Surgical Science
Vol. 3 No. 2 (2012) , Article ID: 17429 , 7 pages DOI:10.4236/ss.2012.32012
Obstructive Sleep Apnea and Post-Operative Complications: Single Center Data, Review of Literature and Guidelines for Practicing Internists and Surgeons
Texas Tech University Health Sciences Center, Lubbock, USA
Email: {*rishi.raj, kenneth.nugent, michael.phy}@ttuhsc.edu
Received October 18, 2011; revised November 22, 2011; accepted December 9, 2011
Keywords: Obstructive Sleep Apnea; Postoperative Complications; Pre-Operative Evaluation
ABSTRACT
Obstructive sleep apnea has been linked to higher rates of post-operative complications in some studies. We examined the prevalence of obstructive sleep apnea and its impact on post-operative complications in 125 patients (21 prospective, 104 retrospective) undergoing various elective outpatient surgeries at our institution. Ten percent of these patients had OSA, and half of them were on continuous positive airway pressure therapy (CPAP). Patients who were on CPAP as outpatients received CPAP post-operatively as well. No patients died, and the prevalence of post-operative complications was low. There was no difference in complication rates between patients with and without OSA. We also review the existing literature on this subject and make practical recommendations regarding pre-operative evaluation and postoperative management of these patients for practicing internists and surgeons based on the current literature.
1. Introduction
Obstructive sleep apnea, a relatively common comorbidity in middle aged adults, is even more prevalent in the highly selected patient populations encountered by physicians performing preoperative evaluations and risk stratification [1]. Studies have estimated the prevalence of OSA in highly select patient populations such as those undergoing bariatric surgery [2], orthopedic [3] or cardiovascular surgery [4], but few studies address the prevalence of this disorder in a diverse patient population similar to that encountered by most internists or surgeons providing preoperative care to patients in their practice. Patients with obstructive sleep apnea have an increased risk for complications when undergoing surgical procedures, but the existing data derive from retrospective or observational studies, and it is unclear if OSA is associated with increased incidence of postoperative complications, independent of BMI and other comorbidities. This study was designed to determine if the presence of previously diagnosed OSA is associated with increased risk of perioperative and postoperative complications in a patient population similar to that a general internist and surgeon might encounter. We also reviewed the literature to develop simple guidelines for screening and management of patients with OSA undergoing surgery.
2. Materials and Methods
2.1. Patient Population
The study was initiated after appropriate IRB approval. Our department has a dedicated Internal Medicine Preoperative Evaluation Clinic for patients undergoing elective outpatient surgical procedures. Patients referred to this clinic generally have multiple comorbidities and risk factors for postoperative complications. The study population included 125 patients from this clinic who eventually underwent orthopedic, general surgical, gynecologic, urologic, ENT, and ophthalmologic surgical procedures. Of these, 21 patients were enrolled prospectively, and the remaining 104 patients’ charts were reviewed retrospectively.
2.2. Data Collection and Analysis
The patients in the prospective group were interviewed by the research staff immediately after they were seen by the single physician who runs the clinic. All patient charts including those in the prospective group were reviewed, and data relevant to patient demographics, medical condition, risk factors, and postoperative outcome were abstracted and analyzed. Risk factors for postoperative complications included the ACCAHA score, ASA score, and the presence of comorbidities, including hypertension, diabetes, coronary artery disease, congestive heart failure, arrhythmias, cerebrovascular disease, chronic obstructive disease, and obstructive sleep apnea. Perioperative and postoperative outcomes included difficult intubation, need for re-intubation, mortality, admission to the intensive care unit, unanticipated ICU transfer, length of hospital stay, new onset myocardial infarction, new onset renal failure, new onset cardiac arrhythmia, pulmonary emboli, hypoxemia, need for oxygen supplementation, respiratory failure needing invasive or noninvasive ventilation, wound infections, and the need for admission to a rehabilitation program. Statistical Package for Social Sciences (SPSS) version 17.0 was used for statistical analysis. Parametric and non-parametric tests including Whitney ranksum and T-test were used as appropriate to assess group differences for continuous variables. Chi-square analysis of contingency tables was used to assess group differences for discreet variables and Fisher’s exact test was used when each cell had expected frequency of less than 5. A p value of <0.05 was considered statistically significant.
3. Results
3.1. Population Characteristics
The prospective and retrospective groups did not differ from each other in age, sex, comorbidities, ACCAHA score, AHA score, perioperative complications, postoperative complications, mortality, or any other variable measured in this study. The prospective and retrospective groups were therefore combined and analyzed as a single group. Table 1 summarizes the baseline clinical characteristics of the

Table 1. Demographic and baseline comorbidity characteristics of 125 patients in the study.
study patients’ demographics and comorbidities. The patients underwent orthopedic, general surgical, gynecologic, urologic, ENT and ophthalmologic surgical procedures, and the percentage of patients undergoing various surgical procedure types is summarized in Table 2. Sixty four percent of patients were hospitalized post-procedure, and the remaining 36% were discharged home after the surgery. Most patients (92%) received general anesthesia, and the remaining 8% of patients received a local, regional or spinal anesthesia.
3.2. Postoperative Course and Complications
No post procedure deaths occurred. Postoperative complications were relatively infrequent, and Table 3 summarizes the incidence of postoperative complications in this patient population. Complications included postoperative hypoxemia requiring oxygen supplementation, respiratory failure requiring mechanical ventilation, myocardial arrhythmia, renal failure, wound infection, unplanned admission to the intensive care unit, unplanned admissions for outpatient surgical procedures and myocardial infarction.
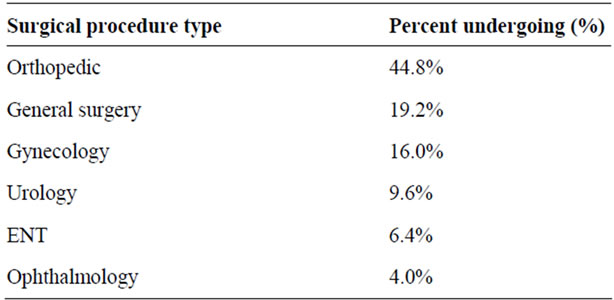
Table 2. Type of surgical procedures.
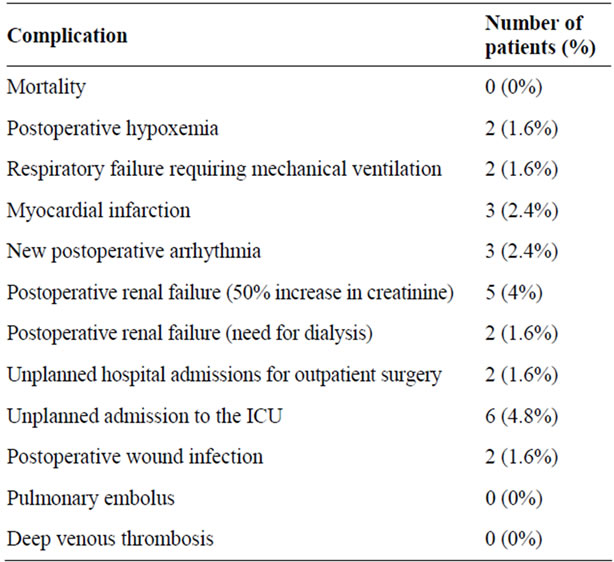
Table 3. Incidence of postoperative complications for the entire group.
Acute myocardial infarction was defined as the presence any one or more of the following criteria postoperatively: elevation of total CK-MB isoenzyme, elevated troponin T values, or new diagnostic ECG changes (new Q wave, new persistent ST segment elevation/depression or Q wave changes). No difficult intubations were reported, and none of the patients needed reintubation. There was no difference in the number of attempts for intubation between patients with and without obstructive sleep apnea. The average duration of hospitalization for those who were hospitalized was 6 (3.1) days. The patients who were admitted to the ICU spent an average of 2.9 (1.9) days in the intensive care unit.
3.3. Obstructive Sleep Apnea
Twelve patients (10%) had previously diagnosed obstructive sleep apnea. Five patients (42%) were using positive airway pressure therapy (CPAP), and one patient was using oxygen alone at the time of preoperative evaluation. The remaining six patients (50%) were not using oxygen or positive airway pressure therapy (CPAP). Patients who were using CPAP as outpatients were prescribed CPAP postoperatively and during hospitalization, and the patients who were not on CPAP as outpatients were not prescribed CPAP postoperatively and during hospitalization. The average AHI for patients for which the sleep study data was available was 14.5. Table 4 compares the baseline characteristics of patients with and without OSA. Patients with OSA had a higher body mass index and a higher prevalence of diabetes mellitus. There was no difference in other baseline characteristics or comorbidities in patients with or without OSA. Postoperative complications were relatively infrequent, and there were no differences in the incidence of postoperative complications between patients with and without OSA (Table 5). There was a higher frequency of unplanned hospital admissions and postoperative myocardial infarctions in patients with OSA, but this did not reach statistical significance.
4. Discussion
4.1. Magnitude of Problem
Population studies suggest that OSA is present in 2% of women and 4% of middle-aged men in the general population in the United States [1]. The true prevalence of OSA in the populations encountered by clinicians in their dayto-day practice depends largely on the demographic and comorbidity composition of that particular patient population. A prevalence as high at 71% has been reported in one particular series consisting of patients undergoing bariatric surgery [2]. Most published data come from specific patient populations, like patients undergoing upper airway surgery, orthopedic surgery [3] or cardiovascular surgery [5]. Our study is different since it includes a diverse patient population undergoing various general surgical, orthopedic, urologic, and other surgical procedures, similar to patients encountered by internists providing preoperative evaluation and postoperative care to patients in most general internal medicine practices. Ten percent of our patients had obstructive sleep apnea, similar to the
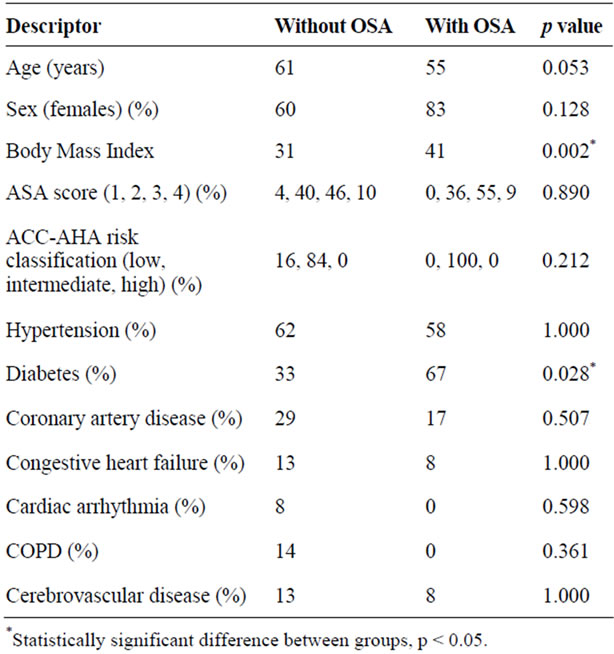
Table 4. Comparison of the baseline characteristics of patients with and without OSA.
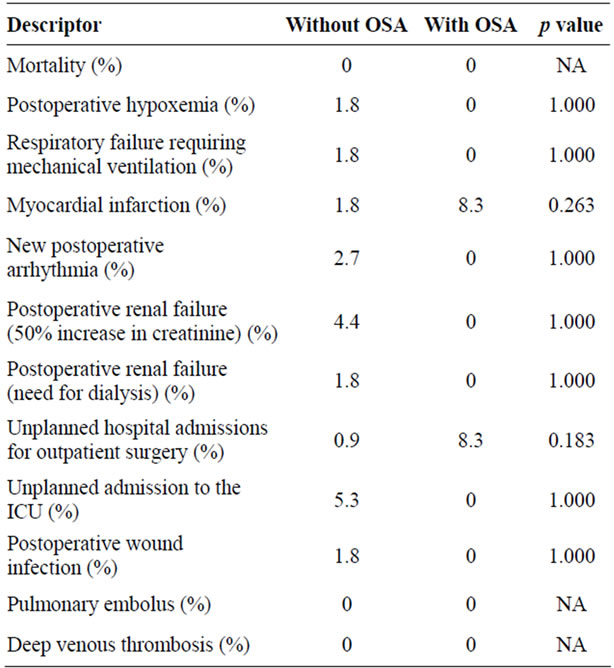
Table 5. Comparison of the postoperative complication rates in patients with and without OSA.
prevalence of 9.5% in patients undergoing general surgical procedures, excluding cardiac and OSA surgery, as reported by Fidan, et al. [6].
4.2. Preoperative Screening and Evaluation for OSA
Although patients with obstructive sleep apnea have an increased risk for perioperative and postoperative complications, there are no definite guidelines for screening preoperative patients for obstructive apnea, and it is unclear if preoperative screening and treatment of these patients alters the postoperative outcome. The ten item Berlin questionnaire [7], the 16 item ASA screening questionnaire [8], and the more recently described four item STOP questionnaire [9] can be used to screen preoperative patients for obstructive sleep apnea. These questionnaires have a sensitivity from 0.66 to 0.89 and a specificity from 0.71 to 0.89 depending on the patient population and the AHI cutoff used for obstructive sleep apnea [9,10]. Addition of BMI, neck circumference, age and gender data to the STOP questionnaire [9] increases the sensitivity to detect OSA of AHI > 30/hr to 100% [9].
Diagnostic polysomnography, the gold standard for diagnosing obstructive sleep apnea [11], can be performed in patients suspected to have OSA based on the results of these screening tools. What is less clear is whether treatment of OSA in patients with varying severity of OSA alters postoperative outcomes. Diagnostic polysomnography may therefore be neither practical nor necessary for most patients with suspected OSA about to undertake surgery [12]. Although no prospective controlled studies exist, data from retrospective and observational studies suggest that postoperative treatment of patients with OSA with positive airway pressure therapy reduces postoperative complications [3,13]. Routine diagnostic polysomnography cannot be recommended for patients undergoing semi-elective or urgent procedures based on current data but can probably be considered for patients undergoing elective surgery with the provision that this recommenddation is based on limited retrospective data only.
4.3. Obstructive Sleep Apnea and Anesthesia
Benzodiazepines [14,15], opioids [16] and other anesthetic agents [17] cause respiratory depression and relaxation of the upper airway muscles resulting in decreased respiratory drive and increased collapsibility of the upper airway even in individuals with normal upper airway anatomy and respiratory drive. The upper airway in patients with obstructive sleep apnea is narrower when compared to normal individuals [18] during wakefulness and exhibit an increased tendency towards collapse and airway closure during sleep [19]. When compared to normal individuals, patients with obstructive sleep apnea are more susceptible to hypoventilation and upper airway collapse induced by alcohol [20] and other anesthetic agents [21]. Additionally, it appears that upper airway collapse rather than suppression of the respiratory drive is primarily responsible for desaturation associated with these medications [16,22]. Difficult intubation [23] and the need for re-intubation [3] have been reported in patients with OSA in some [3,23] but not all [4,24] of the studies. There were no failed intubations in any of the patients in our study. There was no difference between the number of attempts for first intubation or re-intubations between patients with or without OSA in our study.
4.4. Obstructive Sleep Apnea and Postoperative Complications
Retrospective and observational studies [25,26] in patients undergoing upper airway surgery have noted postoperative complications in these patients, but the lack of randomization and proper controls preclude the determination of the exact contribution of obstructive sleep apnea, other comorbidities, and the surgical procedure to the complications in these studies. Case reports [27,28] and observational studies [3-5,12,29,30] suggest an increased rate of perioperative complications in patients with obstructive sleep apnea undergoing non upper-airway surgery, but this finding is by no means universal [24]. Overall, there is insufficient data from randomized trials in the published literature regarding obstructive sleep apnea as a risk for increased cardiovascular or respiratory complications postoperatively, independent of other comorbidities and obesity [31].
Analysis of the studies showing an increased rate of perioperative and postoperative complications in patients with obstructive sleep apnea reveals that the patient population without OSA within the studies differs from that with OSA. In addition, many complications do not involve the respiratory or cardiovascular systems. These complications cannot be directly attributed to obstructive sleep apnea, and alternative explanations exist. In the 37 patients undergoing cardiac surgery described by Kaw et al. postoperative encephalopathy and mediastinitis were the only complications that were observed more frequently in the OSA group [4]. Patients without OSA in the series reported by Hwang et al. [29] had a lower BMI and had complications like pulmonary embolism and postoperative bleeding. There was a trend towards a higher BMI in the control group in the series reported by Gupta et al. [3]. The patients in this study with OSA had a higher rate of ICU transfers but had similar rates of reintubation, acute hypercapnia, episodic hypoxemia, myocardial infarction, myocardial ischemia, arrhythmia, and delirium when compared to patients without OSA [3]. Sabers et al. did not find any difference in rates of postoperative complications or rate hospital admissions in the 234 OSA patients when compared to 234 control patients [24]. More recent larger retrospective observational studies using pre-existing databases [12,30] that have controlled for confounding factors using propensity scores demonstrate an increased risk of aspiration pneumonia [30], respiratory failure [30], ARDS [30], postoperative hypoxemia [12], and longer length of hospital stay [12].
In summary, although there is insufficient Level I and II evidence to demonstrate that OSA increases postoperative complications, and review of the existing data does not clearly link OSA as being directly and independently responsible for postoperative complications, the existing literature does support concerns about more frequent respiratory and non-respiratory postoperative complications in patients with OSA.
4.5. Postoperative Management of Patients with OSA
Anecdotal evidence implicates opioids as a risk factor for cardiorespiratory arrest in patients with severe OSA [32,33], but controlled studies, especially in patients with mild to moderate OSA are non-existent. Level IV data from retrospective and observational studies suggest that positive airway pressure therapy for patients with obstructive sleep apnea reduces postoperative complications [3,13,33]. Although this benefit of using CPAP postoperatively is not universally confirmed in all studies [34,35], given the relative ease of application of CPAP and virtual absence of side effects/complications other than discomfort, postoperative CPAP should be recommended for all patients with OSA unless specific contraindications exist. Forty two percent of the patients in our study were prescribed CPAP postoperatively, and this could explain the lack of difference in postoperative outcomes between patients with and without OSA in the present study.
4.6. Study Limitations
The current study is limited by its relatively small size and absence of polysomnographic data on patients not known to have obstructive sleep apnea. It is possible that undiagnosed OSA in the group without known OSA and continued use of CPAP in postoperative period in patients known to have OSA contributed to the lack of any observed difference in complication rates between patients with and without OSA.
5. Conclusions
Our study includes a heterogeneous group of patients, similar to what many internists or surgeons participating in preoperative evaluation would encounter in their clinics, and found that 10% of our patients had obstructive sleep apnea. Obesity and diabetes mellitus were associated with an increased probability of OSA in our study. We did not systematically screen for OSA but patients with OSA who were on CPAP preoperatively were continued on CPAP in the postoperative period. There was no difference in preoperative or postoperative outcomes in patients with and without OSA in our study. Postoperative treatment of patients with OSA with CPAP and presence of undiagnosed OSA could potentially have contributed to the lack of difference in complication rates between patients with and without OSA. We identified relatively few serious postoperative complications in these patients and as long as patients with known OSA are recognized preoperatively and treated appropriately postoperatively, the incidence of adverse outcomes in these patients is similar to those without OSA.
6. Summary of Recommendations for Internists and Surgeons
We recommend the following diagnostic and therapeutic plan for patients with OSA:
1) Patients undergoing elective surgery should be systematically screened for OSA. Screening options in addition to a routine history and physical examination include the ASA questionnaire, STOP questionnaire, or the Berlin questionnaire. This would help to identify the subgroup of patients at higher risk for postoperative complications.
2) Patients undergoing elective surgery for whom time to surgery is not an immediate concern (for example, bariatric surgery) and in whom the physician has a high index of suspicion of sleep apnea based on the above screening tests can undergo a diagnostic polysomnography followed by treatment of OSA if appropriate (CPAP).This recommendation is based on limited retrospective data, and there are no good data showing that this approach leads to better outcomes when compared to no treatment pre or postoperatively.
3) Patients undergoing urgent surgery and patients undergoing elective surgery where time or resources are a concern should have screening for OSA using the tools mentioned above. If the patient appears to have a high probability of having OSA, appropriate measures should be taken in the perioperative and postoperative period. In the authors’ opinion there is inadequate evidence at this time to recommend delaying surgery until formal evaluation and treatment of OSA can be undertaken in patients undergoing urgent surgery.
4) For patients with OSA or for patients suspected to have OSA by screening tests, the following measures seem beneficial:
a) Anesthesiologists should anticipate difficult intubation or the need for re-intubation in these patients.
b) Physicians should use opioids or other medications that suppress respiration or relax airway muscles in the smallest possible doses.
c) Physicians and nurses should monitor these patients closely post-operatively and use oxygen or CPAP as appropriate. For patients with known OSA and a previous titration study, CPAP should be used at the same pressure setting. There are no guidelines for the recommended pressures for patients who have not had a prior titration polysomnography. For these patients, titration of positive airway pressure can be done using procedures similar to those followed in sleep laboratories. Patients can be started on CPAP pressures of 6 - 8 cm of water, and the pressure titrated upwards in 1 - 2 cm increments to eliminate frank apneas or episodic desaturation.
d) Discharging physicians should refer patients with a high probability of OSA but without a definite diagnosis for a formal diagnostic polysomnography after discharge.
REFERENCES
- T. Young, M. Palta, J. Dempsey, J. Skatrud, S. Weber and S. Badr, “The Occurrence of Sleep-Disordered Breathing among Middle-Aged Adults,” New England Journal of Medicine, Vol. 328, No. 17, 1993, pp. 1230-1235. doi:10.1056/NEJM199304293281704
- W. C. Frey and J. Pilcher, “Obstructive Sleep-Related Breathing Disorders in Patients Evaluated for Bariatric Surgery,” Obesity Surgery, Vol. 13, No. 5, 2003, pp. 676-683. doi:10.1381/096089203322509228
- R. M. Gupta, J. Parvizi, A. D. Hanssen and P. C. Gay, “Postoperative Complications in Patients with Obstructive Sleep Apnea Syndrome Undergoing Hip or Knee Replacement: A Case-Control Study,” Mayo Clinic Proceeding, Vol. 76, No. 9, 2001, pp. 897-905.
- R. Kaw, J. Golish, S. Ghamande, R. Burgess, N. Foldvary and E. Walker, “Incremental Risk of Obstructive Sleep Apnea on Cardiac Surgical Outcomes,” Journal of Cardiovascular Surgery (Torino), Vol. 47, No. 6, 2006, pp. 683-689.
- T. Mooe, S. Gullsby, T. Rabben and P. Eriksson, “SleepDisordered Breathing: A Novel Predictor of Atrial Fibrillation after Coronary Artery Bypass Surgery,” Coronary Artery Disease, Vol. 7, No. 6, 1996, pp. 475-478. doi:10.1097/00019501-199606000-00011
- H. Fidan, F. Fidan, M. Unlu, Y. Ela, A. Ibis and L. Tetik, “Prevalence of Sleep Apnoea in Patients Undergoing Operation,” Sleep Breath, Vol. 10, No. 3, 2006, pp. 161-165. doi:10.1007/s11325-006-0067-9
- R. S. Strauss and W. S. Browner, “Risk for Obstructive Sleep Apnea,” Annals of Internal Medicine, Vol. 132, No. 9, 2000, pp. 758-759.
- J. B. Gross, K. L. Bachenberg, J. L. Benumof, R. A. Caplan, R. T. Connis, C. J. Cote, D. G. Nickinovich, V. Prachand, D. S. Ward, E. M. Weaver, L. Ydens and S. Yu, “Practice Guidelines for the Perioperative Management of Patients with Obstructive Sleep Apnea: A Report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea,” Anesthesiology, Vol. 104, No. 5, 2006, pp. 1081-1093.
- F. Chung, B. Yegneswaran, P. Liao, S. A. Chung, S. Vairavanathan, S. Islam, A. Khajehdehi and C. M. Shapiro, “STOP Questionnaire: A Tool to Screen Patients for Obstructive Sleep Apnea,” Anesthesiology, Vol. 108, No. 5, 2008, pp. 812-821. doi:10.1097/ALN.0b013e31816d83e4
- F. Chung, B. Yegneswaran, P. Liao, S. A. Chung, S. Vairavanathan, S. Islam, A. Khajehdehi and C. M. Shapiro, “Validation of the Berlin Questionnaire and American Society of Anesthesiologists Checklist as Screening Tools for Obstructive Sleep Apnea in Surgical Patients,” Anesthesiology, Vol. 108, No. 5, 2008, pp. 822-830. doi:10.1097/ALN.0b013e31816d91b5
- “Practice Parameters for the Indications for Polysomnography and Related Procedures. Polysomnography Task Force, American Sleep Disorders Association Standards of Practice Committee,” Sleep, Vol. 20, No. 6, 1997, pp. 406-422.
- R. Kaw, V. Pasupuleti, E. Walker, A. Ramaswamy and N. Foldvary-Schafer, “Postoperative Complications in Patients with Obstructive Sleep Apnea,” Chest, 2011, PMID: 21868464.
- M. T. Rennotte, P. Baele, G. Aubert and D. O. Rodenstein, “Nasal Continuous Positive Airway Pressure in the Perioperative Management of Patients with Obstructive Sleep Apnea Submitted to Surgery,” Chest, Vol. 107, No. 2, 1995, pp. 367-374. doi:10.1378/chest.107.2.367
- S. Molliex, B. Dureuil, P. Montravers and J. M. Desmonts, “Effects of Midazolam on Respiratory Muscles in Humans,” Anesthesia & Analgesia, Vol. 77, No. 3, 1993, pp. 592-597. doi:10.1213/00000539-199309000-00029
- P. Montravers, B. Dureuil and J. M. Desmonts, “Effects of i.v. Midazolam on Upper Airway Resistance,” British Journal of Anaesthesia, Vol. 68, No. 1, 1992, pp. 27-31. doi:10.1093/bja/68.1.27
- D. M. Catley, C. Thornton, C. Jordan, J. R. Lehane, D. Royston and J. G. Jones, “Pronounced, Episodic Oxygen Desaturation in the Postoperative Period: Its Association with Ventilatory Pattern and Analgesic Regimen,” Anesthesiology, Vol. 63, No. 1, 1985, pp. 20-28. doi:10.1097/00000542-198507000-00004
- P. R. Eastwood, P. R. Platt, K. Shepherd, K. Maddison and D. R. Hillman, “Collapsibility of the Upper Airway at Different Concentrations of Propofol Anesthesia,” Anesthesiology, Vol. 103, No. 3, 2005, pp. 470-477. doi:10.1097/00000542-200509000-00007
- R. J. Schwab, K. B. Gupta, W. B. Gefter, L. J. Metzger, E. A. Hoffman and A. I. Pack, “Upper Airway and Soft Tissue Anatomy in Normal Subjects and Patients with SleepDisordered Breathing. Significance of the Lateral Pharyngeal Walls,” American Journal of Respiratory and Critical Care Medicine, Vol. 152, No. 5, 1995, pp. 1673-1689.
- W. S. Mezzanotte, D. J. Tangel and D. P. White, “Influence of Sleep Onset on Upper-Airway Muscle Activity in Apnea Patients versus Normal Controls,” American Journal of Respiratory and Critical Care Medicine, Vol. 153, No. 6, 1996, pp. 1880-1887.
- L. Scrima, M. Broudy, K. N. Nay and M. A. Cohn, “Increased Severity of Obstructive Sleep Apnea after Bedtime Alcohol Ingestion: Diagnostic Potential and Proposed Mechanism of Action,” Sleep, Vol. 5, No. 4, 1982, pp. 318-328.
- L. A. Connolly, “Anesthetic Management of Obstructive Sleep Apnea Patients,” Journal of Clinical Anesthesia, Vol. 3, No. 6, 1991, pp. 461-469. doi:10.1016/0952-8180(91)90094-4
- J. G. Jones, C. Jordan, C. Scudder, D. A. Rocke and M. Barrowcliffe, “Episodic Postoperative Oxygen Desaturation: The Value of Added Oxygen,” Journal of the Royal Society of Medicine, Vol. 78, No. 12, 1985, pp. 1019-1022.
- M. A. Siyam and D. Benhamou, “Difficult Endotracheal Intubation in Patients with Sleep Apnea Syndrome,” Anesthesia & Analgesia, Vol. 95, No. 4, 2002, pp. 1098-1102.
- C. Sabers, D. J. Plevak, D. R. Schroeder and D. O. Warner, “The Diagnosis of Obstructive Sleep Apnea as a Risk Factor for Unanticipated Admissions in Outpatient Surgery,” Anesthesia & Analgesia, Vol. 96, No. 5, 2003, pp. 1328-1335.
- D. J. Terris, E. F. Fincher, M. M. Hanasono, W. E. Fee Jr. and K. Adachi, “Conservation of Resources: Indications for Intensive Care Monitoring after Upper Airway Surgery on Patients with Obstructive Sleep Apnea,” Laryngoscope, Vol. 108, No. 6, 1998, pp. 784-788. doi:10.1097/00005537-199806000-00002
- E. M. Gessler and P. C. Bondy, “Respiratory Complications Following Tonsillectomy/UPPP: Is Step-Down Monitoring Necessary?” Ear, Nose and Throat Journal, Vol. 82, No. 8, 2003, pp. 628-632.
- K. Vidhani and B. T. Langham, “Obstructive Sleep Apnoea Syndrome: Is This an Overlooked Cause of Desaturation in the Immediate Postoperative Period?” British Journal of Anaesthesia, Vol. 78, No. 4, 1997, pp. 442-443.
- D. J. Cullen, “Obstructive Sleep Apnea and Postoperative Analgesia—A Potentially Dangerous Combination,” Journal of Clinical Anesthesia, Vol. 13, No. 2, 2001, pp. 83-85. doi:10.1016/S0952-8180(01)00261-6
- D. Hwang, N. Shakir, B. Limann, C. Sison, S. Kalra, L. Shulman, C. Souza Ade and H. Greenberg, “Association of Sleep-Disordered Breathing with Postoperative Complications,” Chest, Vol. 133, No. 5, 2008, pp. 1128-1134. doi:10.1378/chest.07-1488
- S. Memtsoudis, S. S. Liu, Y. Ma, Y. L. Chiu, J. M. Walz, L. K. Gaber-Baylis and M. Mazumdar, “Perioperative Pulmonary Outcomes in Patients with Sleep Apnea after Noncardiac Surgery,” Anesthesia & Analgesia, Vol. 112, No. 1, 2011, pp. 113-121. doi:10.1213/ANE.0b013e3182009abf
- S. A. Chung, H. Yuan and F. Chung, “A Systemic Review of Obstructive Sleep Apnea and Its Implications for Anesthesiologists,” Anesthesia & Analgesia, Vol. 107, No. 5, 2008, pp. 1543-1563. doi:10.1213/ane.0b013e318187c83a
- A. M. Ostermeier, M. F. Roizen, M. Hautkappe, P. A. Klock and J. M. Klafta, “Three Sudden Postoperative Respiratory Arrests Associated with Epidural Opioids in Patients with Sleep Apnea,” Anesthesia & Analgesia, Vol. 85, No. 2, 1997, pp. 452-460.
- M. K. Reeder, M. D. Goldman, L. Loh, A. D. Muir, K. R. Casey and D. A. Gitlin, “Postoperative Obstructive Sleep Apnoea. Haemodynamic Effects of Treatment with Nasal CPAP,” Anaesthesia, Vol. 46, No. 10, 1991, pp. 849-853. doi:10.1111/j.1365-2044.1991.tb09599.x
- C. Delclaux, E. L’Her, C. Alberti, J. Mancebo, F. Abroug, G. Conti, C. Guerin, F. Schortgen, Y. Lefort, M. Antonelli, E. Lepage, F. Lemaire and L. Brochard, “Treatment of Acute Hypoxemic Nonhypercapnic Respiratory Insufficiency with Continuous Positive Airway Pressure Delivered by a Face Mask: A Randomized Controlled Trial,” Journal of the American Medical Association, Vol. 284, No. 18, 2000, pp. 2352-2360. doi:10.1001/jama.284.18.2352
- G. B. Drummond, K. Stedul, R. Kingshott, K. Rees, A. F. Nimmo, P. Wraith and N. J. Douglas, “Automatic CPAP Compared with Conventional Treatment for Episodic Hypoxemia and Sleep Disturbance after Major Abdominal Surgery,” Anesthesiology, Vol. 96, No. 4, 2002, pp. 817-826. doi:10.1097/00000542-200204000-00007
NOTES
*Corresponding author.

