International Journal of Otolaryngology and Head & Neck Surgery
Vol.3 No.5(2014), Article
ID:49636,7
pages
DOI:10.4236/ijohns.2014.35040
Ameloblastoma—A Locally Destructive and Invasive Tumour—Review of Literature
Mir Ruquaya*, Vikram Pratap Singh
Sr. Consultant Surgical Oncology, Indraprastha Apollo Hospital, New Delhi, India
Email: *ruquaya.mir@hotmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 4 June 2014; revised 3 July 2014; accepted 2 August 2014
Abstract
The ameloblastoma is the second most common odontogenic tumour [1] . It occurs exclusively in the jaws, with a strong predilection for the posterior region of the mandible. Although benign, the ameloblastoma is a destructive tumour, locally invasive and presents a high rate of recurrence despite adequate surgical removal. A thorough understanding of its clinico-pathological behaviour is essential to avoid recurrence associated with inadequately treated disease. Currently wide resection and immediate reconstruction are the treatment of choice.
Keywords:Ameloblastoma, Reconstruction, Presentation

1. Case Report 1
31-year-old normotensive, non-diabetic, non-smoker with has a proliferative lesion in central lower alveolus since last 16 years. The lesion has been progressively increasing in size and was associated with loosening and displacement of teeth. He also complained about difficulty in chewing and closing his mouth. On examination there was an ulcero-proliferative growth involving lower central segment of mandible up to angle and crossing the midline anteriorly. The tumour was involving the floor of mouth anteriorly and lower gingivo-buccal sulcus with loosening and displacement of lower molar, premolar and canine teeth (Figure 1). There was no cervical lymphadenopathy.
CECT neck/face showed a large lytic expansile mass involving body of mandible, symphysis menti with displacement of teeth. There was widening of mandible (Figure 2, Figure 3). Incisional biopsy from tumour was suggestive of ameloblastoma. Wide local excision of the mandible, floor of mouth was done. Reconstruction was done with fibular osseo-cutaneous microvascular flap. Post operative recovery was uneventfull.
2. Case Report 2
59-year-old female patient presented with swelling of right face for last 15 years which has been progressively increasing in size. There was no trismus. Patient had undergone surgery twice on same side of face for similar lesions 20 years back. She had undergone right segmental mandibulectomy. Her associated problems were subluxation of right elbow, cervical vertebrae and left knee. There was wasting of muscles of right arm but with no neurological deficit. She complained of deafness for last 2 years. Clinical examination showed a large partially compressible lesion involving right parietal region/right cheek and right submandibular region. Right segment of mandible was missing. The lesion was pushing the posterior pharyngeal wall with stretching of pinna and exter-

Figure 1. Picture showing the extent of tumour involving right cheek, temporal region.
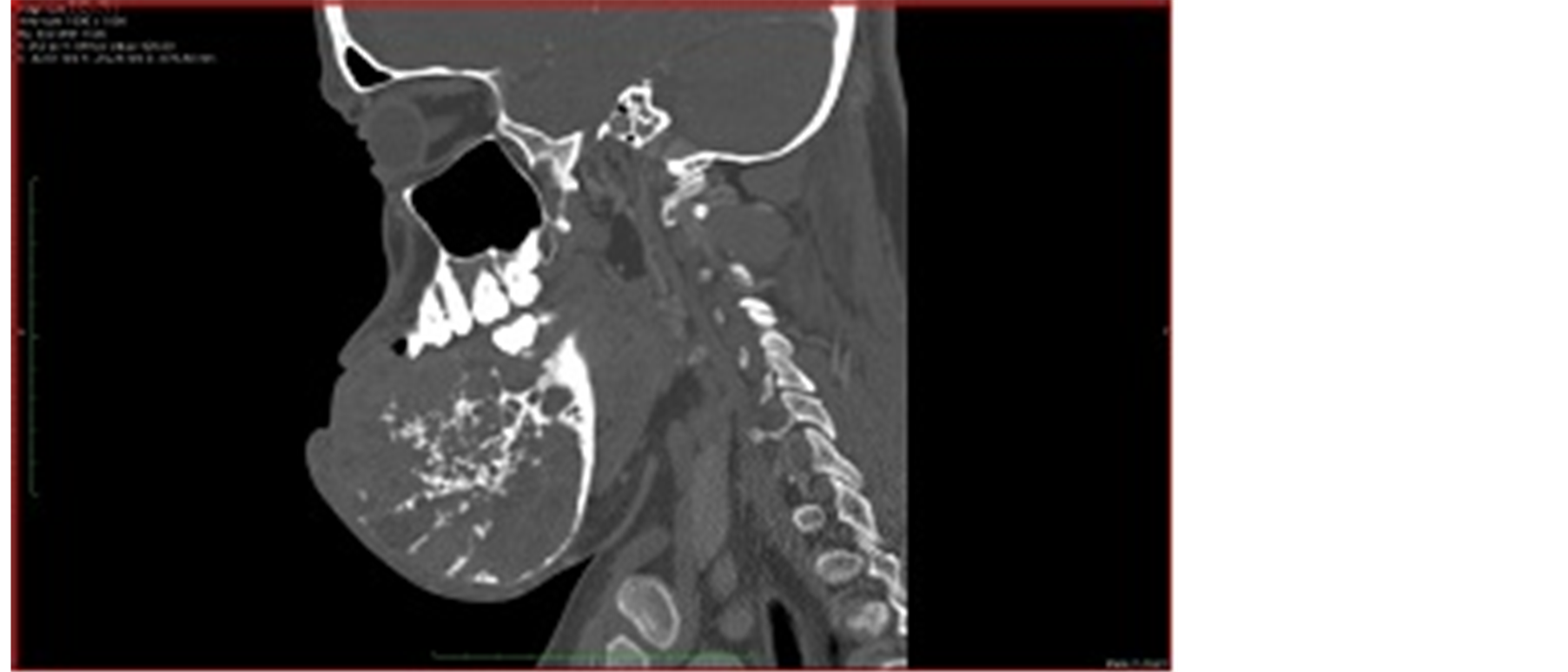
Figure 2. Axial and sagittal of images showing a large expansile osseous mass arising from mandible with associated soft tissue component.

Figure 3. Axial and sagittal of images showing a large expansile osseous mass arising from mandible with associated soft tissue component.
nal auditory canal (Figure 4). CECT face/neck showed mass in right face with erosion of right parietal bone, right zygomatic arch, maxilla, pterygoid plates with compression of external auditory canal. Right eyeball, optic nerve were reported normal (Figure 5, Figure 6). Wide local excision with primary closure was done (Figure 7, Figure 8). Histopathology was reported as ameloblastoma.
3. Discussion
Ameloblastoma is an uncommon tumour of the mandible and maxilla. It is a locally aggressive tumour that, if neglected, can reach an enormous size and cause severe facial disfigurement and functional impairment. It occurs with equal frequency in both sexes and has its peak incidence in the third to fourth decade of life. Overall, 80% of all ameloblastomas occur in the mandible and 20% in the maxilla. According to the 2005 classification of tumours of the World Health Organization, the variants of ameloblastomas are the solid/multicystic, the extra osseous ameloblastoma, the desmoplastic and the unicystic type [1] . Multicystic ameloblastoma is the most common variant, making up 85% of all ameloblastomas. It has a propensity to be more aggressive and is associated with a higher recurrence when compared with the other two forms. Ameloblastomas may be relatively asymptomatic and can be detected incidentally on radiological imaging. When symptoms are present, patients often complain of a slow-growing, painless swelling [2] as in our case report 1. Less commonly, they may present with pain or par aesthesia loose teeth, or malocclusion. Facial deformity, if present, may range from very mild to severe in delayed presentations. They may also be associated with the presence of unerupted teeth, in particular the mandibular third molar. They are believed to arise either from embryonic remnants of the epithelial lining of an odontogenic cyst, dental lamina or enamel organ, stratified squamous epithelium of the oral cavity, or displaced epithelial remnants. Its pathogenesis remains unclear [3] [4] .
Radiological investigations provide a useful aid to diagnosis. However, these findings are not pathognomonic

Figure 4. Clinical photograph showing the extent of lesion.
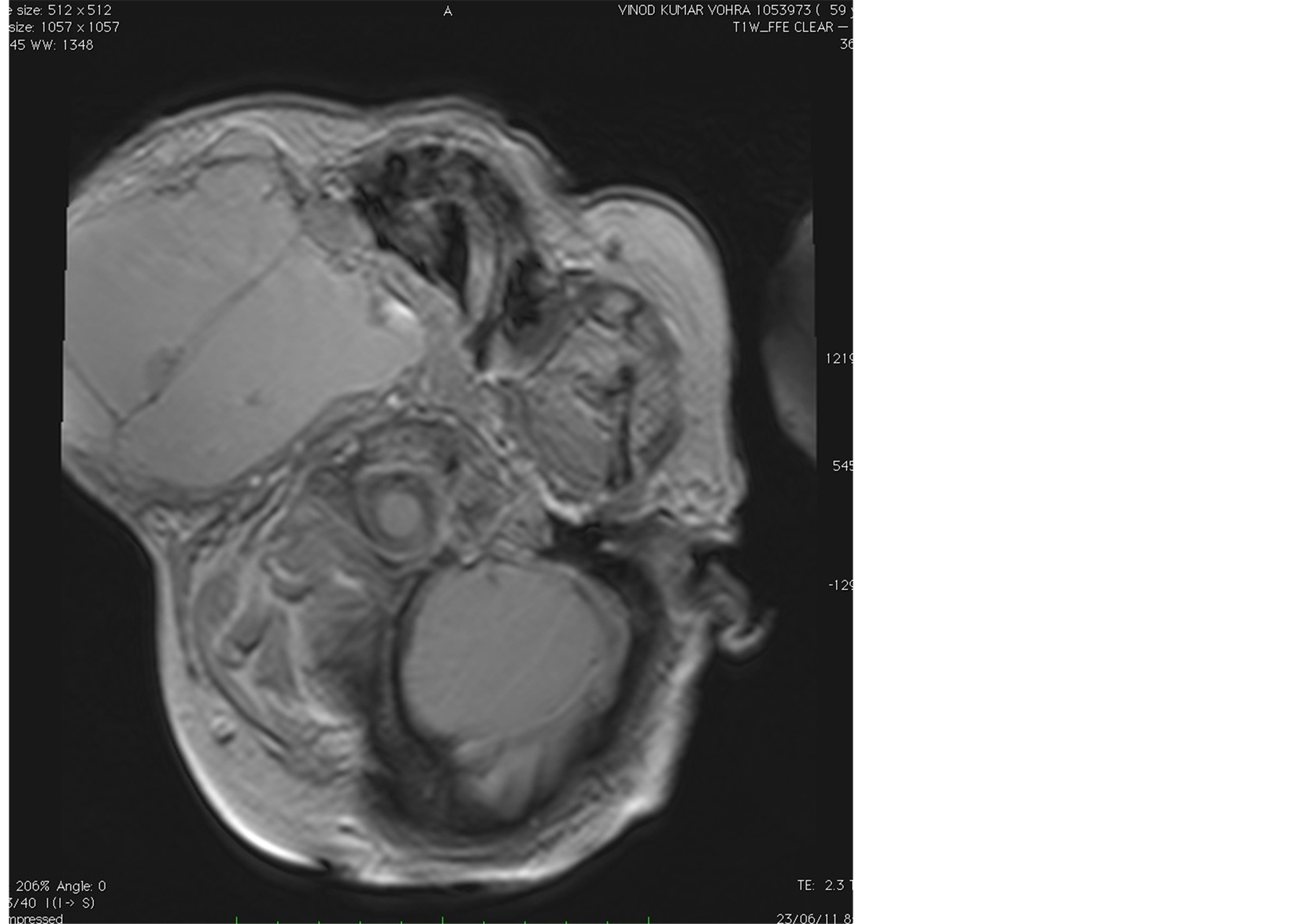
Figure 5. Axial images through skull showing a large cystic lesion in right masticator space with scalloping of temporal and right zygomatic bone.

Figure 6. T2 W sagittal image of cervical spine shows basilar invagination with focal kyphotic deformity at C5-C6 level.

Figure 7. Axial T1 W d T2 W images through skull base reveal deformed cervicovertebral junction. A large cystic mass lesion is also seen in right masticator space.
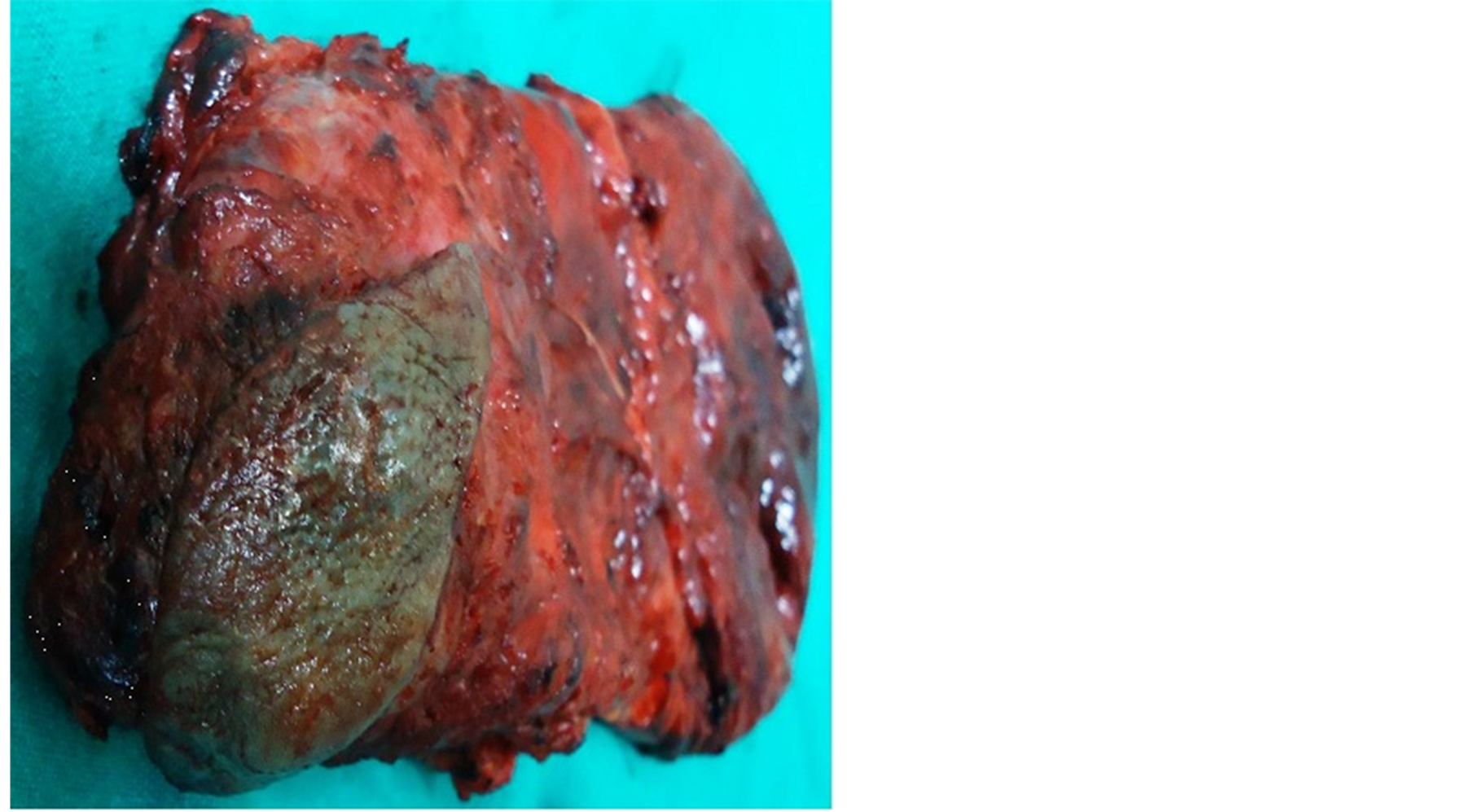
Figure 8. Picture of excised specimen of case report 2.
and must therefore be confirmed with histological examination. The orthopantomogram (OPG) is a useful firstline investigation and may reveal lucency in the bone of varying size and shape associated with scalloped margins and resorption of the roots of involved teeth as in our case report 2.
Occasionally it can be a well-demarcated unilocular lesion, whereas often it presents as multiloculated expansile lucencies with a so called “soap bubble” appearance [5] [6] . Computed tomography (CT) may be useful in the assessment of the extent of the tumour, cortical destruction and extension into the neighbouring soft tissues. Ameloblastoma poses a challenge for all involved not only adequate resection of the tumour but also a functional and aesthetically acceptable reconstruction of the residual defect. Wide resection and immediate reconstruction is currently accepted as the treatment of choice in most cases and are associated with high rate of recurrence if inadequately treated.
They are rarely considered to exhibit metastatic spread. Metastatic ameloblastoma refers to lesions that metastasize despite having the typical benign histology of ameloblastoma in both the primary and metastatic lesions. Ameloblastic carcinoma, on the other hand, refers to lesions that demonstrate histological features of both ameloblastoma and carcinoma [7] [8] .
In contrast to ameloblastoma, ameloblastic carcinoma presents more aggressive clinical features, such as rapid growth, perforation of the cortex, and painful swelling. In most cases, radiographic findings show ill defined radiolucency [9] . However, focal radio opacity may be detected in radiolucent lesions. Ameloblastic carcinoma may metastasize to the regional lymph nodes or lung. In rare cases, brain or multiple bone metastasis have been reported. Patient prognosis is difficult to assign, because of the rarity of well documented follow-up information.
References
- Barnes, L., Everson, J.W., Reichart, P. and Sindransky, D. (Eds.) (2005) Pathology and Genetics of Head and Neck Tumous. WHO Classification of Tumours Series, IARC Press, Lyon.
- Fletcher, C.D.M. (Ed.) (2007) Diagnostic Histopathology of Tumors. 3rd Edition, Churchill Livingstone Elsevier, Philadelphia.
- Thompson, L.D. (2003) Ameloblastoma. Ear, Nose Throat Journal, 82, 19.
- Williams, T. (1992) The Ameloblastoma: A Review of the Literature. Selected Readings in Oral and Maxillofacial Surgery, 2, 1-17.
- Mclvor, J. (1974) The Radiological Features of Ameloblastoma. Clinical Radiology, 25, 237-242. http://dx.doi.org/10.1016/S0009-9260(74)80060-7
- Underhill, T.E., Katz, J.O., Pope, T.L. and Dunlap, C.L. (1992) Radiologic Findings of Disease Involving the Maxilla and Mandible. American Journal of Roentgenology, 159, 345-350. http://dx.doi.org/10.2214/ajr.159.2.1632353
- Slootweg, P.J. and Muller, H. (1984) Malignant Ameloblastoma or Ameloblastic Carcinoma. Oral Surgery, Oral Medicine, Oral Pathology, 57, 168-176. http://dx.doi.org/10.1016/0030-4220(84)90207-X
- Elzay, R.P. (1982) Primary Intraosseous Carcinoma of the Jaws. Review and Update of Odontogenic Carcinomas. Oral Surgery, Oral Medicine, Oral Pathology, 54, 299-303. http://dx.doi.org/10.1016/0030-4220(82)90099-8
- Akrish, S., Buchner, A., Shoshani, Y., Vered, M. and Dayan, D. (2007) Ameloblastic Carcinoma: Report of a New Case, Literature Review, and Comparison to Ameloblastoma. Journal of Oral and Maxillofacial Surgery, 65, 777-783. http://dx.doi.org/10.1016/j.joms.2005.11.116
NOTES

*Corresponding author.

