Surgical Science
Vol.5 No.3(2014), Article ID:43775,6 pages DOI:10.4236/ss.2014.53017
Clinically Relevant Assessment of the Variability of Glycemic Response and Its Affect on Surgical Site Infection Rates?
Ali Mahmood1,2,3,4,5*, Khaled I. El-Badawi1,5, Theodor Asgeirsson1,3,5, Vinay Gajula#, Anthony J. Senagore4,5
1Grand Rapids Medical Education and Research Center, Grand Rapids, USA
2Baylor College of Medicine, Houston, USA
3University of Texas Medical School at Houston, Houston, USA
4Spectrum Health Department of Research, Grand Rapids, USA
5Department of Surgery, Michigan State University, East Lansing, USA
Email: *strikermd@hotmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 20 January 2014; revised 18 February 2014; accepted 26 February 2014
Abstract
Purpose: Despite growing interest in perioperative glycemic control, little data exist defining the optimal value(s) to use to define appropriate glycemic management and the impact on the incidence of surgical site infection (SSI). The aim of this study was to assess variation in glycemic response and risk of SSI and hospital stay as defined by the maximum, minimum, and area under the curve for perioperative glucose in patients undergoing colectomy. We specifically used standard of care obtained glucose levels to reflect limitations of observations typically used to assess quality of care. Methods: All patients undergoing colectomy from 7/2007 to 6/2008 were assessed for the maximum and minimum levels of standard of care glucose levels, as well as area under the curve (AUC) for elevated glucose perioperatively. These were assessed for patients with and without SSI (SSI vs nSSI). Results: 183 consecutive patients were evaluated (22 diabetics). The incidence of SSI for the entire population was 17/183 (9.3%) without significant difference between the groups with respect to mean blood glucose level (SSI-136; nSSI-136). However, the SSI group had a higher maximum glucose level (SSI-194; nSSI 162; p < 0.05) and a lower minimum glucose level (SSI-100; nSSI 117; p < 0.05). Using AUCs for elevated glucose, there was no significant difference in the percentage of SSI patients with glucose > 110 mg/dl (SSI-59%; nSSI-62%) or glucose > 150 mg/dl (SSI 6%; nSSI 18%). Conclusions: The data demonstrate that patients with SSI have wider fluctuations inglycemic response compared to non-SSI when standard of care serum glucose levels was reviewed. Therefore, quality program monitoring of glucose impact on SSI should focus on both maximum and minimum levels during the perioperative period to better define process improvement in colectomy patients.
Keywords:Perioperative Glycemic; Glycemic Response Affect; Glucose Levels

1. Introduction
Perioperative glucose control remains a controversial topic in the medical community, primarily due to the tension between possible benefits with tight glycemic and the possible risk of significant hypoglycemia and increased mortality risk. The implementation of an aggressive glycemic management program requires fastidiousness to a level that requires significant resource consumption.
The historical reliance upon an insulin sliding scale was challenged by Gale et al., arguing that this reactive corrective index did not adequately maintain glycemic control in the aged trauma population where non-survivors had higher average glucose levels compared to survivors [1] . A large randomized trial conducted by Van Den Berghe et al. in 2001 demonstrated that stringent glycemic control effectively reduced mortality with an absolute reduction of nearly 4% in a 1548 patient cohort [2] . The results appeared most promising in the critical care population, where mortality was reduced by close to 50%, although benefit was limited to patients treated greater than 5 days in the surgical intensive care unit (SICU). Trauma literature has also alluded to that fact that poor glycemic control increases the propensity for morbidity and mortality [3] -[5] . Paradoxically, Finney et al. evaluated an Intensive Care Unit (ICU) population, and concluded that increased insulin levels contributed to a greater mortality [6] . They discovered that the prevailing blood glucose levels were less influential on outcome compared to the amount of insulin dispensed. This hypothesis was further supported by Ali et al. where increased glucose variability contributed to a greater mortality, especially in the septic patient population [7] . There are little data regarding glycemic response or the impact of either aggressive glucose control or insulin dosing in a colectomy population. In addition, the limited data have relied in most cases on identifying an at risk population based upon either the highest single glucose level during the postoperative period which may not clearly define the magnitude of relative insulin resistance to surgical stress.
The purpose of this study was to assess the impact of glucose response on surgical site infection (SSI) and length of stay (LOS) following colectomy using standard of care glucose levels. This represents a realistic, administrative data set for quality programs to monitor.
2. Methods
Following approval from our institutional review board (IRB) we retrospectively evaluated a consecutive group of patients undergoing elective colon resection from July 2007 to June 2008, Patients were allocated to one of two groups based upon the presence or absence of SSI (SSI vs nSSI). The preadmission status of diabetes was recorded. The daily maximum and minimum plasma glucose values were assessed for each patient using standard of care levels available in the medical record. We subsequently calculated the area under the curve (AUC) for glucose response. Data was collected regarding LOS.
Patients with a blood glucose level greater than 130 mg/dL, were given insulin based upon an institutional policy that was implemented prior to the study start time. The method of insulin administration was using a “basalbolus” regimen with regular insulin (Table 1). In the established diabetic population, the patients’ blood glucose levels were concurrently managed with a sliding scale in the immediate post operative period, however they were rapidly transitioned back to their native regimen. These management schema were considered standard of care and not specifically controlled as part of this project.
SSIs were identified as any incision that yielded purulence, appeared erythematous, or warranted opening or antibiotics (based upon 30 day follow-up as per our standard NSQIP evaluation process). The length of stay was defined by number of nights spent in the hospital. Statistical analysis consisted of Student’s t test and Chi Square where appropriate with statistical significance set at p < 0.05.
Table 1. Glucose values with the respective corrective insulin regimen.
3. Results
There were 183 colectomy patients available for study of whom 22 (12.0%) were Type II diabetics (10 insulin dependent). The overall incidence of SSI for the entire population was 17 (9.3%). The incidence of patients returning to the emergency room with a SSI was 58.8% (10/17) with 47% (8/17) being readmitted to adequately manage the surgical site infection. The average length of stay for patients with SSI increased to 16.3 days (total days in the hospital), compared to the 3.96 days for the patient population that did not develop a SSI.
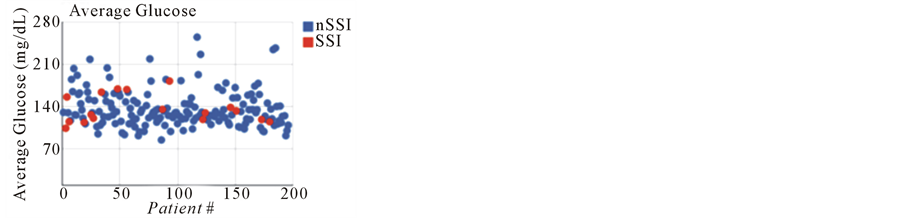
The SSI and nSSI groups were compared for mean daily glucose, maximum daily glucose, and minimum daily glucose levels (Figures 1 and 2). Interestingly, the mean blood glucose levels in the SSI group and nSSI group were identical at 136 mg/dl. The SSI cohort did have a higher maximum blood glucose level reported, 194, compared to the nSSI group, 162 (p < 0.05). However, the SSI group also had a lower average minimum blood glucose than the nSSI, 100 mg/dL and 117 respectively (p < 0.05). The mean glucose values were plotted and the from the values was calculated. There was not a significant difference in the percentage of patients with an SSI using area under the curve (AUC) for glucose levels either >110 mg/dl (SSI 59%; nSSI 62%) or >150 mg/dl (SSI 6%; nSSI 18%) (Figure 2). The length of stay for SSI was 10.4 days, compared to the markedly lower stay for nSSI, 4.5 days.
4. Discussion
Recommendations for routine resuscitation with pharmacologic doses of corticosteroids were subsequently refuted by solid prospective randomized studies and literature reviews [8] [9] . Escalating oxygen to supranormal levels in ARDS patients proved to worsen lung toxicity and outcome, only to give way to reduced tidal volumes as a result of evidence based analysis [10] -[12] . Finally, routine use of perioperative beta blockade for abdominal surgery in drug naïve patients proved to have minimal cardiac benefit while significantly increasing sepsis risk and mortality [13] -[16] .
The topic of hyperglycemia management has gained significance primarily based upon studies from cardiothoracic surgical management. The cardiac surgery population has been the best evaluated and has consistently shown benefit from aggressive glycemic control. The majority of benefit in the cardiovascular surgery population has been a lower rate of sternal wound dehiscence in diabetic patients with more stringent glycemic control [17] [18] . Early administration of glucose following ischemic brain injury to curb hyperglycemia has shown some mortality benefit [19] .
Similar beneficial data from other surgical populations has not been widely available. Although several studies suggested morbidity and mortality benefit for stringent glycemic control of hyperglycemia, these studies primarily evaluated maximum glucose values, or average glucose values. There is more recent data that suggests that despite some mortality benefit with prevention of excessive hyperglycemia, increased variability of insulin requirements may be associated with dramatically disparate morbidity and mortality [20] . This finding was further supported by Krinsley et al., where data from 3252 ICU patients reinforced the additional adverse mortality risk associated with glycemic variability. Tight glycemic control has the potential for clinically significant hypoglycemia which has been associated with a much higher mortality rate in the critical care population (55.9% vs. 39.5%) [21] . In the pediatric population, variability of glucose has also been positively correlated with increased mortality and length of stay [22] .
Our data confirms the lack of absolute adverse effects when utilizing the average glucose level for perioperative colectomy patients for risk of SSI. Interestingly, analysis of hyperglycemia with the AUC methodology
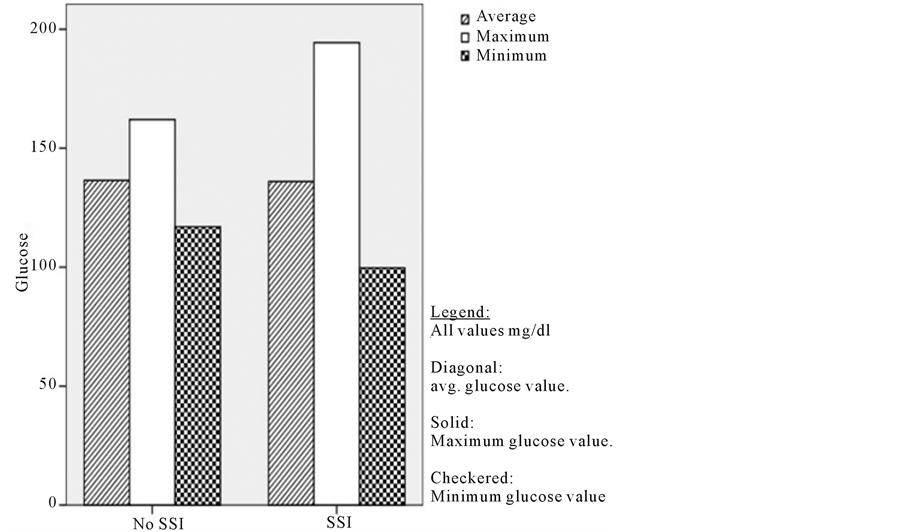
Figure 1. Bar graph depicting SSI vs. nSSI with mean, minimum and maximum values of glucose.
 (a)
(a)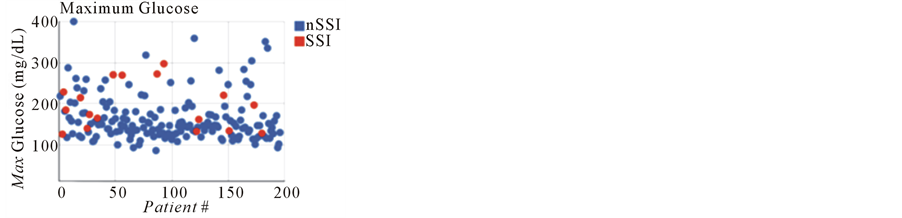 (b)
(b) (c)
(c)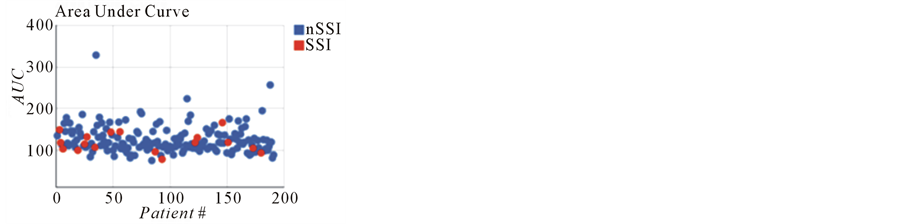 (d)
(d)
Figure 2. Scatter plot graphs depicting average glucose values, minimum and maximum glucose values, along with Area under the curve values.
demonstrated that the there was no significant difference in the values for the two groups of patients with cutoffs of either >110 mg/dl or >150 mg/dl. However, the SSI group clearly demonstrated much greater variability in glycemic ranges (higher highs and lower lows) during the perioperative period compared to the nSSI group. This work is the first demonstration of the negative impact of the lowest glucose level in association with SSI risk. Therefore, our work suggests that reporting both the highest and lowest standard of care perioperative glucose levels during the post-colectomy recovery period may represent a superior outcome measure set for glycemic management for SSI. This reporting structure would simultaneously identify issues related to poor glycemic management as manifested by periods of hypoglycemia.
Although the perils of persistent significant hyperglycemia has been well documented in the diabetic patient stringent control may not provide the same benefit to all patient populations, especially the colectomy population. It is imperative to comprehend that stringent control of blood glucose levels are also inherently associated with the risk of adverse effects. The cost of monitoring, including physician and nursing time, are increased with glycemic monitoring, particularly with the threat of hypoglycemic attacks. While there is little data outlining the exact fiscal expenditure on aggressive glycemic control in the hospital, several studies have reported significant savings with simple patient self-titrated control, circumventing frequent iatrogenic intervention [23] [24] .
Implementation of a broader enhanced recovery protocol and laparoscopic techniques focused on mitigation of the surgical physiologic insult may provide for a better outcome for the colectomy population. There is also some data to suggest that administration of oral carbohdydate solutions in closer proximity to the surgical procedure may further reduce perioperative insulin resistance. Returning diabetic patients to their home regimen of hyperglycemic medication, whether it is oral or subcutaneous, also fosters a faster return to euglycemia. The benefits of an earlier return to enteral nutritional intake leading to a faster return to normoglycemiahave been well documented [2] . This system-based approach may actually provide better outcomes with respect to the rate of SSI than either the current SCIP or glycemic measures.
The current study is limited by the retrospective method of analysis of standard of care glucose measurements which precluded utilization of a rigorous application of the same aggressive methods of glycemic control despite access to the system wide clinical protocol. Our glycemic target and method of treatment may be too aggressive and the rate of hypoglycemia may have adversely affected our outcomes. Alternatively, we were not able to evaluate the impact of hypoglycemic rescue therapy on SSI rates. The selection of timing for glucose measurements was determined by treating surgeon and therefore specific glycemic response curves could not be calculated. However, the use of daily glucose levels as applied in this study are similar to prior work attempting to correlate the impact of glucose levels on SSI and our work raises concerns regarding the validity of single measurement glucose data as a quality measure. Importantly, this work suggests that reporting of both extremes of glucose levels may offer additional risk information for both SSI and the glycemic management program.
In conclusion, our data suggests that assessment of the variability of glycemic response, by monitoring both the highest and lowest perioperative glucose levels, may be a better monitoring measure than either maximal or mean glucose levels. Future studies should seek to define non-insulin based methods of impacting glycemic response and the appropriate targets for glycemic management to reduce the impact of hypoglycemia. Clearer identification of outcomes based process measures which are more highly correlated with reduced SSI and overall enhanced recovery should be achieved to avoid risk of unsuspected harm for our patients.
Acknowledgements
The authors thank Pam Grady, for her assistance in data gathering, and Meredith Vanharn, for her assistance with the statistical analysis.
References
- Gale, S.C., Sicoutris, C., Reilly, P.M., et al. (2007) Poor Glycemic Control Is Associated with Increased Mortality in Critically Ill Trauma Patients. The American Surgeon, 73, 454-460.
- Van den Berghe, G., Wouters, P.J., Bouillon, R., et al. (2003) Outcome Benefit of Intensive Insulin Therapy in the Critically Ill: Insulin Dose versus Glycemic Control. Critical Care Medicine, 31, 359-366. http://dx.doi.org/10.1097/01.CCM.0000045568.12881.10
- Cochran, A., Scaife, E.R., Hansen, K.W., et al. (2003) Hyperglycemia and Outcomes from Pediatric Traumatic Brain Injury. Journal of Trauma, 55, 1035-1038. http://dx.doi.org/10.1097/01.TA.0000031175.96507.48
- Yendamuri, S., Fulda, G.J., Tinkoff, G.H., et al. (2003) Admission Hyperglycemia as a Prognostic Indicator in Trauma. Journal of Trauma, 55, 33-38. http://dx.doi.org/10.1097/01.TA.0000074434.39928.72
- Sung, J., Bochicchio, G.V., Joshi, M., et al. (2005) Admission Hyperglycemia Is Predictive of Outcome in Critically Ill Trauma Patients. Journal of Trauma, 59, 80-83. http://dx.doi.org/10.1097/01.TA.0000171452.96585.84
- Finney, S.J., Zekveld, C., Elia, A., et al. (2003) Glucose Control and Mortality in Critically Ill Patients. JAMA, 290, 2041-2048. http://dx.doi.org/10.1001/jama.290.15.2041
- Ali, N.A., O’Brien, J.M. and Dungan, K. (2008) Glucose Variability and Mortality in Patients with Sepsis. Critical Care Medicine, 36, 2316-2321. http://dx.doi.org/10.1097/CCM.0b013e3181810378
- Hayes, M.A., Timmins, A.C., Yau, E.H., et al. (1994) Elevation of Systemic Oxygen Delivery in the Treatment of Critically Ill Patients. The New England Journal of Medicine, 330, 1717-1722. http://dx.doi.org/10.1056/NEJM199406163302404
- Deal, E.N., Hollands, J.M., Schramm, G.E., et al. (2008) Role of Corticosteroids in the Management of Acute Respiratory Distress Syndrome. Clinical Therapeutics, 30, 787-799. http://dx.doi.org/10.1016/j.clinthera.2008.05.012
- Sakr, Y., Vincent, J.L., Reinhart, K., et al. (2005) High Tidal Volume and Positive Fluid Balance Are Associated with Worse Outcome in Acute Lung Injury. Chest, 128, 3089-3091. http://dx.doi.org/10.1378/chest.128.5.3098
- Numa, A.H. (2001) Acute Lung Injury: Outcomes and New Therapies. Numa AH. Pediatric Respiratory Review, 2, 22-31. http://dx.doi.org/10.1053/prrv.2000.0097
- Hager, D.N., Krishnan, J.A., Hayden, D.L., et al. (2005) Tidal Volume Reduction in Patients with Acute Lung Injury When Plateau Pressures Are Not High. American Journal of Respiratory and Critical Care Medicine, 172, 1241-1245. http://dx.doi.org/10.1164/rccm.200501-048CP
- Leibowitz, A.B. and Porter, S.B. (2009) Perioperative Beta-Blockade in Patients Undergoing Noncardiac Surgery: A Review of the Major Randomized Clinical Trials. Journal of Cardiothoracic and Vascular Anesthesia, 23, 684-693. http://dx.doi.org/10.1053/j.jvca.2009.01.017
- Bangalore, S., Wetterslev, J., Pranesh, S., et al. (2008) Perioperative Beta Blockers in Patients Having Non-Cardiac Surgery: A Meta-Analysis. Lancet, 372, 1962-1976. http://dx.doi.org/10.1016/S0140-6736(08)61560-3
- Chopra, V., Plaisance, B., Cavusoglu, E., et al. (2009) Perioperative Beta-Blockers for Major Noncardiac Surgery: Primum Non Nocere. American Journal of Medicine, 122, 222-229. http://dx.doi.org/10.1016/j.amjmed.2008.11.004
- POISE Study Group, Devereaux, P.J., Yang, H., Yusuf, S., et al. (2008) Effects of Extended-Release Metoprolol Succinate in Patients Undergoing Non-Cardiac Surgery (POISE Trial): A Randomized Controlled Trial. Lancet, 31, 1839-1847.
- Furnary, A.P., Zerr, K.J., Grunkemeier, G.L., et al. (1999) Continuous Intravenous Insulin Infusion Reduced the Incidence of Deep Sternal Wound Infection in Diabetic Patients after Cardiac Surgical Procedures. The Annals of Thoracic Surgery, 67, 352-360. http://dx.doi.org/10.1016/S0003-4975(99)00014-4
- Lazar, H.L., Chipkin, S.R. and Fitzgerald, C.A. (2004) Tight Glycemic Control in Diabetic Coronary Artery Bypass Graft Patients Improves Perioperative Outcomes and Decreases Recurrent Ischemic Events. Circulation, 109, 1497- 1502. http://dx.doi.org/10.1161/01.CIR.0000121747.71054.79
- Scott, J.F., Robinson, G.M. and French, J.M. (1999) Glucose Potassium Insulin Infusions in the Treatment of Acute Stroke Patients with Mild to Moderate Hyperglycemia: The Glucose Insulin in Stroke Trial (GIST). Stroke, 30, 793- 799. http://dx.doi.org/10.1161/01.STR.30.4.793
- Malmberg, K., Ryden, L., Efendic, S., et al. (1995) Randomized Trial of Insulin-Glucose Infusion Followed by Sub-Cutaneous Insulin Treatment in Diabetic Patients with Acute Myocardial Infarction (DIGAMI Study): Effects on Mortality at One Year. Journal of the American College of Cardiology, 26, 57-65. http://dx.doi.org/10.1016/0735-1097(95)00126-K
- Krinsley, J.S. and Grover, A. (2007) Severe Hypoglycemia in Critically Ill Patients: Risk Factors and Outcomes. Critical Care Medicine, 35, 2262-2267. http://dx.doi.org/10.1097/01.CCM.0000282073.98414.4B
- Wintergerst, K.A., Buckingham, B., Gandrud, L., et al. (2006) Association of Hypoglycemia, and Glucose Variability with Morbidity and Death in the Pediatric Intensive Care Unit. Pediatrics, 118, 173-179. http://dx.doi.org/10.1542/peds.2005-1819
- Belsey, J.D., Pittard, J.B., Rao, S., et al. (2009) Self Blood Glucose Monitoring in Type 2 Diabetes. A Financial Impact Analysis Based on UK Primary Care. International Journal of Clinical Practice, 63, 439-448. http://dx.doi.org/10.1111/j.1742-1241.2008.01992.x
NOTES

*Corresponding author.
#Independent author.


