Food and Nutrition Sciences
Vol. 2 No. 10 (2011) , Article ID: 16363 , 6 pages DOI:10.4236/fns.2011.210140
Association between Cardiovascular Disease Risk Factor Knowledge and Lifestyle
![]()
1Unit of Epidemiology and Biostatistics, Queen Astrid Military Hospital, Brussels, Belgium; 2Faculty of Physical Education and Physiotherapy, Laboratory for Human Biometrics and Biomechanics, Vrije Universiteit Brussel, Brussels, Belgium; 3Erasmus University College, Brussels, Belgium.
Email: patrick.mullie@skynet.be
Received August 24th, 2011; revised September 23rd, 2011; accepted September 30th, 2011.
Keywords: Cardiovascular Disease Risk Factor Knowledge, Dietary Patterns, Nutritional Assessment, Health Behavior, Nutritional Epidemiology, Public Health
ABSTRACT
Objective: To relate cardiovascular risk factor knowledge to lifestyle. Methods: In this cross-sectional study, food consumption and lifestyle characteristics were recorded using mailed questionnaires. The dietary pattern was described using the Mediterranean Diet Score (MDS). An open ended questionnaire without predefined choices or answers was used to capture cardiovascular knowledge. Results: Lack of physical activity, smoking and eating too much fat were the 3 most cited potential cardiovascular risk factors, while being overweight, eating too much salt and a low consumption of fruits and vegetables were the least cited risk factors. Age, Body Mass Index, physical activity, smoking, income and dietary habits were not consistently associated with knowledge of risk factors. A low socioeconomic position as measured by the indicator education was associated with a lower knowledge of established and modifiable cardiovascular risk factors. Conclusions: Risk factor knowledge, an essential step in prevention of CVD, is not systematically associated with a healthier lifestyle. The findings of this study confirm that there is a gap between risk factor knowledge and lifestyle.
1. Introduction
Cardiovascular diseases (CVD) remain the most important cause of premature death in Western societies. Adherence to healthy nutritional and lifestyle recommendations can play an essential role in the prevention of CVD [1]. Major independent cardiovascular risk factors are cigarette smoking, elevated blood pressure, elevated serum LDL cholesterol, low serum HDL cholesterol, diabetes mellitus and advancing age.
Despite years of national and international recommendations to encourage people to adopt a cardioprotective lifestyle, little is known about knowledge of cardiovascular risk factors in general population. The limited data available have identified the socioeconomic indicator “education” as a strong predictor of cardiovascular risk factor knowledge, with a higher knowledge associated with higher education [2,3]. This socioeconomic polarization could partly explain the fact that a low socioeconomic position has been associated with higher morbidity and mortality of chronic diseases in different Western countries [4-7].
As clearly described in the behaviour change model of Prochaska and Diclement, knowledge is an essential step in developing a more cardioprotective lifestyle, however, minimal research has been performed to evaluate whether knowledge of cardiovascular risk factors is associated with a healthier lifestyle. To evaluate nutritional characteristics of the respondents, dietary pattern analysis was performed. Dietary pattern analysis is based on the concept that foods eaten combined are more important as a reductive methodology characterized by a single food or nutrient analysis. Dietary pattern analysis emerged as an alternative approach to study the relation between nutrition and disease [8]. In this study, the Mediterranean Diet Score (MDS) has been chosen, since higher scores have been associated with a reduction in cardiovascular and total mortality [9]. The aim of this study is to relate knowledge about potential cardiovascular risk factors to lifestyle, using open ended questionnaires.
2. Method
In February 2007, air and terrestrial components of the Belgian army included 33,053 men. After stratification for military rank and age, 5000 men were selected, representative for the total army structure. Stratification was executed in officers, non commissioned officers and soldiers. The selection consisted of 598 officers; 2103 non commissioned officers and 2299 soldiers.
A semiquantitative food frequency questionnaire, including 150 food items, was sent to the subjects. For each food item, the following categories of consumption frequency were possible: never, one to three times a month, once a week, two to four times a week, five to six times a week, once a day and more than once a day. Portion sizes were predefined using familiar measuring devices (teaspoon, glass, cup...). The validity of the food frequency questionnaire was tested on a sample of 100 men representative for the participants [10]. Total intake of fat, fruits, vegetables and salt were divided into tertiles of intake.
A second questionnaire was used to register healthrelated and lifestyle characteristics. This quest-ionnaire was a more general questionnaire about smoking, marital status, main occupation, age, weight, length, and number of children. This questionnaire was used in previous research [11]. Participation was voluntary without incentives. An informed consent was signed by all participants.
Participants were also asked to provide “five possible protective measures against CVD”. This was an open ended questionnaire without predefined choices or answers to capture cardiovascular knowledge. The open answers of the participants were recode in main categories of established and modifiable risk factors (i.e. no yearly medical control for testing serum cholesterol level and systolic/diastolic blood pressure, no smoking, no overweight and physical activity level) and in main categories of dietary risk factors (i.e. eating too much fat, meat, salt, and not consuming sufficient quantity of fruits and vegetables). Non established risk factors were recode as not relevant, except for stress, which was very often mentioned. A level of knowledge score was calculated: one point was given for mentioning each of the five established and modifiable risk factors and one point for mentioning at least one dietary cause. Participants were given the opportunity to provide five responses, so the knowledge scores ranged from 0 to 5. A low level score was defined as a score of 0 or 1, a medium level for a score of 2, and a high level for a score of 3 and more.
For descriptive statistics, frequencies were calculated for individual characteristics versus risk factors. Individual characteristics were age (20 to 29 years, 30 to 39 years, 40 to 49 years, 50 to 59 years); Body Mass Index (BMI) classified according to the World Health Organization in normal weight, 18.5 ≤ BMI < 25.0 kg/m2, overweight, 25.0 ≤ BMI < 30.0 kg/m2 and obesity, BMI ≥ 30.0 kg/m2 [12]; physical activity (stratified in low, moderate and high according to the International Physical Activity Questionnaire) [13]; actual smoking (yes or no); educational level (low for vocational education, moderate for secondary level and high for bachelor and master level); income (low for lowest tertile of yearly gross income of the group, moderate for intermediate tertile of income and high for highest tertile of yearly income). The MDS was computed as described previously9. The possible scores for the MDS range from 0 to 9. The MDS scores were classified in low (range 0 to 3), moderate (range 4 to 6) and high (range 7 to 9).
Chi-square test was used to test the relation between individual characteristics and potential cardiovascular risk factor knowledge. Binary logistic regression adjusted for education was executed to separately estimate the independent effect of age, BMI, physical activity, smoking, income categories and Mediterranean Diet Score on the reported potential risk factors and on the cardiovascular disease knowledge scores. A two-sided level of significance of 0.05 was defined. SPSS 16.0 (SPSS Inc. Chicago, IL) statistics software was used. The Bioethical Committee of the University of Leuven approved the complete research protocol.
3. Results
Table 1 presents the demographic and lifestyle characteristics of the subjects. Out of the 5000 selected men, 1852 (37%) participated to the study. The most prevalent age category was 40 to 49 years and 76% were nonsmokers. About 58% had a BMI ≥ 25.0 kg/m2 and 42.6% had a low level of education. Responders tended to be older (74.3% were older than 40 years of age) compared to non-responders (only 61.4% were older than 40 y) (p < 0.001). Moreover, soldiers were less incline to participate to the study than officers and non-commissioned officers (p < 0.001).
Table 2 presents the answers to the open questions concerning the prevention of cardiovascular disease, recoded in main categories. Lack of physical activity, smoking, eating too much fat and experiencing more stress in daily life were the 4 most cited potential cardiovascular risk. Lack of exercise, smoking and stress were more cited in the highest educational level category than in the lowest, with respectively 88.9%, 60.7%, 34.9% compared with 73.5%, 53.1% and 21.8% of the answers (p < 0.001). The least cited risk factors were low consumption of fruits and vegetables, being overweight and eating too much salt. Being overweight was more cited in
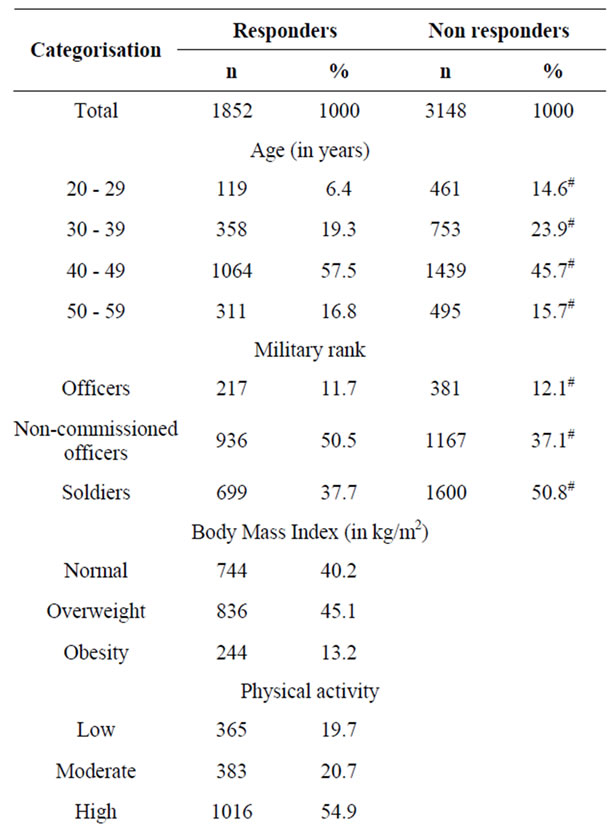
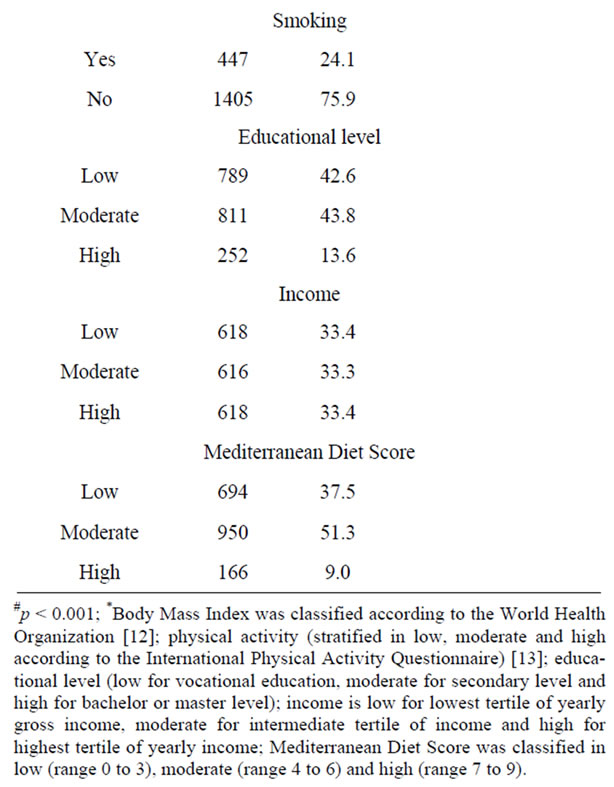
Table 1. Characteristics of the study subjects.
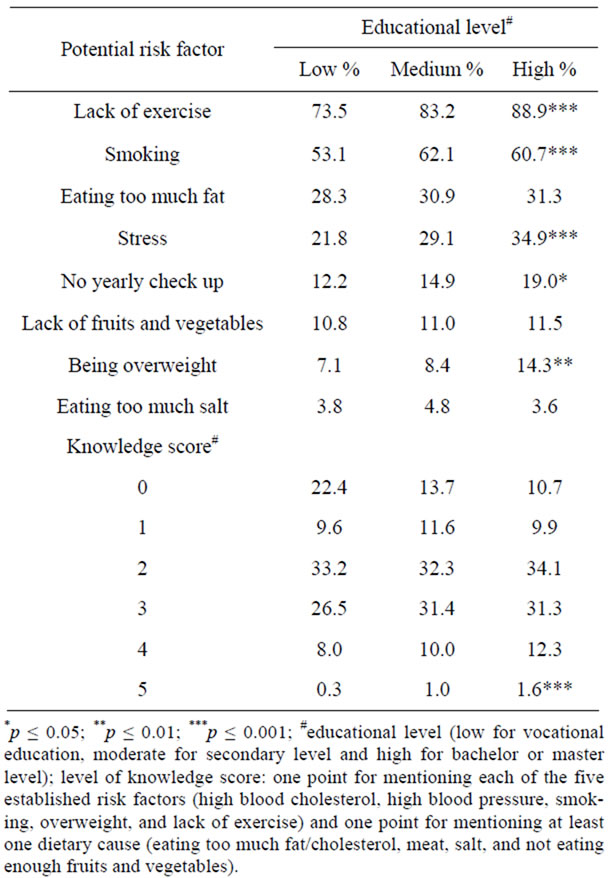
Table 2. Percentages of participants by educational level reporting potential risk factors for cardiovascular disease in the open-ended quest-ionnaires.
the highest educational level, with 14.3% of the answers compared with 7.1% for the lowest educational level (p < 0.01). A high knowledge score of three or more was prevalent for only 34.8% in the low educational category, for 42.4% in the medium category and for 45.2% in the highest educational category (p < 0.001).
Table 3 presents the educational-adjusted odds ratios of the binary logistic regression, executed to estimate the independent effect of age, BMI, physical activity, smoking, income categories and MDS on the knowledge score. Those predictors were not consistently associated with the knowledge scores. However, there was a statistically non-significant increase of the MDS for increasing knowledge score. A high MDS was associated with an odds ratio for higher knowledge of 1.53 (95% CI: 0.98 to 2.38) compared with a low MDS.
Table 4 presents the specific risk factors in function of personal and nutritional characteristics. Reporting overweight, eating too much fat and eating too much salt as risk factor is not associated with respectively the BMI, total fat or salt intake. Reporting lack of physical activity, smoking and low fruit and vegetables intake is associated with respectively a higher physical activity level, nonsmoking status and fruit and vegetables intake. Nonsmokers reported smoking as a risk factor in only 55.9% of the answers, compared with 65.1% for the smokers (p < 0.001). And finally, a high consumption of fruits and vegetables was associated with more frequent reporting of lack of fruit and vegetables intake as risk factor (13.6% versus 7.3%, p < 0.001).
4. Discussion
To our knowledge, this study was the first to relate the level of knowledge of established and modifiable cardiovascular risk factors with dietary pattern analysis: a higher knowledge of potential cardiovascular risk factors was associated with a statistically non-significant increase in MDS.
Secondly, the socioeconomic indicator education played an essential predictive role. The highest level of education was associated with a higher general knowledge of established and modifiable cardiovascular risk factors, which is confirmed by previous research [2,3,14,15].
However, comparing the results of this study with others remains burdensome because of methodological differences. In this study, an open ended questionnaire was used instead of a forced choices questionnaires. The latter increases the chance of responding correctly, which can inflate the prevalent knowledge. Compared with a forced choice questionnaire, an open ended questionnaire will capture a more present cardiovascular knowledge in the memory of the respondent [2].
In a Canadian population, Potvin et al. found that fat, smoking and lack of physical activity were the most cited potential risk factors with 60%, 52% and 41% of the answers [2]. These were also the three most cited factors in our study. This implicates that behavior-related risk factors are cited more frequently than physiologic factors as high blood pressure and blood cholesterol [2]. Two possible explanations are that behavior related risk factors are more easily understood by the public than physiologic factors. Secondly, prevention campaigns often accentuate the essential role of dietary fat, smoking and physical activity in preventing cardiovascular diseases.
Surprisingly, and despite decades of health campaigns, being overweight and consuming less salt were the least spontaneously cited established and modifiable risk factors. The association between overweight and cardiovascular disease is probably less clear to the public, since other risk factors such as lack of physical activity, eating too much fat, high blood pressure and/or high blood cholesterol received more attention in health campaigns. The difficulty with salt is that more than 70% of the daily overconsumption is apparently invisible for the consumers. For instance, bread, cheese, soups, ready to eat cereals and meals are rich in salt. It is very difficult to estimate daily salt consumption and, adding no or less salt during cooking sessions will have an apparent important impact on consumer’s perception of salt intake but a limited impact on total salt consumption.
Experiencing stress was the fourth most cited cardiovascular risk factor, which is a non-established factor as has been confirmed by other research [16]. This must be
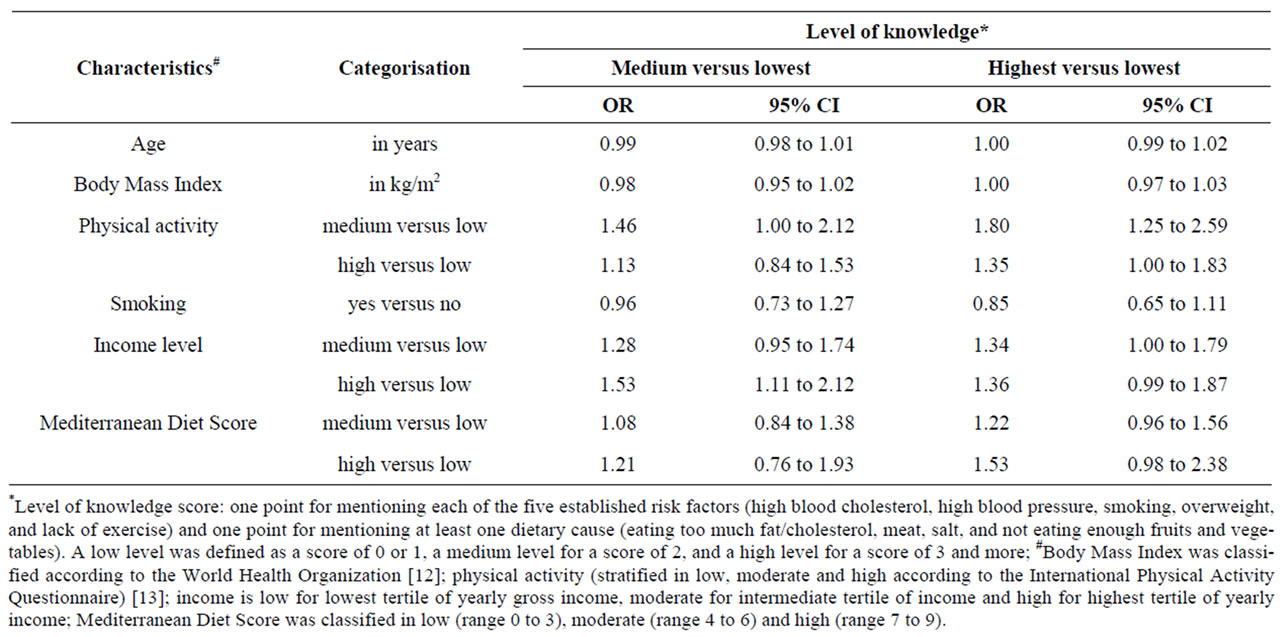
Table 3. Odds ratios adjusted for education for predictors of reporting potential risk factors for cardiovascular disease.
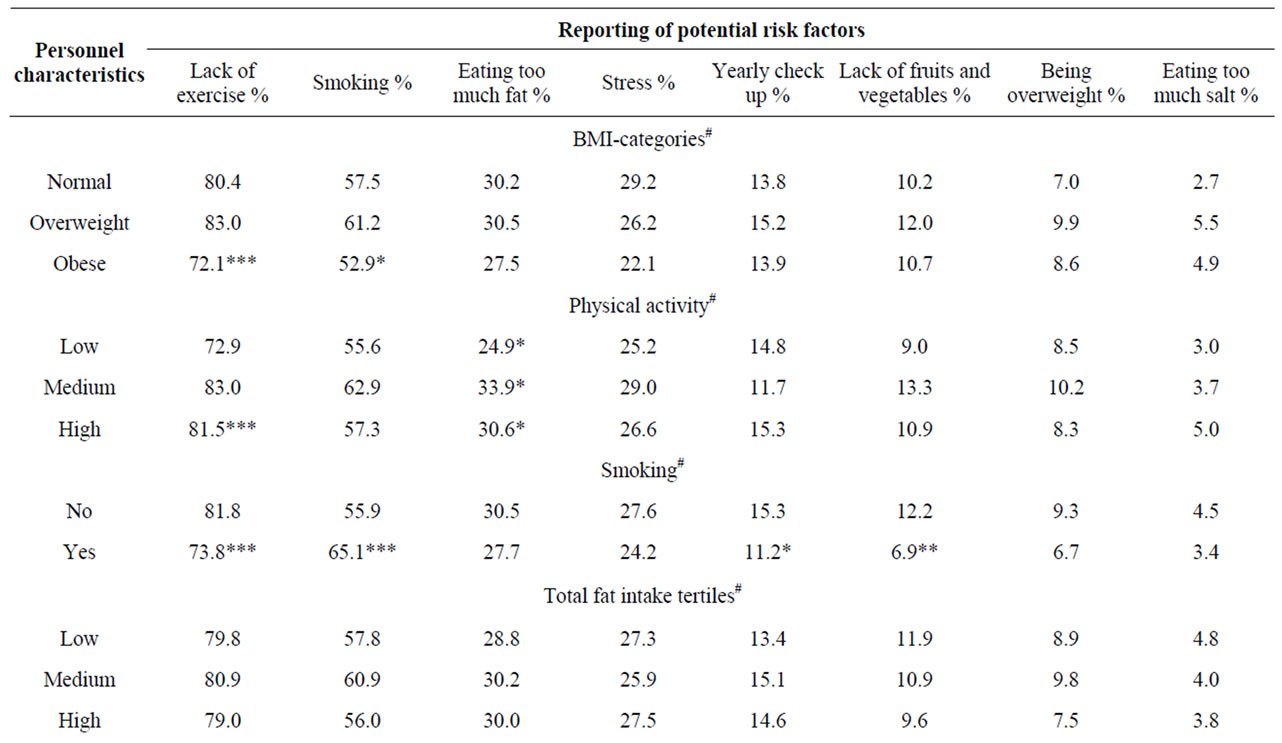
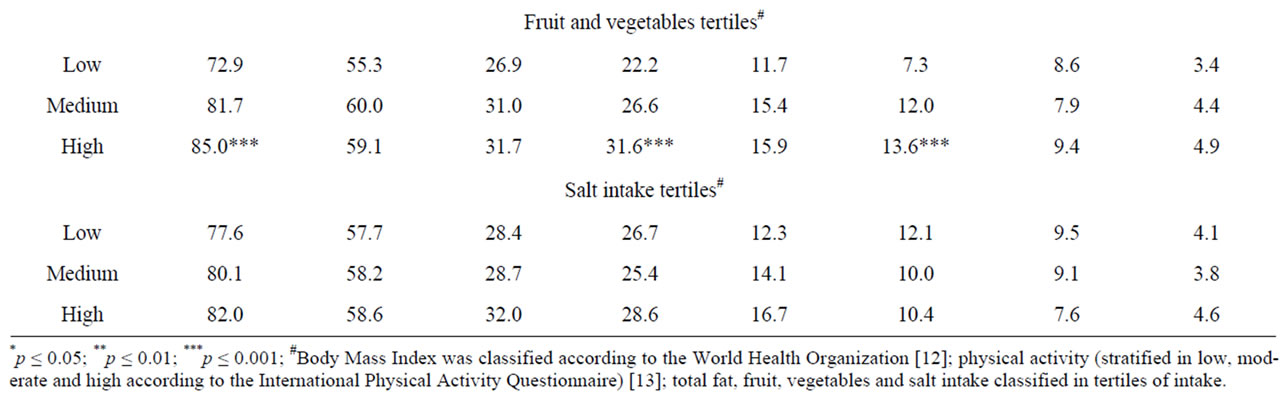
Table 4. Percentages of participants reporting potential risk factors for cardiovascular disease in function of characteristics.
taken into account in developing prevention campaigns, because if an individual believes that stress is an important cause of cardiovascular disease, other protective factors such as more physical activity and lower consumption of saturated fatty acids, both important in reducing the risk of CVD, could be discounted.
The findings of this study confirm that there is a gap between risk factor knowledge and lifestyle. Reporting overweight, eating too much fat and eating too much salt as risk factor was not associated with a more healthy weight, total fat or salt intake. Reporting higher physical activity as cardiovascular protective factor was associated with a higher level of physical activity. Comparably, reporting fruit and vegetables intake as risk factor was associated with a higher consumption of these nutrients. It is however remarkable that smokers are well aware that this addiction can cause CVD, but nevertheless continue to smoke. Thus, risk factor knowledge, an essential step in prevention of CVD, is not systematically associated with a healthier lifestyle.
A military population was selected for this study. This population has the advantage that accurate information about non responders to the mailing, which is usually difficult to obtain in epidemi-ological research, could be obtained from administrative services. Our sample was representative for the socioeconomic level of the Belgian army. However, we believe that due to the different manual and non-manual tasks, occupations and educations present in an army, our sample can be seen as a representative sample for men with an occupation.
Moreover, our nutritional and lifestyle data match with the results of a recent cross-sectional research on a representative Belgian population [17].
In conclusion, a low socioeconomic position as measured by the indicator education was associated with a lower knowledge of established and modifiable cardiovascular risk factors. Risk factor knowledge, an essential step in prevention of CVD, is not systematically associated with a healthier lifestyle. Future research on efficient communication possibilities to members of low socioeconomic positions will be necessary.
REFERENCES
- M. J. Stampfer, F. B. Hu, J. E. Manson, E. Rimm and W. C. Willett, “Primary Prevention of Coronary Heart Disease in Women through Diet and Lifestyle,” New England Journam of Medicine, Vol. 343, 2000, pp. 16-22. doi:10.1056/NEJM200007063430103
- L. Potvin, L. Richard and A. C. Edwards, “Knowledge of Cardiovascular Disease Risk Factors among the Canadian Population: Relationships with Indicators of Socioeconomic Status,” Canadian Medical Association Journal, Vol. 162, No. 9, 2000, pp. S5-S11.
- E. B. Lynch, K. Liu, C. I. Kiefe and P. Greenland, “Cardiovascular Disease Risk Factor Knowledge in Young Adults and 10-Year Change in Risk Factors: The Coronary Artery Risk Development in Young Adults (CARDIA) Study,” American Journal of Epidemiology, Vol. 164, No. 12, 2006, pp. 1171-1179. doi:10.1093/aje/kwj334
- J. J. Feldman, D. M. Makuc, J. C. Kleinman and J. Cornoni-Huntley, “National Trends in Educational Differentials in Mortality,” Amercian Journal of Epidemiology, Vol. 129, No. 5, 1989, pp. 919-933.
- M. Huisman, A. E. Kunst, O. Andersen, M. Bopp, J. K. Borgan, C. Borrell, et al., “Socioeconomic Inequalities in Mortality among Elderly People in 11 European Populations,” Journal of Epidemiology Community Health, Vol. 58, No. 6, 2004, pp. 468-475. doi:10.1136/jech.2003.010496
- M. Rosvall, B. Chaix, J. Lynch, M. Lindstrom and J. Merlo, “Similar Support for Three Different Life Course Socioeconomic Models on Predicting Premature Cardiovascular Mortality and All-Cause Mortality,” BMC Public Health, Vol. 6, 2006, p. 203. doi:10.1186/1471-2458-6-203
- K. Manhem, A. Dotevall, L. Wilhelmsen and A. Rosengren, “Social Gradients in Cardiovascular Risk Factors and Symptoms of Swedish Men and Women: The Goteborg MONICA Study 1995,” European Journal of Cardiovascular Prevention and Rehabilitation, Vol. 7, No. 5, 2000, pp. 359-368.
- M. L. Slattery, “Defining Dietary Consumption: Is the Sum Greater than Its Parts?” American Journal of Clinical Nutrition, Vol. 88, No. 1, 2008, pp. 14-15.
- F. Sofi, F. Cesari, R. Abbate, G. F. Gensini and A. Casini, “Adherence to Mediterranean Diet and Health Status: MetaAnalysis,” British Medical Journal, Vol. 337, No. a1344, 2008. doi:10.1136/bmj.a1344
- P. Mullie, P. Clarys, M. Hulens and G. Vansant, “Reproducibility and Validity of a Semi-Quantitative Food Frequency Questionnaire among Military Men,” Military Medicine, Vol. 174, No. 8, 2009, pp. 852-856.
- P. Autier, J. Creplet, G. Vansant, C. Brohet, N. Paquot, E. Muls, et al., “The Impact of Reimbursement Criteria on the Appropriateness of ‘Statin’ Prescribing,” European Journal of Cardiovascular Prevention and Rehabilitation, Vol. 10, No. 6, 2003, pp. 456-462. doi:10.1097/01.hjr.0000103276.02552.57
- World Health Organisation, Process for a WHO Global Strategy on Diet, Physical Activity and Health, WHA55.23, 2006.
- P. C. Hallal and C. G. Victora, “Reliability and Validity of the International Physical Activity Questionnaire (IPAQ),” Medicine and Science in Sports and Exercise, Vol. 36, No. 3, 2004, p. 556. doi:10.1249/01.MSS.0000117161.66394.07
- S. M. Consoli and E. Bruckert, “Educational Level Has a Major Impact on the Representations of Cholesterol: A Study in 1579 Hypercholesterolemic Patients,” Preventive Medicine, Vol. 38, No. 3, 2004, pp. 323-329. doi:10.1016/j.ypmed.2003.10.009
- K. Momtahan, J. Berkman, J. Sellick, S. A. Kearns and N. Lauzon, “Patients’ Understanding of Cardiac Risk Factors: A Point-Prevalence Study,” Journal of Cardiovascular Nursing, Vol. 19, No. 1, 2004, pp. 13-20.
- E. B. Lynch, K. Liu, C. I. Kiefe and P. Greenland, “Cardiovascular Disease Risk Factor Knowledge in Young Adults and 10-Year Change in Risk Factors: The Coronary Artery Risk Development in Young Adults (CARDIA) Study,” American Journal of Epidemiology, Vol. 164, No. 12, 2006, pp. 1171-1179. doi:10.1093/aje/kwj334
- S. Devriese, I. Huybrechts, M. Moreau and H. Van Oyen, “The Belgian Food Consumption Survey 1―2004. IPH/ EPI Reports N° 2006 - 016―2006,” Epidemiology Unit, Scientific Institute of Public Health, Brussels, 2006.

