Surgical Science
Vol. 3 No. 6 (2012) , Article ID: 19917 , 5 pages DOI:10.4236/ss.2012.36058
Literature Review of the Frequency of Reoperations after One Stage Transanal Endorectal Pull-Through Procedure for Hirschsprung’s Disease in Children
1Autonomous University of Barcelona, Barcelona, Spain
2Department of Pediatric Surgery, Skåne University Hospital, Lund University, Lund, Sweden
Email: *carloslopera.ma@gmail.com
Received May 4, 2012; revised May 27, 2012; accepted June 10, 2012
Keywords: Transanal Endorectal Pull-Through (TERPT); Hirschsprung’s Disease; Postoperative Complications; Stricture; Enterostomy
ABSTRACT
Background: Transanal endorectal one-stage pull-through (TERPT) procedure in children with Hirschsprung’s disease (HD) has gained worldwide acceptance. However surgical success is often reported separately, while the necessity for true reoperation is difficult to establish. Aim: To evaluate the incidence of reoperations following TERPT procedure. The findings will be important in counseling and planning childcare for HD patients as well as providing a benchmark for single centers clinical results. Methods: A literature review of reported TERPT operations on children with HD between 1998 through 2011 was performed. Only planned TERPT operation reports were included. Information was collected with particular emphasis on reoperations and their reasons. Results: Out of 26 published articles 23 were included, reporting on 836 children, female/male ratio: 1/3.3, undergoing the TERPT procedure as the only operative intervention with described postoperative courses. The children comprised neonates, <4 weeks (38%), babies <1 year (35%), toddlers, 1 - 3 years (15%) and children >3 years of age (12%). The average follow up was 18.5 (6 - 38) months. The resected bowel length mean was 20.5 cm. Forty-one reoperations were reported (4.9%), including 24 laparotomies, 8 laparoscopies, 6 colostomies and ileostomies in 3 children. Only 2 re-do TERPT were reported (0.2%). Seven patients were considered TERPT failures (0.8%) with 5 requiring diverting colostomies and additional transabdominal pullthrough operations. Two myectomies were performed (0.2%). One child with aganglionosis underwent a Duhamel pull through. Two (0.2%) had serious damage to the urinary tract also one child with a vas deferens lesion was reoperated. Two bowel obstructions required adhesiolysis. Eight anastomotic dehiscences (0.9%) required surgery after reparation. One prolapse of the pulled through colon was reported. Six patients (0.7%) suffered anastomotic leaks. Anastomotic strictures rate was 2.8%, all repaired with anal dilatation. Conclusion: The review supports the low incidence of reported reoperations for the TERPT procedure.
1. Introduction
Since its introduction [1] more than a decade ago the transanal endorectal pull-through (TERPT) for Hirschsprung’s disease (HD) has been in common use. The TERPT procedure is less invasive than previously used procedures for HD. Since it includes minimal intra-abdominal dissection only, it results in less postoperative pain and shorter hospitalization. The cosmetic results are good with no visual scars.
A comparison of TERPT with previously used procedures would be desirable. However, only a few studies reported in the literature compared the different operative procedures for HD [2,3]. In centers where the TERPT procedure has been introduced, the older procedures are no longer in use and interest for them has diminished. At the same time postoperative complications after TERPT, such as the frequency of reoperations, have not been thoroughly assessed.
This review was undertaken to assess the incidence of postoperative complications after the TERPT procedure leading to reoperations in children with HD. We are not aware of any similar reports in the literature. The findings will be of importance in preoperative counseling and planning of childcare for HD children undergoing the TERPT procedure as well as providing a benchmark for single centers’ clinical results.
2. Methods
A literature review of reported TERPT operations on children with HD between 1998 through 2011 was performed. Only planned TERPT operation reports were included. Information was collected with particular emphasis on reoperations and their reasons. MEDLINE and EMBASE were searched for all studies reporting on children who had undergone surgical intervention for HD using TERPT between 1998 through 2011.
The search terms used were:
• Transanal endorectal pull-through
• Hirschsprung’s disease
• Newborns The reference list from the retrieved articles was reviewed for additional reports on children undergoing TERPT. All published reports and abstracts presented at meetings were evaluated.
Detailed information was recorded regarding the type of study, children’s age and gender, intraoperative details including the length of the bowel affected by HD and postoperative complications with particular emphasis on the frequency of reoperations and the reasons for them. Postoperative problems solved at the outpatient clinic without operative intervention were excluded.
3. Results
Results: Of 26 published articles, 23 were included [4-27]. These 23 publications reported on 836 children undergoing the TERPT procedure as the only operative intervention with described postoperative courses. The demography of the children included in the survey is summarized in Table 1. The mean length of the resected bowel was 20.5 cm. The average follow up time was 18.5 (6 - 38) months.
The type and frequency of the reported reoperations after TERPT operations in children are summarized in Table 2. Forty-one reoperations were reported (4.9%), including 24 laparotomies, 8 laparoscopies, and there
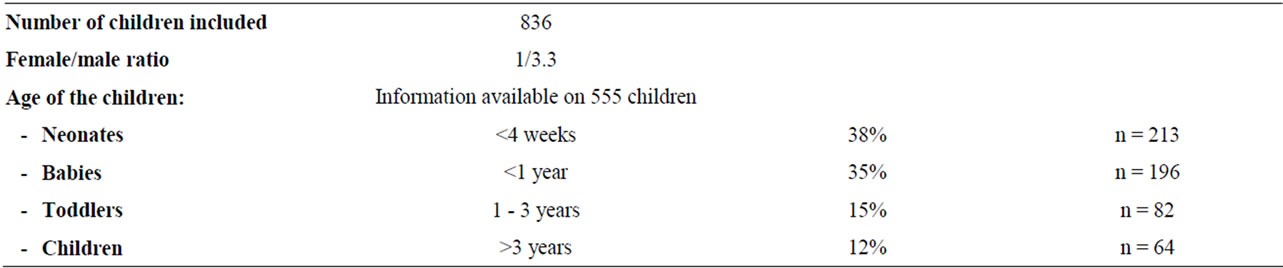
Table 1. Information available on 555 children.
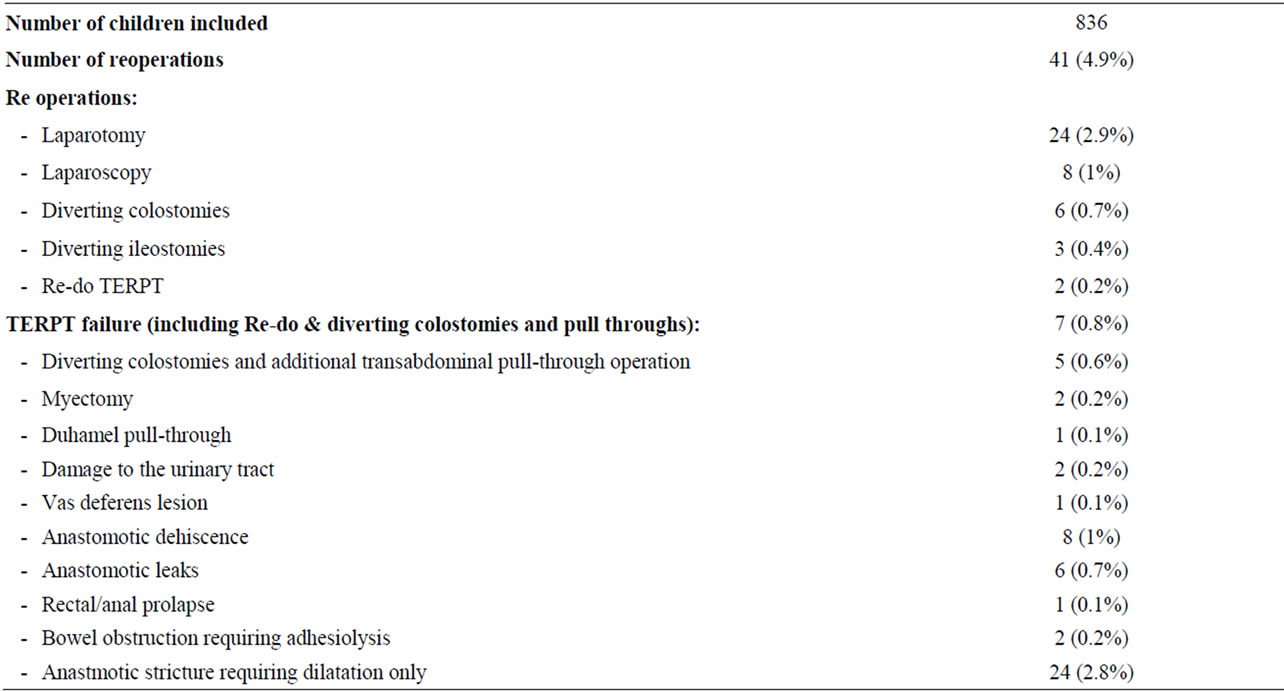
Table 2. A summary of the type and frequency of the reported reoperations after TERPT operations in children.
were 6 colostomies and ileostomies in 3 children. Only 2 re-do TERPT were reported (0.2%). Seven patients were considered TERPT failures (0.8%) with 5 requiring diverting colostomies and additional transabdominal pullthrough operations. Two myectomies were performed (0.2%). One child with aganglionosis underwent a Duhamel pull through.
Two (0.2%) had serious damage to the urinary tract and one child with a vas deferens lesion was reoperated. Two bowel obstructions required adhesiolysis. Eight anastomotic dehiscence (0.9%) required surgery after reparation. One prolapse of the pulled through colon was reported. Six patients (0.7%) suffered anastomotic leaks. Anastomotic stricture rate was 2.8%, all repaired with anal dilatation and not included in the group of children requiring reoperations.
4. Discussion
The results of a literature survey of reports on transanal endorectal pull-through (TERPT) for Hirschsprung’s disease in children, with particular emphasis on reoperations and the reasons for them, revealed that the number of reoperations was low after performing a TERPT operation for Hirschsprung’s disease in children. However, in spite of this low frequency there are some serious postoperative consequences of this procedure.
One of these is damage to the urinary tract and a vas deferens lesion. Rectourethral and rectovaginal fistulae are absolutely unacceptable complications and can be avoided by adherence to basic surgical principles [28].
The observation time reported in the publications studied is short, 18.5 months, (range 6 - 38 months). Some complications leading to reoperations may be discovered later, although the majority of the reoperations are probably performed shortly after the TERPT operation. Some authors [29] anticipate the need of a re-do pull-through, either with TERP or with other techniques at a later date after the TERPT, but the follow up time is too short to evaluate this suspicion.
Enterocolitis is a potentially life-threatening complication after TERPT operations, occurring in 4.6% to 54% of the children. Many of the children hit by this complication are treated conservatively only, and less than 20% of these are in need of operative intervention [30]. Abscesses were mostly treated conservatively, while there were two cases that required surgical drainage [11,29], one including a colostomy after the drainage had been performed.
A review of the literature can be used to evaluate it both qualitatively and quantitatively by comparing and integrating results of different studies, accounting for variations in characteristics that can influence the overall estimate of the outcome in question. It is important, however, to address the limitations of the literature review; there is a bias in this report due to several reasons.
Firstly, different studies may have had slightly different defining criteria for the outcome measures. This would certainly not apply to the complications in need of operative interventions which are relatively homogeneously reported throughout the studies. In this report, every attempt is made to select outcome measures that are as absolute as possible, such as operative complications leading to re-do. These parameters can hardly become influenced by local traditions and the child’s situation compared with the treatment of enterocolitis where not all the patients undergo any operative intervention.
Secondly, it is important to bear in mind a non-publication bias, particularly in a review based on published studies. The studied material is, moreover, biased by the fact that some of the authors do not report their results. Thus, we have probably missed a considerable number of operated children as well as several complications that have not been reported.
Thirdly, the duration of the observation time is short, even if it is long enough to evaluate functional bowel movement, and the chances of re-do surgery. Some complications requiring reoperation may be discovered later. We are not able to establish a normal sphincter function in the neonatal group. In all groups and cases there is no chance of evaluation of the sexual function. In some patients intraoperative damage of the sexual organs leads to reoperation [16].
Fourth, the length of the resected bowel in the reported children is 20.5 cm only and thus representing the group of children suitable for the TERPT operation and excluding those where laparoscopy or laparotomy is used to facilitate the intervention due to a preoperative clinical suspicion of a longer malformed bowel. It was not possible to differentiate the length of the aganglionotic segment from rectum, recto-sigmoideum and recto descendens and longer, due to missing data in most of the studies.
Fifth: There may be a variation in inclusion criteria, a study type, lack of randomization, treatment protocol, and outcome assessment between the studies.
The literature also reveals a considerable number of patients with Down’s syndrome [7,9,14] Ondine’s curse or congenital central hypoventilation syndrome (CCHS) [16,22] and congenital heart diseases [16], who were often excluded from the studies, or needed surgery related to these diseases but not considered as TERPT complications. Some deaths due to other diseases or causes were reported but none related to the TERPT procedure.
Finally the studies included in this paper reported results from a pediatric population only. This population represents a wide age range from newborns to 15 years old, while the great majority of the children included here are under three years of age.
In conclusion, the review supports the low incidence of reported reoperations after the TERPT procedure. The results of this review are of importance in preoperative counseling and when planning for the postoperative care of children with HD undergoing the TERPT procedure. Furthermore, the results may provide a benchmark for single centers’ clinical results.
REFERENCES
- L. De la Torre-Mondragón and J. A. Ortega-Salgado, “Transanal Endorectal Pull-Through for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 34 No. 3, 1998, pp. 1283-1286.
- A. Gunnarsdóttir, L. T. Larsson and E. Arnbjörnsson, “Transanal Endorectal vs. Duhamel Pull-Through for Hirschsprung’s Disease,” European Journal of Pediatric Surgery, Vol. 20, No. 4, 2010, pp. 242-246.
- A. C. Tannuri, U. Tannuri and R. L. Romão, “Transanal Endorectal Pull-Through in Children with Hirschsprung’s Disease—Technical Refinements and Comparison of Results with the Duhamel Procedure,” Journal of Pediatric Surgery, Vol. 44, No. 4, 2009, pp. 767-772. doi:10.1016/j.jpedsurg.2008.08.002
- C. T. Albanese, R. W. Jennings, B. Smith, B. Bratton and M. R. Harrison, “Perineal One-Stage Pull-Through for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 34, No. 3, 1999, pp. 377-380. doi:10.1016/S0022-3468(99)90480-3
- M. K. Aslan, I. Karaman, A. Karaman, D. Erdoğan, Y. H. Cavuşoğlu and O. Cakmak, “Our Experience with Transanal Endorectal Pull-Through in Hirschsprung’s Disease,” European Journal of Pediatric Surgery, Vol. 42, No. 7, 2007, pp. 335-339. doi:10.1055/s-2007-965447
- O. Ateş, G. Hakgüder, Y. Kart, M. Olguner and F. M. Akgür, “The Effect of Dilated Ganglionic Segment on Anorectal and Urinary Functions During 1-Stage Transanal Endorectal Pull through for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 42, No. 7, 2007, pp. 1271-1275.
- L. de la Torre and A. Ortega, “Transanal versus Open Endorectal Pull-Through for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 35, No. 8, 2000, pp. 1630-1632. doi:10.1053/jpsu.2000.18338
- G. Ekema, D. Falchetti, F. Torri, V. E. Merulla, A. Manciana and G. Caccia, “Further Evidence on Totally Transanal One-Stage Pull-Through Procedure for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 38, No. 10, 2003, pp. 1434-1439. doi:10.1016/S0022-3468(03)00492-5
- Y. Gao, G. Li, X. Zhang, Q. Xu, Z. Guo, B. Zheng and P. Li, G. Li, “Primary Transanal Rectosigmoidectomy for Hirschsprung’s Disease: Preliminary Results in the Initial 33 Cases,” Journal of Pediatric Surgery, Vol. 36, No. 12, 2001, pp. 1816-1819. doi:10.1053/jpsu.2001.28847
- A. Hadidi, “Transanal Endorectal Pull-Through for Hirschsprung’s Disease: Experience with 68 Patients,” Journal of Pediatric Surgery, Vol. 38, No. 9, 2003, pp. 1337-1340. doi:10.1016/S0022-3468(03)00392-0
- M. E. Höllwarth, M. Rivosecchi, J. Schleef, S. Deluggi, G. Fasching, E. Ceriati, G. Ciprandi and F. De Peppo, “The Role of Transanal Endorectal Pull-Through in the Treatment of Hirschsprung’s Disease—A Multicenter Experience,” Pediatric Surgery International, Vol. 18, No. 5-6, 2002, pp. 344-348.
- Y. Huang, S. Zheng and X. Xiao, “A Follow-Up Study on Postoperative Function after a Transanal Soave 1-Stage Endorectal Pull-Through Procedure for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 43, No. 9, 2008, pp. 1691-1695. doi:10.1016/j.jpedsurg.2007.12.053
- I. Jester, S. Holland-Cunz, S. Loff, S. Hosie, K. Reinshagen, H. Wirth, M. Ali and K. L. Waag, “Transanal Pull-Through Procedure for Hirschsprung’s Disease: A 5-Year Experience,” European Journal of Pediatric Surgery, Vol. 19, No. 2, 2009, pp. 68-71. doi:10.1055/s-2008-1039052
- D. D. Jovanović, V. A. Milojković, Z. M. Stevanović and M. M. Vukadin, “Transanal One-Stage Endorectal Technique for Hirschprung’s Disease—A Preliminary Report of 24 Cases from a Single Institution,” Acta Chirurgica Iugoslavica, Vol. 56, No. 1, 2009, pp. 109-113. doi:10.2298/ACI0901109J
- H. Y. Kim and J. T. Oh, “Stabilization Period after 1-Stage Transanal Endorectal Pull-Through Operation for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 44, No. 9, 2009, pp. 1799-1804. doi:10.1016/j.jpedsurg.2008.10.070
- J. C. Langer, A. C. Durrant, L. de la Torre, D. H. Teitelbaum, R. K. Minkes, M. G. Caty, B. E. Wildhaber, S. J. Ortega, S. Hirose and C. T. Albanese, “One-Stage Transanal Soave Pull-Through for Hirschsprung’s Disease: A Multicenter Experience with 141 Children,” Annals of Surgery, Vol. 238, No. 4, 2003, pp. 569-583.
- A. Nasr and J. C. Langer, “Evolution of the Technique in the Transanal Pull-Through for Hirschsprung’s Disease: Effect on Outcome,” Journal of Pediatric Surgery, Vol. 42, No. 1, 2007, pp. 36-39. doi:10.1016/j.jpedsurg.2006.09.028
- F. Obermayr, P. Szavay, R. Beschorner and J. Fuchs, “Outcome of Transanal Endorectal Pull-Through in Patients with Hirschsprung’s Disease,” European Journal of Pediatric Surgery, Vol. 19, No. 4, 2009, pp. 220-223. doi:10.1055/s-0029-1220682
- A. Pratap, D. K. Gupta, V. C. Shakya, S. Adhikary, A. Tiwari, P. Shrestha, S. R. Pandey and R. K. Yadav, “Analysis of Problems, Complications, Avoidance and Management with Transanal Pull-Through for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 42, No. 11, 2007, pp. 1869-1876. doi:10.1016/j.jpedsurg.2007.07.017
- A. Pratap, V. C. Shakya, B. K. Biswas, A. Sinha, A. Tiwari, C. S. Agrawal and S. Adhikary, “Single-Stage Transanal Endorectal Pull-Through for Hirschsprung’s Disease: Perspective from a Developing Country,” Journal of Pediatric Surgery, Vol. 42, No. 3, 2007, pp. 532-535. doi:10.1016/j.jpedsurg.2006.10.049
- R. J. Rintala, “Transanal Coloanal Pull-Through with a Short Muscular Cuff for Classic Hirschsprung’s Disease,” European Journal of Pediatric Surgery, Vol. 13, No. 3, 2003, pp. 181-186.
- E. Sapin, A. Centonze, R. Moog, J. Borgnon and F. Becmeur, “Transanal Coloanal Anastomosis for Hirschsprung’s Disease: Comparison between Endorectal and Perirectal Pull-Through Procedures,” European Journal of Pediatric Surgery, Vol. 16, No. 5, 2006, pp. 312-317. doi:10.1055/s-2006-924523
- S. Teeraratkul, “Transanal One-Stage Endorectal PullThrough for Hirschsprung’s Disease in Infants and Children,” Journal of Pediatric Surgery, Vol. 38, No. 2, 2003, pp. 184-187. doi:10.1053/jpsu.2003.50039
- Vijaykumar, A. Chattopadhyay, R. Patra and M. Murulaiah, “Soave Procedure for Infants with Hirschsprung’s Disease,” Indian Journal of Pediatrics, Vol. 69, No. 7, 2002, pp. 571-572. doi:10.1007/BF02722679
- T. Wester and R. J. Rintala, “Early Outcome of Transanal Endorectal Pull-Through with a Short Muscle Cuff during the neonatal period,” Journal of Pediatric Surgery, Vol. 39, No. 2. 2004, pp. 157-160. doi:10.1016/j.jpedsurg.2003.10.007
- A. Yamataka, K. Kaneyama, N. Fujiwara, Y. Hayashi, G. J. Lane, K. Kawashima and T. Okazaki, “Rectal Mucosal Dissection during Transanal Pull-Through for Hirschsprung’s Disease: The Anorectal or the Dentate Line?” Journal of Pediatric Surgery, Vol. 44, No. 1, 2009, pp. 266-269. doi:10.1016/j.jpedsurg.2008.10.054
- S. C. Zhang, Y. Z. Bai, W. Wang and W. L. Wang, “Clinical Outcome in Children after Transanal 1-Stage Endorectal Pull-Through Operation for Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 40, No. 8, 2005, pp. 1307-1311. doi:10.1016/j.jpedsurg.2005.05.016
- A. Peña, M. Elicevik and M. A. Levitt, “Reoperations in Hirschsprung’s Disease,” Journal of Pediatric Surgery, Vol. 42, No. 6, 2007, pp. 1008-1013. doi:10.1016/j.jpedsurg.2007.01.035
- E. A. Elhalaby, A. Hashish, M. M. Elbarbary, H. A. Soliman, M. K. Wishahy, A. Elkholy, S. Abdelhay, M. Elbehery, N. Halawa, T. Gobran, S. Shehata, N. Elkhouly and A. F. Hamza, “Transanal One-Stage Endorectal Pull-Through for Hirschsprung’s Disease: A Multicenter Study,” Journal of Pediatric Surgery, Vol. 39, No. 3, 2004, pp. 345-351. doi:10.1016/j.jpedsurg.2003.11.038
- E. Ruttenstock and P. Puri, “Systematic Review and Meta-Analysis of Enterocolitis after One-Stage Transanal Pull-Through Procedure for Hirschsprung’s Disease,” Pediatric Surgery International, Vol. 26, No. 11, 2010, pp. 1101-1105. doi:10.1007/s00383-010-2695-1
NOTES
*Corresponding author.

