International Journal of Otolaryngology and Head & Neck Surgery
Vol.3 No.3(2014), Article ID:45691,5 pages DOI:10.4236/ijohns.2014.33023
Primary Oropharyngeal Tuberculosis—A Differential Diagnosis to Malignancy
Swati D. Lambor, Dheeraj V. Lambor*, Sai Spoorthi R. Nayak, Archan D. Naik
Department of Otorhinolaryngology and Head & Neck Surgery, Goa Medical College, Goa, India
Email: *drdheerajlambor@rediffmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 23 February 2014; revised 22 March 2014; accepted 21 April 2014
ABSTRACT
Tuberculosis is a communicable disease manifesting as pulmonary and extra pulmonary infection. Extra pulmonary tuberculosis involving pharynx is usually secondary to active pulmonary tuberculosis. Primary oropharyngeal tuberculosis is rare and has been reported in association with immunocompromised states like HIV-AIDS and chronic alcoholism. It has very unusual clinical presentation and sometimes mimics malignancy. We report herewith two cases of primary oropharyngeal tuberculosis, clinically mimicking a malignancy, in immunocompetent adult patients. A high index of suspicion is required to diagnose pharyngeal tuberculosis in patients presenting with ulceroproliferative mass in oropharynx. Histopathological findings of characteristic tuberculous granuloma are confirmatory. Anti-tuberculous therapy gives excellent results within two months of commencing the treatment.
Keywords:Tuberculosis, Pharyngeal, Tonsil, Oropharynx

1. Introduction
Tuberculosis (TB) is a specific infectious disease caused by Mycobacterium tuberculosis and it continues to be a worldwide public health problem responsible for high mortality even today. The disease primarily involves lungs and various extrapulmonary sites, viz. lymph nodes, pleura, genitourinary tract, bones and joints, central nervous system and abdomen. Pharyngeal tuberculosis is usually secondary to pulmonary tuberculosis. Primary oral and oropharyngeal tuberculosis in absence of pulmonary focus is a rare event and accounts for 0.05% - 5% of total tuberculosis cases [1] . Extensive search of literature revealed that tonsil is the commonest subsite of oropharynx involved in the primary oropharyngeal TB followed by oropharyngeal wall and palate.
We report herewith two cases of oropharyngeal TB without pulmonary focus. The aim of this report is to create awareness in the medical fraternity about the existence of primary oropharyngeal tuberculosis and consider it as one of the differential diagnosis for ulceroproliferative lesion of the oropharynx.
2. Case 1
A 65-year-old man, chronic smoker, presented to our outpatient with history of right-sided throat pain radiating to right ear and dysphagia for one year. He also had muffled voice, nasal regurgitation and foreign body sensation on right side of throat since four months. He had a history of decreased appetite and weight loss. There was no history of fever, cough, haemoptysis or contact with Koch’s. On clinical examination, he was thinly built weighing 27 kg, anaemic, and had grade two clubbing. There was a single right level IIb lymph node measuring 1 × 1 cm, which was firm, mobile and nontender. Oropharyngeal examination revealed an ulceroproliferative growth with everted edges extending from lower pole of right tonsil to tonsillo-lingual sulcus, continuing over right lateral pharyngeal wall and vallecula. Larynx was normal on indirect laryngoscopy.
Fine needle aspiration cytology (FNAC) of lymph node showed chronic inflammatory infiltrate. Haemogram revealed features of iron-deficiency anaemia. He was nonreactive for HIV-ELISA and Hepatitis B (HBsAg). His chest X-ray was normal. Clinically he was diagnosed as malignancy of the oropharynx and wedge biopsy was taken under general anaesthesia. To our surprise, histopathological examination revealed epithelioid cells with Langhans Giant cells and caseation necrosis. Thus the diagnosis of oropharyngeal TB was established. Sputum examination with Ziehl-Neelsen stain for acid fast bacillus (AFB) was negative. He was started on Category I Directly Observed Treatment Shortcourse (DOTS). After two months of treatment, the oropharyngeal mass completely regressed and the patient was symptomatically relieved. He completed the treatment and is well.
3. Case 2
A 31-year-old lady, presented to our outpatient with history of left sided throat pain and foreign body sensation for three years. She also noticed bleeding from throat on manipulating with the fingers while brushing her teeth. She was treated by several doctors for chronic pharyngitis. There was no history of fever, weight loss, cough, haemoptysis or hoarseness. On clinical examination she had an irregular growth involving left tonsil extending superiorly over uvula and inferiorly over lateral pharyngeal and posterior pharyngeal walls (Figure 1), vallecula, left pharyngoepiglottic fold and epiglottis (Figure 2). The surface of the growth showed pale granulations. On palpation, it was firm in consistency and bled to touch. She had enlarged bilateral jugulodigastric lymph nodes measuring 1.5 × 1.5 cm each. Hence clinical diagnosis of oropharyngeal malignancy was suspected. A punch biopsy of the growth was performed under local anaesthaesia. The histopathology revealed typical features of tuberculous granuloma. Her sputum examination for AFB was negative and chest X-ray was normal. She was
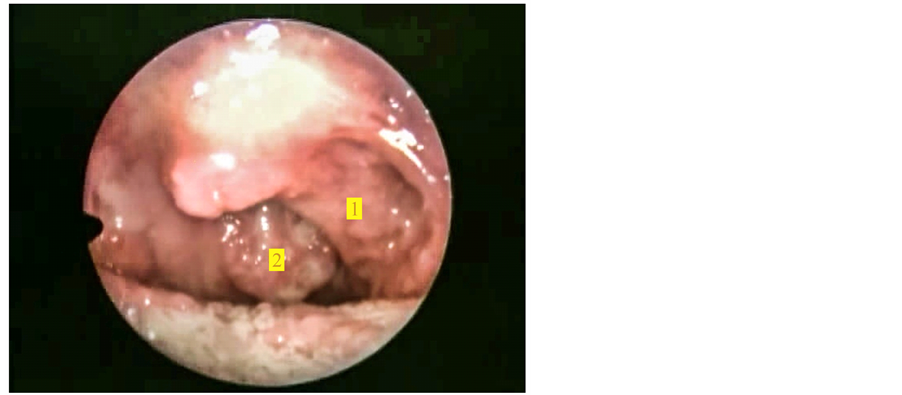
Figure 1. Showing pale, proliferative growth involving (1) Tonsillar fossa extending over uvula, (2) Posterior pharyngeal wall.
non reactive for HIV-ELISA and Hepatitis B. Hence diagnosis of primary oropharyngeal TB was established and she was started on Category I DOTS. After two months of intensive phase of treatment, her growth regressed (Figure 3) and symptoms were relieved.
4. Discussion
There have been changing trends noted in the epidemiology of tuberculosis and several unusual presentations of extra pulmonary tuberculosis have been reported. The upper respiratory tract is generally resistant to infection by Mycobacterium tuberculosis due to the protection offered by presence of salivary enzymes, tissue enzymes, oral saprophytes, cleansing action of saliva and thick epithelial lining [2] . Any break or loss of this protective mechanism due to trauma, inflammatory conditions, tooth extraction or poor oral hygiene may provide a route of entry for the mycobacterium [3] . However the organism can invade intact mucosal barriers by endocytosis within mucosal lymphoepithelial sites like oropharyngeal and nasopharyngeal tonsils and peyer’s patches [4] .
Primary oropharyngeal involvement without pulmonary infection, though uncommon, is a known entity. Pharyngeal TB usually occurs in children which causes an asymptomatic primary focus in pharynx with cervical
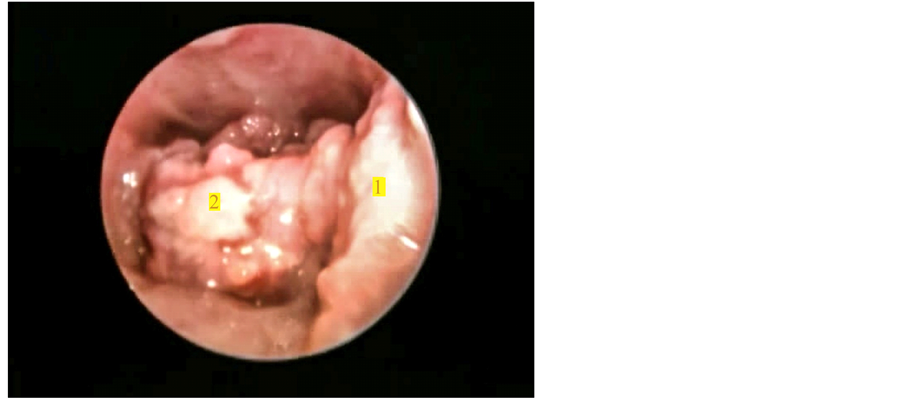
Figure 2. Showing extension of growth inferiorly over (1) Lateral pharyngeal wall, (2) Vallecula and epiglottis.

Figure 3. Showing regression of growth after two months of intensive phase of DOTS.
lymphadenopathy [5] [6] . Several cases of paediatric primary oropharyngeal tuberculosis have been reported in literature [7] [8] [9] . However our search of literature has revealed that adult cases of primary oropharyngeal TB are more in number than paediatric, even in the absence of immunocompromised states like HIV and chronic alcoholism [2] [10] [11] [12] .
Patients usually present with sore throat, fever, malaise, decreased appetite, weight loss, and odynophagia, tonsillar enlargement with surface ulceration or ulceroproliferative growth mimicking a malignancy. Therefore a high index of suspicion is required to diagnose primary oropharyngeal tuberculosis. The other important differential diagnoses include aphthous ulcers, traumatic ulcers, haematological disorders, actinomycosis, and other granulomatous disorders. The final diagnosis of oropharyngeal TB is established with histopathological features of caseation necrosis, Langhans giant cells and epithelioid cells. However in initial stages when caseation is absent, the hard tubercle may be difficult to differentiate from other granulomatous lesions like sarcoidosis, syphilis, leprosy or granulomatous response to foreign bodies, lipids and certain fungi. If the diagnosis of primary oropharyngeal TB is correct, then patient will respond to antiTB therapy within two months of commencing the treatment.
In our report both the patients were adults and they were immunocompetent. Also both presented with a proliferative mass mimicking a malignancy. Neither of them had pulmonary tuberculosis. The mass regressed completely within two months of receiving Category I DOTS.
5. Conclusion
So we conclude herewith that any patient presenting with ulceroproliferative lesion of the oropharynx should be subjected for histopathological examination to rule out malignancy and a differential diagnosis of tuberculosis should be kept in mind.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Mignogna, M.D., Muzio, L.L., Flavia, G., Ruoppo, E., Sammartino, G., Zarrelli, C., et al. (2000) Oral Tuberculosis: A Clinical Evaluation of 42 Cases. Oral Diseases, 6, 25-30. http://dx.doi.org/10.1111/j.1601-0825.2000.tb00317.x
- Dadgarnia, M.H., Baradaranfar, M.H., Yazdani, N. and Kouhi, A. (2008) Oropharyngeal Tuberculosis: An Unusual Presentation. Acta Medica Iranica, 46, 521-524.
- Iype, E.M., Ramdas, K., Pandey, M., Jayasree, K., Thomas, G., Sebastian, P., et al. (2001) Primary Tuberculosis of Tongue: Report of Three Cases. British Journal of Oral and Maxillofacial Surgery, 39, 402-403. http://dx.doi.org/10.1054/bjom.2000.0663
- Gupta, K.B., Yadav, S.P.S., Sarita and Manchanda, M. (2005) Primary Pharyngeal Tuberculosis. Lung India, 22, 127- 129.
- Gupta, K.B., Tandon, S., Jaswal, T.S. and Singh, S. (2001) Tuberculosis of Tonsil with Unusual Presentation. Indian Journal of Tuberculosis, 48, 223-224.
- Madhuri, Mohan, C. and Sharma, M.L. (2002) Posterior Oro-Pharyngeal Wall Tuberculosis. Indian Journal of Otolaryngology and Head & Neck Surgery, 54, 152-153.
- Ghatak, S., Jana, T., Bandopadhyaya, S. and Biswas, S.K. (2010) Primary Oropharyngeal Tuberculosis Causing Destruction of Uvula—A Rare Presentation. International Journal of Pediatric Otorhinolaryngology, 5, 91-92. http://dx.doi.org/10.1016/j.pedex.2009.04.001
- Prasad, P. and Bharadwaj, M. (2012) Primary Tuberculosis of Tonsils: A Case Report. Case Reports in Medicine, 2012, 120382. http://dx.doi.org/10.1155/2012/120382
- Chavolla, R., Dolci, G.F., Hernandez, J.F.M., Ysunza, A., Cuevas, B., Lazos, M., et al. (2006) Primary Tuberculosis of the Tonsil. International Journal of Pediatric Otorhinolaryngology Extra, 1, 150-153. http://dx.doi.org/10.1016/j.pedex.2006.03.006
- Kant, S. and Verma, S.K. (2008) Sanjay. Isolated Tonsil Tuberculosis. Lung India, 25, 163-164. http://dx.doi.org/10.4103/0970-2113.45284
- Sood, A.S., Bharadwaj, B. and Gill, J.S. (2011) Primary Tuberculosis of the Tonsil. Nepalese Journal of ENT Head and Neck Surgery, 2, 17-18.
NOTES

*Corresponding author.

