Health
Vol. 4 No. 6 (2012) , Article ID: 19705 , 7 pages DOI:10.4236/health.2012.46049
Prevalence of daily or near daily aspirin use by US adults with diabetes: A cross-sectional study using a multi-year national database
![]()
1Ambulatory Care Residency Program, College of Pharmacy, University of Minnesota, Minneapolis, USA;
*Corresponding Author: mlutfiyya@eirh.org
2Essentia Institute of Rural Health, Duluth, USA
Received 4 March 2012; revised 3 April 2012; accepted 10 April 2012
Keywords: Aspirin Use; CVD Prevention; Diabetes; Practice Guidelines
ABSTRACT
Introduction: For persons with diabetes, cardiovascular disease is the major cause of morbidity and mortality that is reflected in a two-tofour times greater risk for both heart disease and stroke when compared to adults without diabetes. Although not without controversy, diabetes and cardiovascular disease (CVD) management guidelines in the US recommend the use of once-daily aspirin. This epidemiological study was undertaken to fill the knowledge gap regarding the prevalence of daily or near daily aspirin use for US age-appropriate adults with diabetes. Methods: Using bivariate and multivariate techniques, a cross-sectional analysis of an amalgamated database using 2005, 2007, and 2009 Behavioral Risk Factor Surveillance Survey data was performed. The dependent variable for this analysis was daily or near daily aspirin use. The population of interest was US adults, men >= 45 - 79 and women >= 55 - 79 years of age. Results: Overall the prevalence of daily or near daily aspirin use by age-appropriate US adults with diabetes was 62.5%; it was 41.0% for similar non-diabetic adults. Logistic regression analysis yielded that age-appropriate adults, of both genders, with diabetes taking daily or near daily aspirin were more likely to be: physically active, male, live in rural locales, not have a health care provider, have deferred medical care because of cost, have an elevated BMI, a smoker, and have hypertension. Conclusion: It was determined that the age-appropriate use of aspirin in the US adult population with diabetes is underutilized. The role of the pharmacist throughout the continuum of care is one way to improve appropriate aspirin use in patients with diabetes.
1. INTRODUCTION
For persons with diabetes, cardiovascular disease (CVD) is the major cause of morbidity and mortality [1] that is reflected in a two-to-four times greater risk for both heart disease and stroke when compared to adults without diabetes [2]. It is estimated that at least 65% of people with diabetes die from some form of heart disease or stroke [3]. Furthermore, the Adult Treatment Panel (ATP) III report on high cholesterol considers diabetes a coronary heart disease (CHD) risk equivalent due to the high risk of developing CHD within 10 years [4].
The mechanisms behind the increased CVD risk for adults with diabetes are multifactorial and not completely understood. The factors thought to play a role include: impaired endothelial function, subclinical inflammation, changes in adipokines, development of atherogenic dyslipidemia, increased levels of free fatty acids, and changes in thrombosis and fibrinolysis [5]. The latter of these proposed mechanisms is thought to be related to the impaired endothelial function. This leads to suppressed nitric oxide production and prostacyclin synthesis resulting in increased platelet aggregation [5].
Given the increased platelet aggregation and the necessity to reduce morbidity and mortality from cardiovascular causes, aspirin has been recommended for use by people with diabetes in an attempt to reduce the risk of CHD and stroke [1-3]. In a joint statement from the American Diabetes Association (ADA), the American Heart Association (AHA), and the American College of Cardiology Foundation (ACCF), aspirin use for the primary prevention of CVD is recommended in men over age 50 and women over age 60 with diabetes who have at least one major CVD risk factor (i.e., smoking, hypertension, dyslipidemia, albuminuria, family history of premature CVD) [6]. Additionally, since 2002 the US Preventive Task Force (USPTF) has recommended that all adults take daily or near daily aspirin for the primary prevention of CVD. The USPTF makes this recommendation for men between the ages of 45 and 79 years and women 55 through 79 years of age when the potential benefits for CVD risk reduction outweigh the risk for gastrointestinal hemorrhage [7].
While much has been written about the recommended use of aspirin for the prevention of CVD in both the general as well as the adult diabetes populations, there is a paucity of studies regarding the prevalence of aspirin use based on these recommendations. For instance, relying on 1993-2003 data from a large public national database, a 2005 study [8] found that aspirin was underutilized in US ambulatory care settings for both the primary and secondary prevention of CVD. Likewise, Third National Health and Nutrition Examination Survey data from 1988-1994 were analyzed in a 2001 study focusing on aspirin use for the prevention of CVD by US adults with diabetes [9]. This study found that, among adults with diabetes, aspirin was used regularly by 37% who also had CVD, and by 13% of those with CVD risk factors only [9]. Additionally, there have been several studies looking at aspirin use among more narrowly defined populations of US adults, with or without diabetes such as elderly women, [10] or different ethnic and racial groups [11-14].
The purpose of this study was to ascertain the prevalence of daily or near daily aspirin use among age-appropriate US adults with diabetes. The USPTF criterion for age was chosen because it encompassed the broadest age range of all guidelines pertaining to aspirin use for the prevention of CVD. The findings from this study provide an update on the epidemiology of aspirin use for CVD prevention by age-appropriate US adults with diabetes. Since aspirin use remains controversial for the prevention of CVD, this update reflects aspirin use prevalence in age-appropriate US adults with diabetes in light of continually evolving evidence-based recommendations for its use.
2. METHODS
Using bivariate and multivariate techniques, a crosssectional analysis of an amalgamated database using 2005, 2007, and 2009 Behavioral Risk Factor Surveillance Survey (BRFSS) data was performed. BRFSS data are collected using a random-digit dial telephone survey targeting adults 18 - 97 years of age. These data are collected under the guidance of the Centers for Disease Control and Prevention (CDC) in collaboration with all US states and most US territories. All BRFSS data are self-reported responses to mostly forced-choice questions. As recommended by the CDC, all analyses conducted for this study using BRFSS data were performed on weighted data. The weighting provides a stratified representation of the US adult non-institutionalized population and conforms to census data patterns. A detailed description of the survey design and sampling measures can be found elsewhere [15].
BRFSS includes both core modules and optional modules in the survey. All states and US territories collecting BRFSS data must use the core modules; they may choose to include optional modules. Along with data generated from core questions, data from the BRFSS optional module on CVD prevention were used in these analyses. From the CVD prevention module, we were interested in the data generated by the question regarding daily or near daily aspirin use for CVD prevention. Because different states used this module in different years, we merged 2005, 2007, and 2009 data to include as many US states and territories as possible. Data from 29 states and the District of Columbia were used in the analyses performed for this study. If a state used the module more than once, only the data from the most recent year were used. The dependent variable for this analysis was daily or near daily aspirin use. The population of interest was US adults, men aged 45 to 79 years and women aged 55 to 79 years. The covariates for the analysis were: sex, race/ethnicity, household income, education, marital status, geographic locale, timing of last routine medical checkup, have a personal health care provider (HCP), have health insurance, deferment of medical care because of cost, self-defined health status, smoking status, body mass index (BMI), high blood pressure, high cholesterol, physical activity, seasonal flu vaccination, and lifetime pneumococcal vaccination. Almost all of the covariates were originally categorical variables and a number of them were recoded from their original format, mostly in order to collapse categories for analysis.
BMI, calculated or computed from the variables height and weight, was originally a continuous variable. It was recoded into the two categories of: not overweight or obese and overweight or obese. The Metropolitan Statistical Area (MSA) variable included in BRFSS was used to define geographic locale and was recoded into the dichotomous categories of rural or non-rural. Rural residents were defined as people living either within an MSA that had no center city or outside an MSA. Non-rural residents included all respondents living in a center city of an MSA, outside the center city of an MSA but inside the county containing the center city, or inside a suburban county of an MSA.
Race and ethnicity was also a computed variable calculated from participant responses to two separate survey questions—one regarding race and the other regarding Latino/Hispanic ethnicity. By combining the responses to these two questions, it was possible to compute the race and ethnicity variable used in the analyses. All race/ethnicity categories were computed as mutually exclusive. For instance, all respondents coded as Caucasian chose white as their racial classification, likewise black for African American, etc. If a respondent identified themselves as Hispanic, they were classified by that ethnic category regardless of any additional racial classification they may have chosen. The category of other/multi-racial was also calculated. All racial categories were non-Hispanic.
For this research study, the covariates with response categories collapsed into fewer categories were:
• Education (did not graduate from high school (HS)/ graduated from HS/university graduate)
• Household Income (<$50,000/>=$50,000 annually)
• Self-Reported Health Status (fair-to-poor health/ goodto-excellent health)
• Smoking Status (yes/no)
• Have Personal HCP (yes/no)
• Timing of Last Routine Medical Check-up (within the past 12 months/more than 12 months ago)
• Diabetes (yes/no)
Seven additional variables: sex, have health insurance, medical care deferment because of cost, hypertension, hyperlipidemia, seasonal flu vaccine within the past 12 months, and have had pneumococcal vaccine, were also included in the analyses as covariates. The only recoding efforts involved with these variables entailed the removal of missing data.
Bivariate analysis was performed to ascertain the association between daily or near daily aspirin use by age-appropriate adults with diabetes and specific sociodemographic, health service and health status variables. A multivariate logistic regression model was also performed using the same covariates. The dependent variable for the logistic regression model was taking daily or near daily aspirin.
For all statistical analyses, alpha was set at p < 0.05. Statistical Package for Social Scientists (SPSS, IBM, Chicago, IL) version 19.0 was used to complete all statistical analyses performed for this study. Human subject approval was sought and received from Essentia Health’s Institutional Review Board (IRB).
3. RESULTS
The multi-year amalgamated BRFSS database yielded 6,434,246 women 55 - 79 years of age and 8,802,793 men 45 - 79 years of age with 15.3% and 16.8% of the gendered population, respectively. The overall prevalence of daily or near daily aspirin use by age-appropriate US adults with diabetes was 62.5%; for men, the prevalence was 65.5% and women 58.5%. This overall prevalence of aspirin use for CVD prevention by US age-appropriate adults with diabetes was significantly higher than the 41.0% prevalence estimate yielded for similar-aged, non-diabetic adults (Table 1). Additionally, 29.2% of age-appropriate US adults with diabetes and 15.2% of same-aged US adults without diabetes reported that they had been told that aspirin use was unsafe for their health.
Table 2 presents the bivariate analysis of the characteristics of age-appropriate US adults with diabetes taking daily or near daily aspirin. Odd ratios were calculated for all of the dichotomous variables and percentages for variables with more than two factors or categories. The bivariate analysis revealed that those age-appropriate US adults with diabetes taking daily or near daily aspirin for CVD prevention were more likely to be: male, married or living with a partner and at least moderately physically active. They were also more likely to: have health insurance, have a personal health care provider, have hypertension, have had a lifetime pneumonia vaccine, and to have had a seasonal flu shot and a routine medical exam within the last twelve months. Furthermore, at 64.3%, Caucasians constituted the racial/ethnic group with the highest prevalence of age-appropriate adults with diabetes taking daily or near daily aspirin, while Hispanics had the lowest prevalence at 55.2%. In the bivariate analysis conducted, prevalence of aspirin use did not differ significantly by level of attained education.
A multivariate logistic regression model was performed using daily or near daily aspirin use as the dependent variable (Table 3). The population included in the analysis was US adult women ages 55 to 79 years and men 45 to 79 years with diabetes. Logistic regression analysis yielded that age-appropriate adults (of both genders) with diabetes taking daily or near daily aspirin were more likely to be: a smoker, physically active, male, live in rural locales, not have a personal health care provider, have deferred medical care because of cost, have an elevated BMI, and have hypertension.
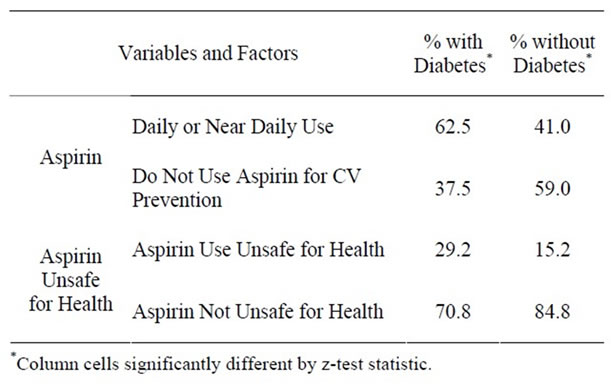
Table 1. Daily or near daily use of aspirin and aspirin safety status by age-appropriate US adults by diabetes status. 2005, 2007 and 2009 BRFSS data.
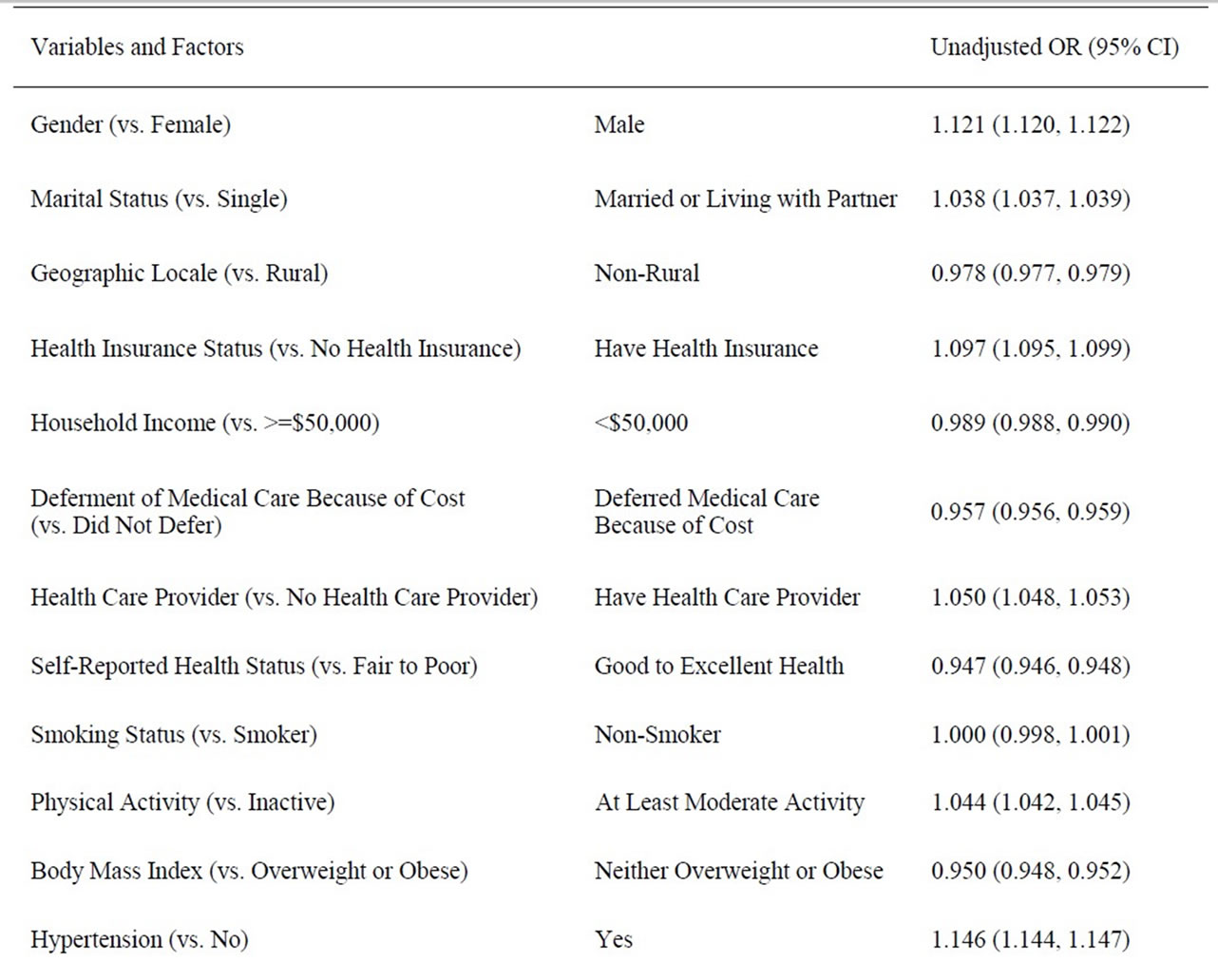
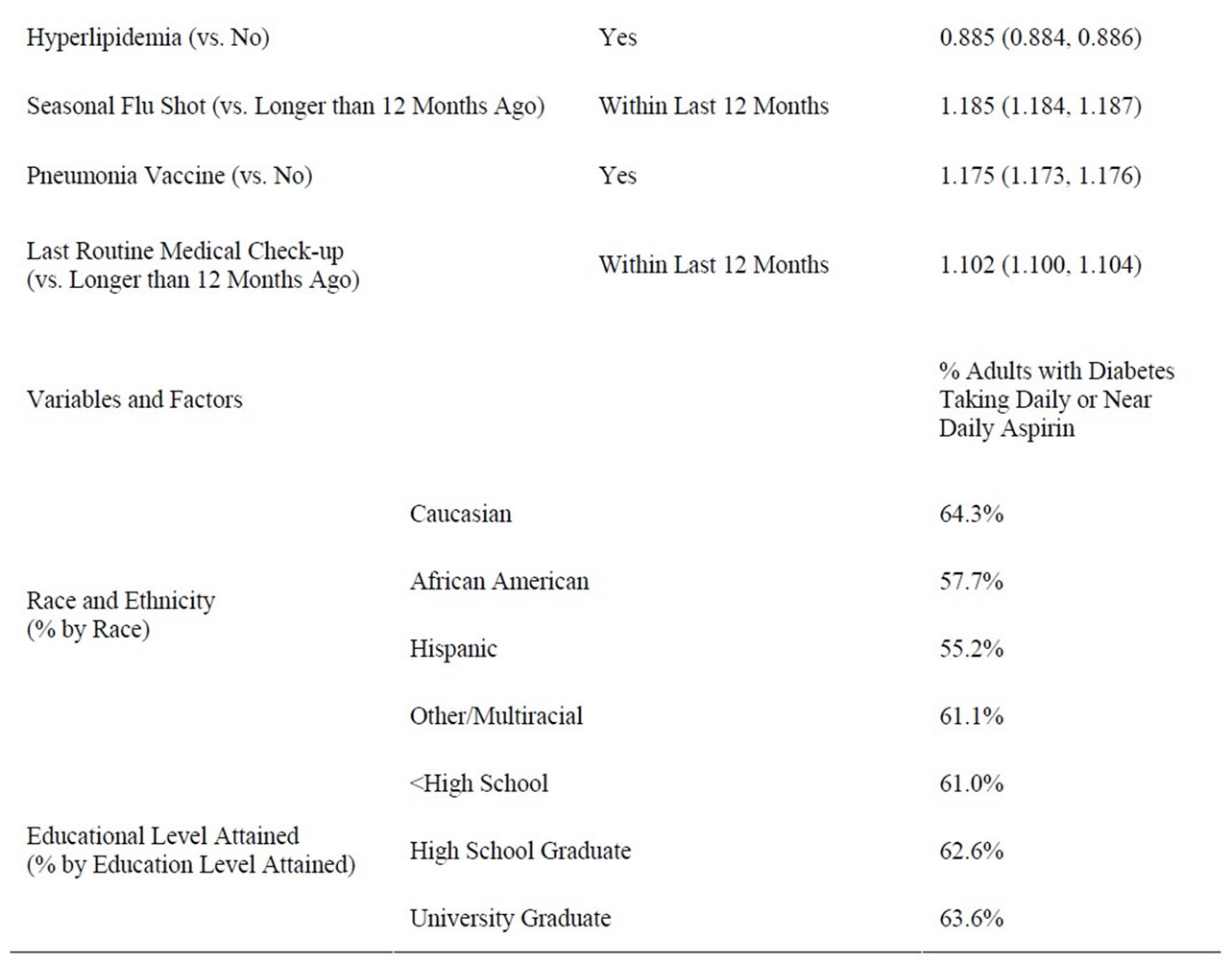
Table 2. Bivariate analysis of characteristics of age-appropriate adults with diabetes taking daily or near daily aspirin. 2005, 2007 and 2009 BRFSS data.

Table 3. Logistic regression analysis of daily or near daily use of aspirin by women 55 - 79 and men 45 - 79 years of age with diabetes. 2005, 2007 and 2009 BRFSS data.
4. DISCUSSION
The CVD risk for US adults with diabetes is considerable [6] leading clinicians and researchers alike to seek avenues for reducing this burden. Multiple studies [16] have indicated that the morbidity and mortality from CVD in high risk groups may be reduced by daily or near daily aspirin use. Aspirin use for the primary and/or secondary prevention of CVD is, however, not without controversy [6]. For instance, despite the implications of some earlier treatment guidelines, [17] not all US adults with diabetes are at high risk for CVD [4]. While the most recent ADA, AHA and ACCF position statement [6] modifies earlier recommendations regarding use of aspirin for the primary prevention of cardiovascular events in adults with diabetes; it remains the case that the US Food and Drug Administration has, to date, not approved aspirin for the primary prevention of CVD. A further contribution to the controversy is the updated USPTF recommendation for the use of aspirin, regardless of diabetes status, for the primary prevention of CVD in age-specific adults [7].
Our findings indicated that the overall prevalence of daily or near daily use of aspirin by US adults differed significantly by diabetes status. Overall 62.5% of ageappropriate (by USPTF criterion) US adults with diabetes, in comparison to 41.0% of those without diabetes, used daily or near daily aspirin. This finding suggests that earlier ADA recommendations, those prior to 2010, [17] appear to have had more of an impact on daily or near daily aspirin use than the USPTF recommendations.
Interestingly, those age-appropriate adults with diabetes using daily or near daily aspirin were also more likely to: have a university degree, have health insurance, be Caucasian, be male, be physically active and live in a household with an annual income of >$50,000. These findings suggest that those age-appropriate US adults with diabetes using aspirin for CVD prevention are among the segment of society who have greater resources—factors that Link and Phalen [18] have identified as those influencing the ability to avoid risks and minimize the consequences of disease once it occurs.
CVD prevention in adults with diabetes remains a public health concern. However, the overall conflicting or inconsistent recommendations for daily or near daily aspirin use makes it difficult for health care providers of all stripes—physicians, nurse practitioners, physician assistants, and pharmacists—as well as patients to determine the appropriate use of aspirin for CVD prevention. Pharmacists may be in one of the better positions to provide patient education regarding aspirin use for CVD prevention in adults with diabetes [19,20].
Pharmacists have the advantage of practicing in multiple health care settings throughout the continuum of care—hospital care teams, primary care clinics, and community pharmacies [21]. As a member of a hospital care team, medication reconciliation offers the opportunity to screen patients with diabetes for appropriate aspirin use for CVD prevention while also providing education at discharge. In primary care clinics, ambulatory care pharmacists conduct complete medication reviews with patients offering yet another opportunity to screen for aspirin appropriateness for patients with diabetes. Finally, a pharmacist in a community setting provides a safety net for those diabetes patients whose needs have not yet been ascertained. For instance, community pharmacists could identify persons with diabetes who would benefit from aspirin therapy. Pharmacists might also choose to refer patients with diabetes to another health care provider, such as a primary care provider, for further evaluation.
Several potential limitations to this study should be noted. First, the survey is based on telephone derived data. Those who could not be reached by phone were not able to participate in the survey administration process. Additionally, with the widespread use of answering machines and caller identification possible participants are now able to filter their phone calls potentially resulting in a passive refusal to participate in surveys such as the BRFSS. Call filtering, however, is beyond the control of survey administrators. Historically, persons of lower socioeconomic status may have been excluded because of poorer phone access. However, the vast majority of US residents live in households with telephones, which minimizes this bias. Moreover, US cell phone numbers are now included in the pool of phones contacted for the survey. Regardless of these issues with the reliance of a telephone to reach survey participants, study strength is in the use of a national database that included a robust sample of residents weighted to reflect the demographics of the US population.
A second limitation is that the survey used close-ended questions. Such questions may limit participants’ options to fully explain response choices. Nonetheless, a wide range of response possibilities are available to the survey questions.
A third, and related, limitation is self-reported nature of the responses to survey questions—introducing the possibility of recall bias on the part of the survey participants.
A fourth limitation is that, given the nature of the survey questions, it was not possible to determine whether or not aspirin was being used for primary or secondary CVD prevention. However, since our basic research purpose was to ascertain the prevalence of daily or near daily aspirin use by age-appropriate adults with diabetes for CVD prevention, this limitation in the data does not compromise our findings. A final potential bias resulted from the languages of the survey—English and Spanish. Individuals who did not speak English or Spanish were excluded from this survey.
5. CONCLUSION
Recommendations for aspirin use remain controversial. This study demonstrated that the age-appropriate use of aspirin in the US adult population with diabetes was underutilized. The role of the pharmacist in the continuum of care is one way to improve appropriate aspirin use in patients with diabetes. This paper should raise awareness for all healthcare providers and underscores the need for patient-centered care and health services research.
![]()
![]()
REFERENCES
- American Diabetes Association (2011) Position statement: Standards of medical care in diabetes—2011. Diabetes Care, 34, S11-S61.
- American Diabetes Association, c1995-2011. Statistics. http://www.diabetes.org/diabetes-basics/diabetes-statistics/?loc=DropDownDB-stats
- Lloyd-Jone, D., Adams, R.J., Brown, T.M., Carnethon, M., Dai, S., De Simone, G., et al. (2010) Heart disease and stroke statistics—2010 update: A report from the American Heart Association. Circulation, 121, e46-e215. doi:10.1161/CIRCULATIONAHA.109.192667
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation, 106, 3143- 3421.
- Laakso, M. (2010) Cardiovascular disease in type 2 diabetes from population to man to mechanisms. Diabetes Care, 33, 442-449. doi:10.2337/dc09-0749
- Pignone, M., Alberts, M.J., Colwell, J.A., Cushman, M., Inzucchi, S.E., Mukherjee, D., et al. (2010) Aspirin for primary prevention of cardiovascular events in people with diabetes. Circulation, 121, 2694-2701. doi:10.1161/CIR.0b013e3181e3b133
- US Preventive Services Task Force (2002) Aspirin for the primary prevention of cardiovascular events: Recommendation and rationale. Annals of Internal Medicine, 136, 157-160.
- Stafford, R.S., Monti, V. and Ma, J. (2005) Underutilization of aspirin persists in US ambulatory care for the secondary and primary prevention of cardiovascular disease. PLoS Medicine, 2, e353. doi:10.1371/journal.pmed.0020353
- Rolka, D.B., Fagot-Campagna, A. and Narayan, K.M. (2001) Aspirin use among adults with diabetes. Diabetes Care, 24, 197-201. doi:10.2337/diacare.24.2.197
- Lee, H.Y., Tong, Y.P., Xing, S. and Cooke, C.E. (2010) Aspirin use in elderly women receiving medication therapy management services. Advances in Therapy, 27, 613- 622. doi:10.1007/s12325-010-0046-1
- Brown, D.W., Shepard, D., Giles, W.H., Greenlund, K.J. and Croft, J.B. (2005) Racial differences in the use of aspirin: An important tool for preventing heart disease and stroke. Ethnicity and Disease, 15, 620-626.
- Berlie, H.D., Hammad, A. and Jaber, L.A. (2007) The use of glucose-lowering agents and aspirin among Arab Americans with diabetes. Ethnicity and Disease, 17, 42- 45.
- Lee, R., Onopa, J., Mau, M.K. and Seto, T.B. (2010) Diabetes care in a predominantly Native Hawaiian and Pacific Islander outpatient population. Hawaii Medical Journal, 69, 28-30.
- Sanchez, D.R., Diez-Roux, A.V., Michos, E.D., Blumenthal, R.S., Schreiner, P.J., Burke, G.L. and Watson, K. (2011) Comparison of the racial/ethnic prevalence of regular aspirin use for the primary prevention of coronary heart disease from the multi-ethnic study of Atherosclerosis. American Journal of Cardiology, 107, 41-46. doi:10.1016/j.amjcard.2010.08.041
- Mokdad, A.H., Stroup, D.F. and Giles, W.H. (2003) Public health surveillance for behavioral risk factors in a changing environment: Recommendations from the behavioral risk factor surveillance team. Morbidity and Mortality Weekly Report, 52, RR09.
- Antithrombotic Trialists’ (ATT) Collaboration (2009) Aspirin in the primary and secondary prevention of vascular disease: Collaborative meta-analysis of individual participant data from randomised trials. Lancet, 373, 1849- 1860. doi:10.1016/S0140-6736(09)60503-1
- Buse, J.B., Ginsberg, H.N., Bakris, G.L., Clark, N.G., Costa, F., Eckel, R., Fonseca, V., Gerstein, H.C., Grundy, S., Nesto, R.W., Pignone, M.P., Plutzky, J., Porte, D., Redberg, R., Stitzel, K.F. and Stone, N.J. (2007) Primary prevention of cardiovascular diseases in people with diabetes mellitus: A scientific statement from the American Heart Association and the American Diabetes Association. Circulation, 115, 114-126. doi:10.1161/CIRCULATIONAHA.106.179294
- Link, B.G. and Phelan, J.C. (1996) Editorial: Understanding sociodemographic differences in health—The role of fundamental social causes. American Journal of Public Health, 86, 471-473. doi:10.2105/AJPH.86.4.471
- Smith, M., Bates, D.W., Bodenheimer, T. and Cleary, P.D. (2010) Why pharmacists belong in the medical home. Health Affairs, 29, 906-913. doi:10.1377/hlthaff.2010.0209
- Goode, K.R. (2006) Change in community pharmacy practice—It is not just coming from the cash register. US Pharmacy Review.
- Krantz, M.J., Berger, J.S. and Hiatt, W.R. (2010) An aspirin a day: Are we barking up the wrong willow tree? Pharmacotherapy, 30, 115-118. doi:10.1592/phco.30.2.115

