Natural Science
Vol.4 No.12(2012), Article ID:25369,7 pages DOI:10.4236/ns.2012.412126
Comparison of myocardial perfusion scintigraphy and computed tomography (CT) angiography based on conventional coronary angiography*
![]()
1Department of Nuclear Medicine, Dicle University Medical Faculty, Diyarbakir, Turkey
2Department of Nuclear Medicine, Firat University Medical Faculty, Elazig, Turkey; #Corresponding Author: tansel_balci@yahoo.com
3Department of Nuclear Medicine, Oncology Hospital, Ankara, Turkey
4Department of Cardiology, Firat University Medical Faculty, Elazig, Turkey
5Department of Radiology, Firat University Medical Faculty, Elazig, Turkey
Received 24 August 2012; revised 23 September 2012; accepted 9 October 2012
Keywords: Myocardial Perfusion SPECT; Scintigraphy; CT Coronary Angiography; Conventional Coronary Angiography
ABSTRACT
Coronary artery disease is one of the most common and important health problems in the world. Early diagnosis of this disease is very important to treat before severe myocardial damage occurred. Myocardial perfusion scintigraphy (MPS) and computed tomography coronary angiography (CTCA) which evaluates regional myocardial perfusion and coronary arteries, respectively, are reliable and non-invasive methods in terms of coronary artery disease. In this study we aimed to compare MPS and CTCA based on conventional coronary angiography (CCA). Totally 60 patients were included in the study. CCA and MPS were performed to 30 patients; CCA and CTCA were performed to the rest of the patients (30 patients). Lesions were classified as mild, moderate and severe in these imaging methods. MPS and CTCA were compared with CCA by using chi-square and Fisher’s exact test. MPS and CTCA’s p values were found for left anterior descending artery (LAD) p: 0, p: 0.271; for circumflex artery (Cx) p: 0.256, p: 0.08 and for right coronary artery (RCA) p: 0.033, p: 0.271, respectively. Furthermore MPS and CTCA’s sensitivity, specificity, accuracy, positive predictive value and negative predictive value were calculated 81% to 87%; 70% to 49%; 73% to 72%; 54% to 72%; 90% to 71%, respectively. CCA results were found more concordant with MPS for LAD and RCA lesions and more concordant with CTCA for Cx lesions. It was also found that positive predictive value of MPS and negative predictive value of CTCA were significantly higher than the others. As a result, MPS and CTCA were suggested as complementary techniques for the diagnosis of coronary artery disease, not as alternatives to each other.
1. INTRODUCTION
Coronary artery disease is the most common and one of the most important health problems. It is the obstruction of the coronary arteries feeding the heart muscle because of the hardening of the arteries which is called atherosclerosis. Ischemia, the most important feature of this disease at an early stage, may occur in myocardial tissue and life-threatening myocardial infarction usually develops in the later stages. Therefore, early diagnosis of this disease is very important in terms of the treatment without severe myocardial injury.
History of the patient is also very important in the coronary artery diseases as the other diseases. The majority of patients refers to the doctor with chest pain. However, the cause of chest pain is a subjective criteria, as well as may be cardiac or non-cardiac causes. Therefore, the cause of chest pain has to be exactly determined whether if it is cardiac origin or not.
Many non-invasive examinations have been developed for the diagnosis of coronary artery disease. Algorithms for diagnosis in routine practice are as follows: resting electrocardiogram (ECG), exercise stress test, myocardial perfusion scintigraphy (MPS) and computed tomography coronary angiography (CTCA), respectively. However, because of resting ECG and exercise stress test have low level of specificity, both examinations are also insufficient in determination of the localization of focal ischemia [1]. For this purpose, further examinations such as MPS and/or CTCA are admitted to the patients whose tests were positive or suspicious.
Our aim in this study is to evaluate MPS and CTCA, comparing with conventional coronary angiography (CCA), which is the gold standard method for diagnosis of coronary artery disease, and to compare the efficacy of these two different imaging methods in the diagnosis of coronary artery disease.
2. MATERIALS AND METHODS
Totally 60 patients who were followed with the suspicion of coronary artery disease were included in this study. 30 patients with positive MPS and/or severe cardiac symptoms and other 30 patients who have positive CTCA and/or severe cardiac symptoms underwent coronary angiography. Groups were designed as the Group A and B involving the patients with both CTCA and CCA and the patients with both MPS and CCA, respectively. This study is approved by the institutional ethical committee and has been conducted according to the princeples of the Declaration of Helsinki. All patients signed a consent form after detailed information about the study.
To perform MPS, beta blockers and calcium channel blockers and nitrates were stopped 48 - 72 hours and 12 hours respectively, prior the test. Imaging was performed after at least 6 hours fasting period. However, the patients ate/drunk chocolate and milk approximately 15 minutes after radiopharmaceutical injection to remove gallbladder activity in both stress and rest imaging. MPS was performed in two stages as stress and rest condition according to one day protocol. Technetium-99m sestamibi was injected intravenously 10 mCi (370 MBq) and 25 mCi (925 MBq) for stress and rest imaging, respectively. The patients were kept in rest at least 4 hours before rest imaging which was performed after stress imaging.
Exercise stress test was done to the patients by treadmill according to standard Bruce protocol through monitoring 12-lead ECG. When reached 85% of the estimated maximum heart rate, Tc-99m sestamibi was injected; exercise was continued one more minute and then stress test was terminated.
Parallel-hole, low-energy, high resolution collimator integrated with double head SPECT gamma camera (GE Infinia) was used in scintigraphic study. Single photon emission computed tomography (SPECT) imaging in 180-degree was performed (i.e. started from 45 degrees right anterior oblique and completed at the 45-degree left posterior oblique) while the patient was lying in both supine and prone position for stress imaging and in supine position for rest imaging. Raw data for both the supine and prone position were obtained (totally 60 images in 64 × 64 matrices at each 3˚) 25 sec/image and 20 sec/image for stress and rest imaging, respectively. Then short axis (SA), horizontal long axis (HLA) and vertical long axis (VLA) sections of raw images were reconstructed on Xeleris workstation in gamma camera system by using Myovation program (butterword filter, 0.5 frequency). Stress and rest myocardial perfusion images were evaluated visually and were classified as mild, moderate and severe.
CTCA examinations of the patients were performed using 64-slice CT device (Toshiba Aquilion 64, Japan) with 0.5 mm slice-width and 120 kV - 400 mA and 135 kV - 400 mA was used as the energy level in patients less than 100 kg and equal or over 100 kg in weight, respectively. Lesions in coronary arteries were evaluated visually and they were reported directly as mild, moderate and severe and as a percentage (i.e. mild, moderate and severe if they were 50% and lower, between 50% - 70% and over 70%, respectively).
CCA of the patients was performed using a standard 6 F Judkins left and right catheters with femoral artery puncture. At least four projections for the left coronary system and at least two projections for the right coronary system were taken and stored in the digital memory. When a coronary artery lesion were visualized, quantitative coronary measurements were performed through a digital memory using the Automated Coronary Analysis computer software for the suspicious lesion. Calibration was performed utilizing the diameter of the catheter to estimate the actual lumen width value of coronary artery. Later, these detected lesions were classified as in CTCA.
Lesions observed in circumflex, right main coronary and left anterior descending coronary artery were classified as mild, moderate and severe on vascular basis and also regarding the presence of mild-moderate ischemia and severe ischemia in MPS for each patient. According to this classification, the results of CCA were compared with both CTCA and MPS results using chi-square and Fisher’s exact chi-square tests. p < 0.05 was considered statistically significant. Moreover, sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) of the CTCA and MPS were calculated based on CCA.
3. RESULTS
The average age of 30 male patients and 30 female patients who participated in our study were 54.1 years (age range: 28 - 79) and 51.3 years (age range: 19 - 73 years), respectively.
Obesity was the most frequent risk factor in both groups (22/30 patients in Group A, 21/30 patients in Group B). Hyperlipidemia (22/30 patients) in Group A and smoking (14/30 patients) in Group B were the second frequent risk factors. The other risk factors were hypertension, diabetes and family history of cardiovasculary disease for both groups.
Number of the patients with the lesions in LAD, Cx or RCA (classified as normal, mild, moderate and severe according to severity of the lesions) in Group A were summarized in Table 1.
Likewise of Table 1, number of the patients with the lesions in LAD, Cx or RCA (classified as normal, mild, moderate and severe according to severity of the lesions) in Group B were summarized in Table 2.
Moreover, CTCA and CCA examinations were statistically compared with the chi-square test and p values for LAD, Cx and RCA as follows: p = 0.271, p = 0.08 and p = 0.271, respectively.
In the same way, also MPS was compared with CCA using chi-square test and p values were found as p = 0, p = 0.256 and p = 0.033 for the LAD, Cx and RCA, respectively. And also, when the patients were grouped as with diabetes and without diabetes and compared, p values were as follows: p = 0.083, p = 0 for LAD; p = 0.237p = 0.08 for Cx and p = 0.223, p = 0.114 for RCA, respectively. Higher concordance was determined between two tests for the patients without diabetes. In the same way, the patients were also grouped only for RCA as with obesity and without obesity; the comparison was performed between this groups and p values were found as p = 0.237, p = 0.04, respectively. It can be said that higher concordance was determined between two tests for patients without obesity.
The efficacy of CTCA and MPS in determining the lesions were evaluated and the results were summarized in Table 3.
Sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) of CTCA and MPS were also calculated and the results were summarized in Table 4.
4. DISCUSSION
CCA is an invasive method and could lead to serious complications, which is even death although rare (overall complication rate 1.8%, mortality rate 0.1%) [2,3]. Patients experience stressful procedures for catheterization.
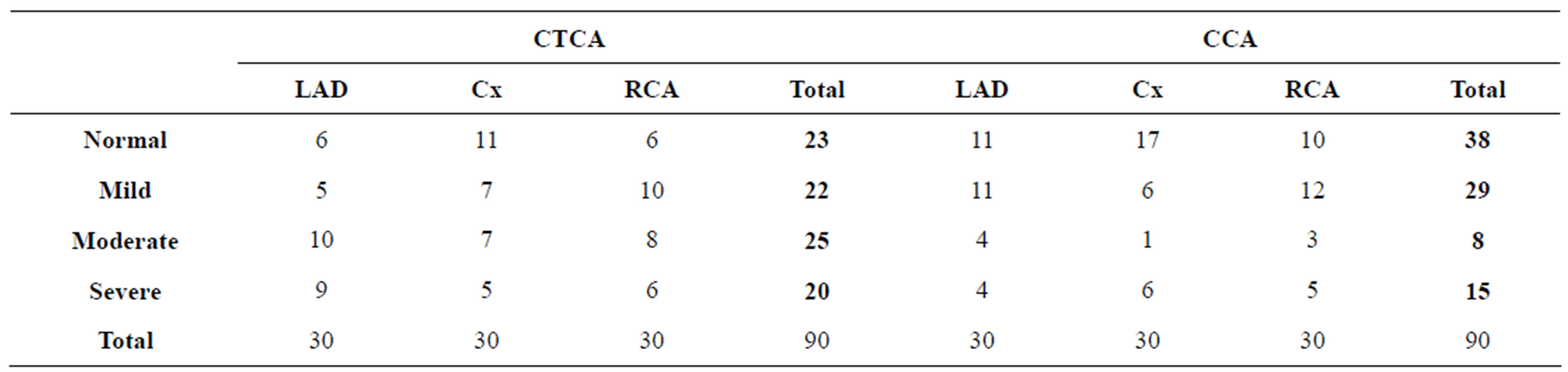
Table 1. Patients distribution according to the severity of the lesions in LAD, Cx and RCA in Group A.
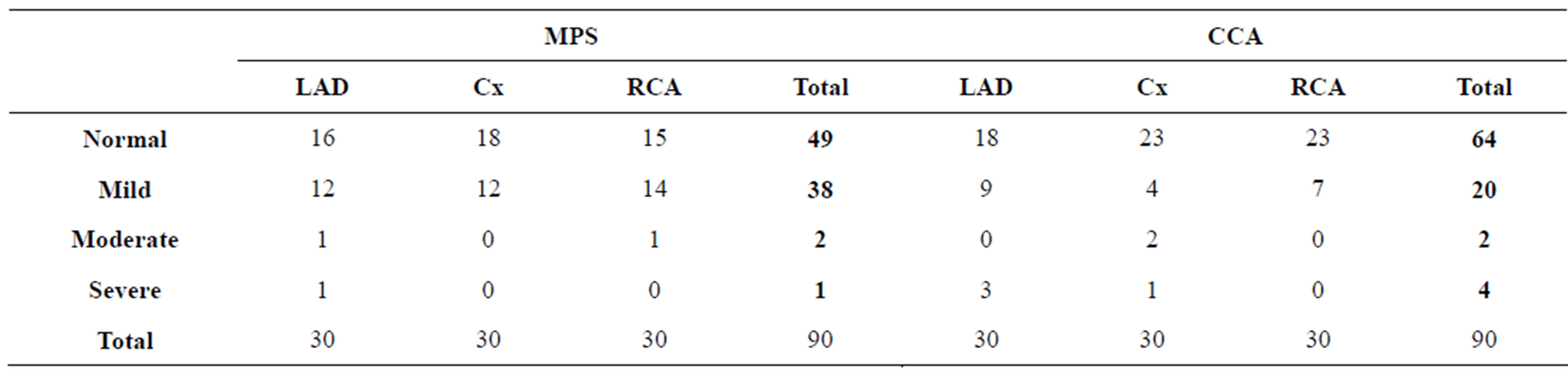
Table 2. Patients distribution according to the severity of the lesions in LAD, Cx and RCA in Group B.
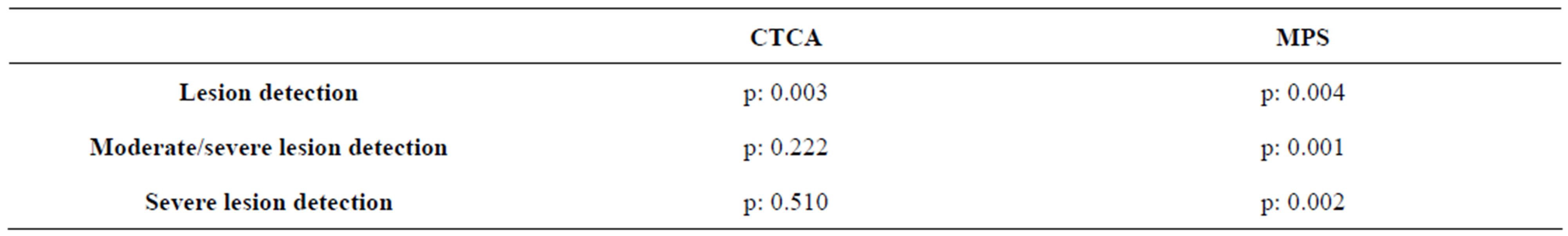
Table 3. Efficacy of CTCA and MPS examinations in determining severity of the lesions.
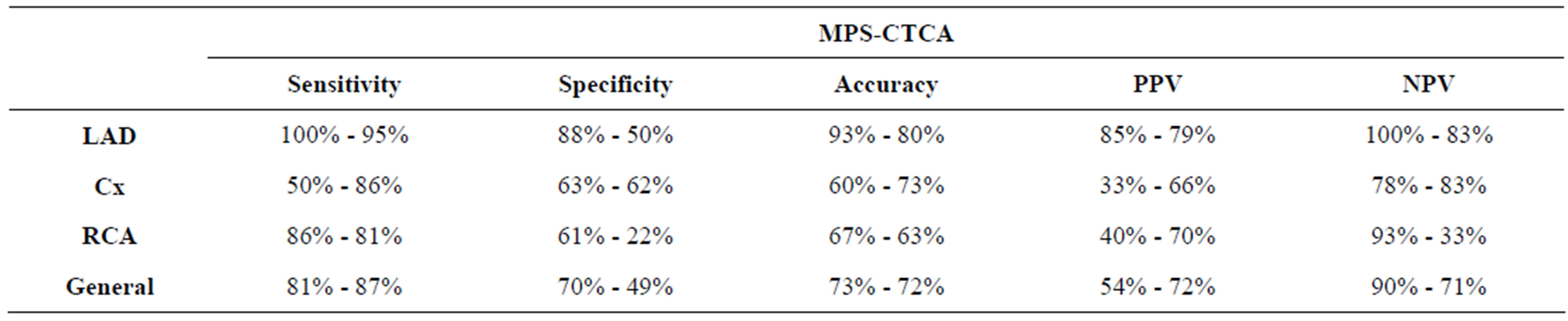
Table 4. Sensitivity, specificity, accuracy, PPV and NPV of MPS and CTCA.
More importantly, significant coronary artery stenosis is not determined on, at least 20% - 30% of the CCA performed for diagnostic purposes, and interventional treatment is applied to only 30% of the patients in the same session [4]. Since CCA is invasive although it is the gold standard method in terms of diagnosis and treatment of coronary artery disease, it has a great importance to determine healthy individuals by means of non-invasive examinations before CCA. MPS and CTCA are used for this purpose and the main accepted examinations in terms of non-invasive diagnosis of coronary artery disease [5].
CTCA, which allows the detection of coronary artery obstruction with minimal invasive procedure, is a new method and gaining popularity [6]. Since it is non-invasive and can be done very quickly, it is extremely comfortable for the patient and does not require hospitalization. Besides CTCA, in addition to conventional CCA, not only provided the lumen information but at the same time allows to evaluate the wall of vessel, to identify the plate character and to demonstrate the atherosclerotic changes in the vessel wall even in the condition of no critical narrowing happened [7-11].
In a meta-analysis which was recently published by Stein et al., evaluable coronary artery percentage was reported 78% in 4-slice CT, 91% in 16-slice CT and 100% in 64-slice CT. The average sensitivity and specificity rates with 16-slice CT for determining critical stenosis were determined 95% and 84%, respectively [12]. As proximal as and as higher degree as the stenosis, as higher as the detectability of the lesion is possible for CTCA. In the study which was done by Hoffman et al. with 16- slice CT, sensitivity and specificity in the evaluation of stenosis of the proximal segments were found as 93% and 94%, respectively [13]. Sensitivity, specificity, PPV and NPV for determining stenosis for all segments were established as 63%, 96%, 64% and 96%, respectively, in the same study in which 530 segments were evaluated. Sensitivity and specificity of CTCA has been reported as 71% - 95% and 86% - 98%, respectively, in other similar studies which had been done before [14-16].
The sensitivity, specificity, accuracy, PPV and NPD of the CTCA with 64-slice CT were found as 87%, 49%, 72%, 72% and 71%, respectively in our study. Although the results have come close to literature, the specificity value was lower than the reported in literature [14-16]. A possible reason for this can be adversely affected of the specificity due to majority of patients with normal CTCA who did not be included in the study because of ethical aspect.
Severe coronary calcification causes artifacts in CTCA as a result of partial volume effect and beam hardening and therefore the plaque size and stenosis can be evaluated larger than they are. Also it may hinder to evaluate lumen integrity reliably in case of high calcium density. As a result of these, CTCA can assess severity of stenosis more than it is, especially in calcified vessels [17]. In general, the severity of lesions in CTCA were also found one more degree severe than in CCA in our study. For example, although there was a statistical concordance (p: 0.003) between CTCA and CCA for determining lesions, we could not find any statistical adjustment in none of three coronary arteries according to lesion’s severity (p: 0.271 for LAD, p: 0.08 for Cx, p: 0.271 for RCA). Another reason may be that classification of lesions had been generally made visually by clinicians.
Artifacts which can be created in CTCA images should not be also ignored. Indeed, the CT images can be influenced especially by high heart rates (>70 - 75 beats/ minute) and respiratory movements [18,19]. The use of beta blockers, by reducing heart rate, provides rising in both evaluable number of segments and sensitivity of CTCA to identify blockage in the vessels [20]. Although beta blockers was used to reduce heart rate in patients and patients were asked to hold breath during the CTCA, the optimal conditions may not be fully achieved. Obtaining CTCA images with retrospective ECG gating technique is another reason of artifact and almost all patients can be affected slightly by cardiac motion [21].
MPS which is another diagnostic method for coronary artery disease, is safe, reliable, non-invasive and widely use examination to evaluate regional myocardial perfusion. It enables the diagnosis of myocardial ischemia in the myocardial regions supplied by stenotic coronary artery by demonstrating a reversible decrease of radiopharmaceutical uptake in the myocardium on the peak point of stress relative to rest [22].
Sensitivity and specificity of MPS for detection of coronary artery disease were evaluated in many studies and in these studies, CCA was usually used as a standard to evaluate the accuracy of scintigraphy. The precision of this approach is questionable. However, although angiography is less appropriate for the evaluation of coronary function, at least, it offers an universal standard for the evaluation of coronary anatomy [22,23].
Published figures are quite different for the sensitivity and specificity of MPS in the diagnosis of coronary artery disease. It depends on different parameters such as studied population (e.g. gender, age, symptoms, drug therapy, presence of previous infarction etc.), imaging method (planar or SPECT, qualitative or semi-quantitative analysis) and also institutional experience. However, if it is performed under suitable conditions, MPS is an effective method for detecting ischemic heart disease and if SPECT technique is used, the sensitivity and specificity are increased up to 91% and 89%, respectively [22].
In our research, we also compared the MPS and CCA in terms of the severity of all three coronary artery lesions. A correlation was observed statistically in both studies regarding LAD and RCA, however there was no correlation regarding the Cx artery (for LAD p: 0, for RCA p: 0.033, for Cx p: 0.256). Besides sensitivity, specificity, accuracy, PPV and NPV were found as the best for LAD and better for RCA than Cx. The values were found in general as 81%, 70%, 73%, 54%, 90%, respectively, for all three vessels. The low specificity and PPV might be caused by not being able to include some of the patients with normal MPS due to ethical and algorithmic reasons as with the same reason of the CTCACCA comparison.
A major limitation of MPS is partial impairment in its specificity due to various soft tissue attenuation artifacts. Main attenuation artifacts are breast tissue for the anterior wall and diaphragm attenuation for inferior wall. In our study, while the breast was lifted up and fixed with bandages to avoid the anterior wall attenuation which arisen due to breast tissue, imaging in prone position were additionally performed to remove the inferior wall attenuation. In terms of the effects of the diaphragm attenuation observed on the inferior wall, patients were especially evaluated for RCA in two groups as those who were obese or not. In spite of images in prone position, there was no statistical correlation between MPS and CCA for the obese patients (p: 0.237) although statistical correlation was observed for those without obesity (p: 0.04).
Another vessel segments which are effected with the diaphragm attenuation is Cx artery. That is probably why we had low sensitivity for Cx (i.e. depending on the wrong positive evaluations) and thus, statistical correlation was not observed between MPS and CCA groups. As a matter of fact, in some of the previous reports, the sensitivity of MPS for Cx region was found to be around 50% just like our study [24-29]. For example, while one of these studies has reported a 75% sensitivity in LAD area, much lower sensitivity scores (40%) for Cx and RCA has been stated [29]. And this situation was dedicated to very large blood supplying area of LAD compared to the area of RCA and Cx, and lower inter-vessel flow heterogeneity of LAD [29]. Just like in our study, Elhendy et al. also stated in a review about the importance of MPS in coroner artery disease that MPS had the lowest sensitivity score in Cx supplying area and the lower specificity score in RCA supplying area. The lowest specificity score in RCA area was explained with the rise in wrong negative results related to the diaphragm attenuation on inferior wall, and the lowest sensitivity score in Cx artery area was explained with the variations of coroner anatomy (i.e. Cx artery bleeding area can be smaller in some patients and the vascular connections can be possible between RCA and Cx artery) [30].
Diabetes is a disease that can affect smaller vessels as well as large vessels and the involving of smaller vessels in diabetes is called microangiopathy. Until recently, it was assumed that the ischemic heart disease was caused by the diseases of large vessels, especially the coronary arteries. However, it is now known that coronary microcirculation abnormalities can contribute to arising of the ischemia even without a visible disease in big epicardial arteries. An abnormal reserve of perfusion can be a result of the contraction of epicardial coronary arteries, or it can show a coronary microcirculation dysfunction when there are no angiographically visible atherosclerotic diseases [1]. Consequently, the ischemic tissue in patients with microangiopathy without coroner artery involvement can be detected with MPS, whereas pathological condition can be skipped by CCA since the CCA only evaluates coronary arteries and the main branches. This may be the reason for the low correlation between MPS and CCA with diabetes patients’ group in our study. It has been stated long years ago that not all of the lesions that are determined in CCA were physiologically important. Therefore MPS is the most suitable non-invasive diagnostic test for the determination of the physiological importance of borderline lesions [31].
Patients with diabetes are the group with the highest risk in terms of coronary artery disease and the early diagnosis of cardiovasculary disease is essential. MPS is a method which has high sensitivity for evaluating patients with diabetes in asymptomatic period [31]. In a large study by Kang et al. including 1271 patients with diabetes, subjects with normal MPS had 1% - 2% cardiovascular events in a year whereas the group with abnormal data had incidence more than 7% [32].
When diabetes is considered in our patients, the p rates according to the existence and absence of diabetes have been spotted as p: 0.083 and p: 0 for LAD, p: 0.237 and p: 0.08 for Cx, p: 0.223 and p: 0.114 for RCA, respectively. These results clearly show that the statistical concordance is higher for MPS and CCA in the patients without diabetes.
Besides the intensity of lesions in main coroner artery, MPS was compared with CCA according to definition of mild, medium-serious or serious lesions in patients, and statistical compliance was spotted in all three comparesons (p: 0.004 for the lesion definition, p: 0.001 for medium-serious lesions and p: 0.002 for serious lesions). Even though evaluation for all three lesion level had significant results, much higher statistical compliance was observed between MPS and CCA especially in the medium-serious lesions.
In our study although sensitivity (87% in CTCA, 81% in MPS) and accuracy (72% in CTCA, 73% in MPS) scores for CTCA and MPS were found in similar values, specificity of CTCA was defined quite lower than MPS (49% in CTCA, 70% in MPS). The reason for this might be that the number of patients with normal CTCA involved in the study was also quite lower than those patients with normal MPS (number of patients with normal CTCA: 2, number of patients with normal MPS: 6).
Another significant result of our study was that NPV of MPS was significantly higher than that of CTCA (71% for CTCA, 90% for MPS) and PPV of CTCA was significantly higher than that of MPS (72% for CTCA, 54% for MPS). NPV is a very important parameter for the scanning tests. Because the real purpose of scanning tests is to define the patients who do not need the further examination. So higher the NPV is for a test, lower the possibility of a person with a disease to be left undiagnosed. In our study, MPS achieved this better than CTCA, showing extraordinary NPV results. But PPV, which prevents patients from further unnecessary examinations, is also not a parameter to be skipped or underrated and CTCA gave better results for this parameter compared with MPS. Without such studies, patients that are supposed as abnormal is experienced a higher examination, which may provide data about PPV, whereas there is no data about NPV on cases which are considered normal since there are no further examinations done. Thus clinicians can determine the higher PPV of CTCA compared to MPS, however the very high NPV of MPS does not stand out. So if the clinician is left with a choice between two examinations, it is perfectly natural to choose the CTCA. However, while the clinicians are choosing the diagnostic test with high PPV, they have to always consider and question in order to not to miss out the patients who actually have disease, that the NPV scores of the chosen test might be low.
5. CONCLUSIONS
Both MPS and CTCA are diagnostic methods with a high sensitivity and specificity for the determination of healthy individuals before the coronary angiography, which is an invasive approach. Today, with the more common usage of these diagnostic methods, CCA is almost exclusively used for the treatment of coronary heart disease instead of diagnosing it.
MPS is an examination for the evaluation of myocardial ischemia and CTCA is for the examination of coronary stenosis, and these two methods are actually complementary to each other in terms of clinical management. In our study, MPS has been determined more concordant with CCA for LAD and RCA lesions, and CTCA for Cx lesions. PPV of CTCA and NPV of MPS was found clearly higher. Therefore, before a decision to perform CCA, evaluating both of them seems to be the better approach instead of choosing one of them.
REFERENCES
- Crea, F., Camici, P.G., De Caterina, R. and Lanza, G.A. (2006) Chronic ischaemic heart disease. In: Camm, A.J., Luescher, T.F. and Serruys, P.W., Eds., The ESC Textbook of Cardiovascular Medicine, Blackwell Publishing Ltd., Oxford, 391-424.
- Bashore, T.M., Bates, E.R., Berger, P.B., et al. (2001) American College of Cardiology/Society for Cardiac Angiography and Interventions clinical expert consensus document on cardiac catheterization laboratory standards. A report of the American College of Cardiology Task Force on clinical expert consensus documents. Journal of the American College of Cardiology, 37, 2170-2214. doi:10.1016/S0735-1097(01)01346-8
- Scanlon, P.J., Faxon, D.P., Audet, A.M., et al. (1999) ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. Journal of the American College of Cardiology, 33, 1756-1824. doi:10.1016/S0735-1097(99)00126-6
- Johnson, L.W., Lozner, E.C., Johnson, S., et al. (1989) Coronary arteriography 1984-1987: A report of the registry of the society for cardiac angiography and interventions. I. Results and complications. Catheterization and Cardiovascular Diagnosis, 17, 5-10. doi:10.1002/ccd.1810170103
- Gaemperli, O., Schepis, T., Valenta, I., et al. (2007) Cardiac image fusion from stand-alone SPECT and CT: Clinical experience. Journal of Nuclear Medicine, 48, 696- 703. doi:10.2967/jnumed.106.037606
- Lau, G.T., Ridley, L.J., Schieb, M.C., et al. (2005) Coronary artery stenoses: Detection with calcium scoring, CT angiography, and both methods combined. Radiology, 235, 415-422. doi:10.1148/radiol.2352031813
- Schoenhagen, P., Halliburton, S.S., Stillman, A.E., et al. (2004) Noninvasive imaging of coronary arteries: Current and future role of multi detector row CT. Radiology, 232, 7-17. doi:10.1148/radiol.2321021803
- Schoepf, U.J., Becker, C., Ohnesorge, B.M. and Yucel, K. (2004) CT of coronary arter disease. Radiology, 232, 18- 37. doi:10.1148/radiol.2321030636
- Achenbach, S. (2007) Cardiac CT: State of the art for the detection of coronary arterial stenosis. Journal of Cardiovascular Computed Tomography, 1, 3-20. doi:10.1016/j.jcct.2007.04.007
- Lawler, L.P., Pannu, H.K. and Fishman, E.K. (2005) MDCT evaluation of the coronary arteries, 2004: How we do it—Data acquisition, postprocessing, display, and interpretation. American Journal of Roentgenology, 184, 1402-1412.
- Schoepf, P.D., Zwerner, P.L., Savino, G., Herzog, C., Kerl, J.M. and Costello, P. (2007) Coronary CT angiography. Radiology, 244, 48-63. doi:10.1148/radiol.2441052145
- Stein, P.D., Beemath, A., Kayali, F., Skaf, E., Sanchez, J. and Olson, R.E. (2006) Multidetector computed tomography for the diagnosis of coronary artery disease: A systematic review. American Journal of Medicine, 119, 203-216. doi:10.1016/j.amjmed.2005.06.071
- Hoffmann, U., Moselewski, F., Cury, R.C., et al. (2004) Predictive value of 16-slice multidetector spiral computed tomography to detect significant obstructive coronary artery disease in patients at high risk for coronary artery disease. Circulation, 110, 2638-2643. doi:10.1161/01.CIR.0000145614.07427.9F
- Nieman, K., Cademartiri, F., Lemos, P.A., et al. (2002) Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation, 106, 2051-2054. doi:10.1161/01.CIR.0000037222.58317.3D
- Ropers, D., Baum, U., Pohle, K., et al. (2003) Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation, 107, 664-666. doi:10.1161/01.CIR.0000055738.31551.A9
- Knez, A., Becker, C.R., Leber, A., et al. (2001) Usefulness of multislice spiral computed tomography angiography for determination of coronary artery stenoses. American Journal of Cardiology, 88, 1191-1194. doi:10.1016/S0002-9149(01)02060-4
- Feyter, P.J. and Achenbach, S. (2006) Cardiovascular computerized tomography. In: Camm, A.J., Luescher, T.F. and Serruys, P.W., Eds., The ESC Textbook of Cardiovascular Medicine, Blackwell Publishing Ltd., Oxford, 115- 139.
- Choi, H.S., Choi, B.W., Choe, K.O., et al. (2004) Pitfalls, artifacts and remedies in multi-detector row CT coronary angiography. Radiographics, 24, 787-800. doi:10.1148/rg.243035502
- Nakanishi, T., Kayashima, Y., Inoue, R., Sumii, K. and Gomyo, Y. (2005) Pitfalls in 16 detector row CT of the coronary arteries. Radiographics, 25, 425-440. doi:10.1148/rg.252045098
- Nieman, K., Rensing, B.J., van Geuns, R.J.M., et al. (2002) Non-invasive coronary angiography with multislice spiral computed tomography: Impact of heart rate. Heart, 88, 470-474. doi:10.1136/heart.88.5.470
- Giesler, T., Baum, U., Ropers, D., et al. (2002) Noninvasive visualization of coronary arteries using contrast-enhanced multidetector CT: Influence of heart rate on image quality and stenosis detection. American Journal of Roentgenology, 179, 911-916.
- Kaufmann, P.A., Camici, P.G. and Underwood, S.R. (2006) Nuclear cardiology. In: Camm, A.J., Luescher, T.F. and Serruys, P.W., Eds., The ESC Textbook of Cardiovascular Medicine, Blackwell Publishing Ltd., Oxford, 141-159.
- Zaret, B.L., Rigo, P., Wackers, F.J.T., et al. (1995) Myocardial perfusion imaging with Tc-99m tetrofosmin comparison to Tl-201 imaging and coronary angiography in a phase III multicenter trial. Circulation, 91, 313-319. doi:10.1161/01.CIR.91.2.313
- Geleijnse, M.L., Elhendy, A., Fioretti, P.M. and Roelandt, J.R.T.C. (2000) Dobutamine stress myocardial perfusion imaging. Journal of the American College of Cardiology, 36, 2017-2027. doi:10.1016/S0735-1097(00)01012-3
- Elhendy, A., van Domburg, R.T., Bax, J.J., et al. (1998) Noninvasive diagnosis of coronary artery stenosis in women with limited exercise capacity. Chest, 114, 1097- 1104. doi:10.1378/chest.114.4.1097
- Boomsma, M.M., Niemeyer, M.G., van der Wall, E.E., et al. (1998) Tc99m tetrofosmin myocardial SPECT perfusion imaging: comparison of rest-stress and stress-rest protocols. The International Journal of Cardiac Imaging, 14, 105-111. doi:10.1023/A:1005930200119
- Tamaki, N., Takahashi, N., Kawamoto, M., et al. (1994) Myocardial tomography using technetium-99m-tetrofosmin to evaluate coronary artery disease. Journal of Nuclear Medicine, 35, 594-600.
- Bai, J., Hashimoto, J., Suzuki, T., et al. (2001) Comparison of image reconstruction algorithms in myocardial perfusion scintigraphy. Annals of Nuclear Medicine, 15, 79-83. doi:10.1007/BF03012138
- Elhendy, A., van Domburg, R.T., Bax, J.J., Poldermans, D., Sozzi, F.B. and Roelandt, J.R.T.C. (2000) Accuracy of dobutamine technetium 99m sestamibi SPECT imaging for the diagnosis of single-vessel coronary artery disease: comparison with echocardiography. American Heart Journal, 139, 224-230.
- Elhendy, A., Bax, J.J. and Poldermans, D. (2002) Dobutamine stress myocardial perfusion imaging in coronary artery disease. Journal of Nuclear Medicine, 43, 1634-1646.
- Unlü, M. (2008) Myocardial perfusion scintigraphy in the diagnosis and prognostic assessment of coronary artery disease: SPET and PET. Anatolian Journal of Cardiology, 8, 5-11.
- Kang, X., Berman, D.S., Lewin, H.C., et al. (1999) Incremental prognostic value of myocardial perfusion single photon emission computed tomography in patients with diabetes mellitus. American Heart Journal, 138, 1025-1032. doi:10.1016/S0002-8703(99)70066-9
NOTES
*This study was presented as an oral presentation in Annual Congress of the European Association of Nuclear Medicine (EANM) 2010, Vienna, Austria.

