEC5 and Various Established Modalities. Journal of Cancer Therapy,06,1045-1053. doi: 10.4236/jct.2015.612114
References
- 1. Cham, A., Cham, K., Chase T. and Cham, B.E. (2015) A Standardized Plant Extract Containing a Target Compound Is Acceptable as a Potent Therapeutic Entity: Relevance to BEC and Solamargine, a Topical Clinical Formulation CuradermBEC5. Journal of Cancer Treatment and Research, 3, 22-27.
http://dx.doi.org/10.11648/j.jctr.20150302.12 - 2. Fighting the High Cost of RX Drugs.
http://www.uspirg.org/issues/usp/fighting-high-cost-rx-drugs - 3. Inside Daraprim’s Price Hike.
http://www.businessinsider.com.au/turning-increases-price-of-daraprim-2015-9 - 4. Daunter, B. and Cham, B.E. (1990) Solasodine Glycosides. In Vitro Preferential Cytotoxicity for Human Cancer Cells. Cancer Letters, 55, 209-220.
http://dx.doi.org/10.1016/0304-3835(90)90121-D - 5. Lipscombe, R.J., Carter, S.J. and Ruane, M. (2005) Rhamnose Binding Protein. US Patent No. 6930171.
- 6. Cham, B.E. (2007) Solasodine Rhamnosyl Glycosides Specifically Bind Cancer Cell Receptors and Induce Apoptosis and Necrosis. Treatment for Skin Cancer and Hope for Internal Cancers. Res. J. Biol. Sci., 2, 503-514.
- 7. Sun, L., Zhao, Y., Li, X., Yuan, H., Cheng, A. and Lou, H. (2010) A Lysosomal-Mitochondrial Death Pathway Is Induced by Solamargine in Human K562 Leukemia Cells. Toxicology in Vitro, 24, 1504-1511.
http://dx.doi.org/10.1016/j.tiv.2010.07.013 - 8. Surgery for Basal Cell and Squamous Cell Skin Cancers. American Cancer Society.
http://www.cancer.org/acs/groups/cid/documents/webcontent/003075-pdf.pdf - 9. Radiation therapy for Non melanoma Skin Cancer—WebMD.
http://www.cancerresearchuk.org/about-cancer/type/skin-cancer/treatment/radiotherapy-for-skin-cancer - 10. Lasers in Cancer Treatment—National Cancer Institute.
http://www.cancer.gov/about-cancer/treatment/types/surgery/lasers-fact-sheet - 11. Photodynamic Therapy for Skin Cancer. Accessed July 2015.
http://www.cancerresearchuk.org/about-cancer/cancers-in-general/treatment/other/photodynamic-therapy-pdt - 12. Imiquimod Topical: Medline plus Drug Information. Accessed September 2015.
http://www.nlm.nih.gov/medlineplus/druginfo/meds/a698010.html - 13. Cryosurgery. Accessed September 2015.
http://www.cancer.gov/about-cancer/treatment/types/surgery/cryosurgery-fact-sheet - 14. Cham, B.E. (2013) Inspired by Nature, Proven by Science. The New Generation Cancer Treatment That Causes Cancer Cells to Commit Suicide. 1st Edition, Colorite Grahics Printers, Efate.
- 15. Cham, B.E. (1994) Solasodine Glycosides as Anti-Cancer Agents: Pre-Clinical and Clinical Studies. Asia Pacific Journal of Pharmacology, 9, 113-118.
- 16. Cham, B.E., Daunter, B. and Evans, R. (1991) Topical Treatment of Malignant and Premalignant Skin Cancers by Very Low Concentrations of a Standard Mixture (BEC) of Solasodine Glycosides. Cancer Letters, 59, 183-192.
http://dx.doi.org/10.1016/0304-3835(91)90140-D - 17. Cham, B.E. (2011) Topical Solasodine Rhamnosyl Glycosides Derived from the Eggplant Treats Large Skin Cancers: Two Case Reports. International Journal of Clinical Medicine, 2, 473-477.
http://dx.doi.org/10.4236/ijcm.2011.24080 - 18. Cham, B.E. (2008) Cancer Intralesion Chemotherapy with Solasodine Rhamnosyl Glycosides. Research Journal of Biological Sciences, 3, 1008-1017.
- 19. Cham, B.E. and Meares, H.M. (1987) Glycoalkaloids from Solanum sodomaeum L. Are Effective in the Treatment of Skin Cancers in Man. Cancer Letters, 36, 111-118.
http://dx.doi.org/10.1016/0304-3835(87)90081-4 - 20. Punjabi, S., Cook, L.J., Kersey, P., Marks, R. and Cerio, R. (2008) Solasodine Glycoalkaloids: A Novel Topical Therapy for Basal Cell Carcinoma. A Double-Blind, Randomized, Placebo-Controlled, Parallel Group, Multicentre Study. International Journal of Dermatology, 47, 78-82.
http://dx.doi.org/10.1111/j.1365-4632.2007.03363.x - 21. Goldberg, L.H., Landau, J.M., Moody, M.N. and Vergilis-Kalner, I.J. (2011) Treatment of Bowen’s Disease on the Penis with Low Concentration of a Standard Mixture of Solasodine Glycosides and Liquid Nitrogen. Dermatologic Surgery, 37, 858-861.
http://dx.doi.org/10.1111/j.1524-4725.2011.02014.x - 22. Chase, T.R. (2011) CuradermBEC5 for Skin Cancers, Is It? An Overview. Journal of Cancer Therapy, 2, 728-745.
http://dx.doi.org/10.4236/jct.2011.25099 - 23. Cham, B.E. and Chase T.R. (2012) Solasodine Rhamnosyl Glycosides Cause Apoptosis in Cancer Cells, Do They Also Prime the Immune System Resulting in Long Term Protection? Planta Medica, 78, 349-353.
http://dx.doi.org/10.1055/s-0031-1298149 - 24. Cham, B.E. (2012) Intralesion and CuradermBEC5 Topical Combination Therapies of Solasodine Rhamnosyl Glycosides Derived from the Eggplant or Devil’s Apple Result in Rapid Removal of Large Skin Cancers. Methods of Treatment Compared. International Journal of Clinical Medicine, 3, 115-124.
http://dx.doi.org/10.4236/ijcm.2012.32024 - 25. Cham, B.E. (2013) Topical CuradermBEC5 Therapy for Periocular Nonmelanoma Skin Cancer: A Review of Clinical Outcomes. International Journal of Clinical Medicine, 4, 233-238.
http://dx.doi.org/10.4236/ijcm.2013.45041 - 26. Cham, B.E. (2013) Solasodine Glycosides: A Topical Therapy for Actinic Keratosis. A Single-Blind, Randomized, Placebo-Controlled, Parallel Group Study with CuradermBEC5. Journal of Cancer Therapy, 4, 588-596.
http://dx.doi.org/10.4236/jct.2013.42076 - 27. Cham, B.E. (2013) Drug Therapy: Solamargine and Other Solasodine Rhamnosyl Glycosides as Anticancer Agents. Modern Chemotherapy, 2, 33-49.
http://dx.doi.org/10.4236/mc.2013.22005 - 28. Cham, B.E. (2014) A Review of Solasodine Rhamnosides Therapy for in Situ Squamous Cell Carcinoma on the Penis. British Journal of Medicine and Medical Research, 4, 621-631.
- 29. Cham, A. and Cham, B.E. (2015) Treatment of Skin Cancer with a Selective Apoptotic-Inducing CuradermBEC5 Topical Cream Containing Solasodine Rhamnosides. International Journal of Clinical Medicine, 6, 326-333.
http://dx.doi.org/10.4236/ijcm.2015.65042
Abbreviations
AK: actinic keratosis
Bax, Bcl-2, Bcl-x: apoptotic regulatory proteins
BCC: basal cell carcinoma
BEC: a specific mixture of solasodine rhamnosides
Caspase-8, -9, -3: a group of intracellular proteases responsible for the disassembly of the cell into apoptotic bodies
c SCC: cutaneous squamous cell carcinoma
EEL: endogenous endocytic lectin
Fas: a protein member of tumor necrosis factor receptor superfamily
PDT: photodynamic therapy
RBP: rhamnose binding protein
SCC: squamous cell carcinoma
SCC is: squamous cell carcinoma in situ
TNF-1: tumor necrosis factor receptor
NOTES
*Corresponding author.