Advances in Microbiology
Vol.4 No.11(2014), Article ID:49477,8 pages
DOI:10.4236/aim.2014.411076
Status of Mycoplasma pneumoniae Pneumonia in Chinese Children: A Systematic Review
Qiang Qin, Baoping Xu, Xiuyun Liu, Kunling Shen*
Key Laboratory of Major Diseases in Child and National Key Discipline of Pediatrics (Capital Medical University), Department of Respiratory Medicine, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Email: *kunlingshen1717@163.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 30 April 2014; revised 28 May 2014; accepted 22 June 2014
ABSTRACT
Mycoplasma pneumoniae pneumonia (MPP) becomes one of the most important health problems in China recently. Date for MPP in China is scarce. Although macrolides and/or cortical steroids had been reported to be effective treatment for MPP, the long-term outcome remained uncertain. A study on status of MPP in China was conducted via a systematic review of published studies which have the Chinese data and collected from published PubMed and core journals of China Knowledge Resource Integrated Database (CNKI). The analysis was based on epidemiology, clinical characteristics, treatment, drug resistance and prognosis. Twenty five articles concerned about MPP in Chinese children and adolescent were enrolled, including 11 studies on epidemiology/etiology, 11 studies on clinical characteristics, 7 studies on drug resistance, 5 studies on treatment from mainland China respectively. The overall incidence of MPP ranged from 7.1% to 54.4%. Fever and cough were most frequently identified in manifestations. Drug resistance to macrolides ranged from 18.9% to 90%. The outcome of treatment in patients who received combined treatment of macrolides, cephalosporin antibiotics and/or cortical steroid seems to be better than those who received macrolides only. Macrolide combined with cephalosporin or cortical steroid both may decrease the severity of MPP in the past decade. There was not enough evidence to suggest that cortical steroid can decrease the mortality of MPP in children. And a multi-center, randomized double blind research on the effect of cortical steroid was encouraged.
Keywords:Mycoplasma pneumoniae, Pneumonia, Chinese Children, Systematic Review

1. Introduction
Mycoplasma pneumoniae (MP) is among the smallest microorganisms which is capable of self-replication, with a whole genome [1] . MP is a frequent cause of community acquired pneumonia (CAP) in children, which has been well described and is considered self-limited in most cases. When it adheres to human airway epithelial cells, MP can trigger a series of immunological responses, which result in both atypical respiratory tract symptoms (e.g. fever, cough, headache, sore throat, runny nose, general malaise) and various extra-pulmonary complications such as encephalitis, meningoencephalitis, Guillain-Barre syndrome, optic neuritis, nephritis, rash, arthritis, and pericarditis [2] . However, the number of severe cases and pulmonary complications appears to be increasing in recent years.
CAP is the main cause of hospitalization and death of children in China, especially for children 5 years old and younger. Although many studies have focused on etiologies of pneumonia, there are limited high quality data regarding MPP in China. The positive rates of MP infection range from 10% - 30%, and may reach 50% - 80% in years of peak incidence or during local outbreaks. Global pandemics of MP generally occur every 3 - 7 years, and may persist for 1 - 2 years [3] [4] . Because MP lacks a cell wall, it is not susceptible to penicillins and other β-lactam antibiotics. However, drug resistance to the macrolides has been observed in Mycoplasma pneumoniae strains and appears to have been increasing in China and other area all over the world since year 2000. Improving the therapeutic management of pneumonia has been defined by international experts as one of the top priorities to decrease the CAP burden and improve health worldwide [5] .
The present study was designed using a systematic review on the status of MPP patients in Chinese children, including the epidemiology, clinical characteristics, treatment, drug resistance and prognosis. Overall, the present study may provide a whole view on MP infection in large Chinese pediatric population.
2. Results
Screening process of studies is outlined in Figure 1. A total of 96 papers were found by their titles and whole contents reviewed for relevance in PubMed, Google Scholar, WHO and EMBASE data, and 303 papers in CNKI. Only 25 studies met the inclusion criteria, most of them were published in 5 years.
The characteristics for each study are presented in Table1 The etiologies of CAP were determined by antigen and serological tests, or molecular diagnostic tools (PCR and Real Time-PCR).
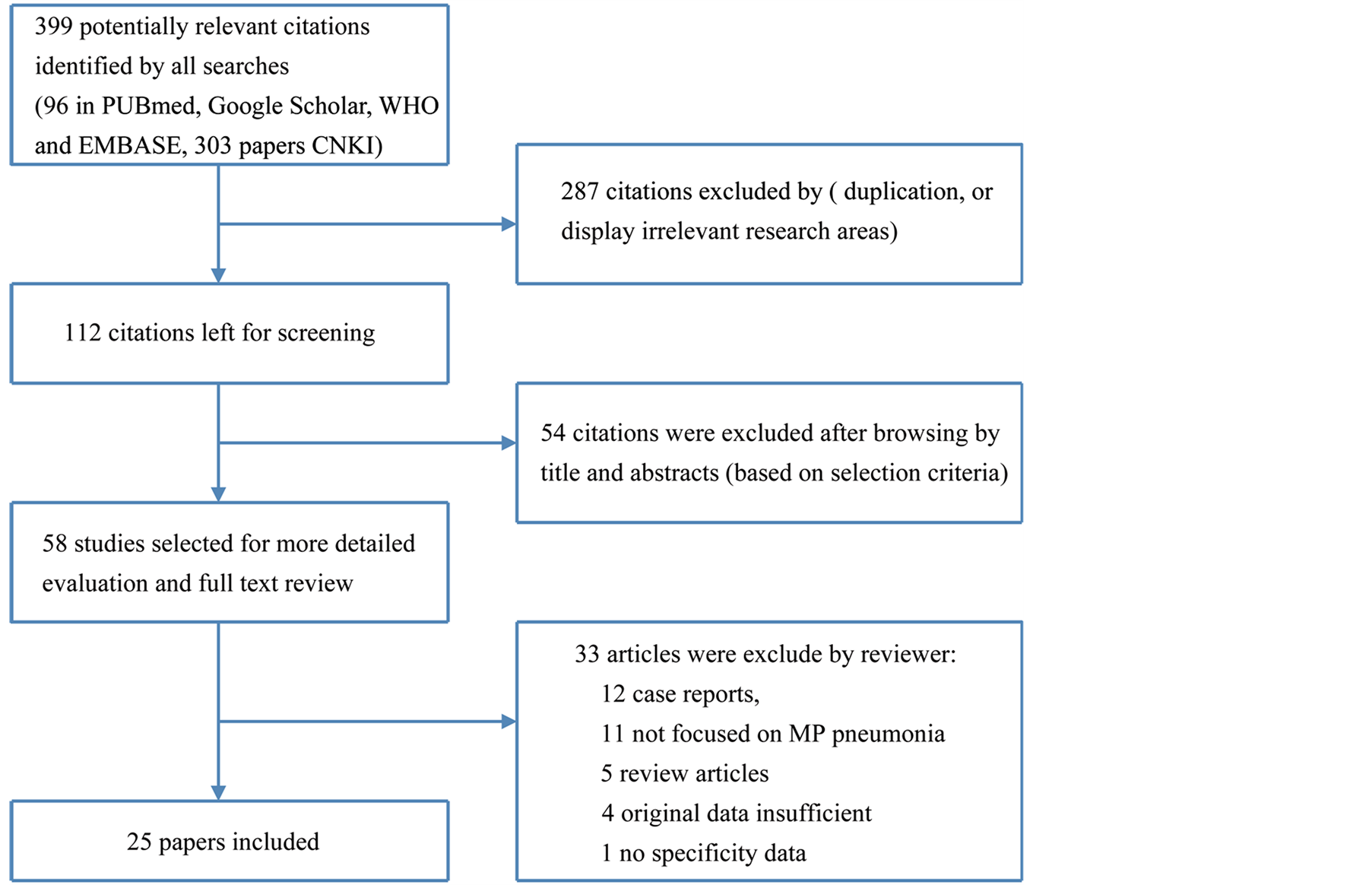
Figure 1. Study screening scheme.
In 11 papers concerned about epidemiology/etiology, the overall incidence of MPP ranged from 7.1% [9] to 54.4% [22] . The incidence seems increased in recent years, particularly in East Asia. Data from several studies showed that the prevalence of MP infection was higher during fall, winter, and spring, and lower in summer. Fever and cough were most frequently identified in clinics, followed by wheezing and other lung abnormalities. Of particular note is the airway mucosal damage, in some severe cases, it is the risk factor for atelectasis and obstructive bronchitis [32] . MPP can cause multi-system infections in children, and may be accompanied with other pathogens. The positive rate of pneumonia diagnosed by X-ray was not significantly different between children with MP infection and those with other pathogen infection [10] . In most cases of MPP, the leukocyte count, neutrophil proportion, CRP, and ESR were normal or only slightly elevated. Drug resistance rate vary from 18.9% [13] to 90% [8] , may contributed to the different test methods and interpretative breakpoints. Gene mutations associated with macrolides resistance were very common. Several point mutations in 23S rRNA have been reported, and different mutations cause different level of resistance to 14-, 15-, and 16-member macrolides. No death case was reported in all studies, but in younger children, the complications are more often to be seen and some of them had severe clinical course [29] [30] .
3. Discussion
Our study findings indicate that pathogens isolated in patients with CAP in China seem to differ from those described from Western countries. Streptococcus pneumoniae remains the most important pathogen in adults of all ages admitted to hospital with CAP [33] , and the fulminant MPP cases were rarely reported in Japan (only 52 fulminant MPP cases were reported between September, 1979 and February, 2010) [34] . In the last ten years, great emphasis has been placed on the role of MP infection with atypical pneumonia in children. The incidence of MP infection in CAP may be higher than previously thought [22] . But in MP infection, it is difficult to set up a criteria list for the “gold standard” to detect acute or remote infections. As to different studies, various etiologic tests have been used. Currently, the laboratory diagnosis of MP infection is mainly based on the serologic or molecular-based testing. Compared with serological index, PCR results seemed to be the most promising direct technology due to its high sensitivity and specificity [35] [36] . There needs an universally agreed-upon gold standard assay for detecting MP now.
*less than 3 years old patients.
According to the results of our study, MPP is very common in present society, but its clinical features and laboratory parameters are not clear and specific. In the majority of investigated cases of MP infections, the leukocyte count, neutrophil proportion, CRP, and ESR were normal or only slightly elevated [10] . Although some minor variations maybe detected, there was no statistically significant of the peripheral leukocyte, CRP, and ESR value between the children with MPP and those with other viral infections. Therefore, the routine laboratory tests are not specific to diagnose children with MP infection. In some severe cases, the airway mucosal damage is the risk factor for atelectasis and obstructive bronchitis, contribute to prolonged pneumonia. This phenomenon has been increasingly recognized by pediatricians in recent years. So airway mucosal damage under bronchofiberscopy may be a promising method to diagnose MPP [32] . In children, MPP may be complicated by plastic bronchitis, even if it did not have severe systemic inflammatory reaction. In present study, we found the presence of fever, cough and wheezing seemed to be peculiar to the diagnosis for MPP. Thus, it may be not possible to predict the occurrence of MPP by depending only on the initial clinical symptoms and common laboratory parameters. MPP can cause multi-system infections in children, and may be accompanied with viral infections, school-age children are more susceptible to this disease, particularly in autumn and winter [18] . So, it is essential for identifying the respiratory infection pathogen. And the antibiotic treatment should be based on the results of etiologic tests.
In present study, the macrolide resistance rates were very high in China, up to 90% [8] . Macrolide resistance in M. pneumoniae is due to mutations in 23S rRNA [37] . Several point mutations in 23S rRNA have been reported, and different mutations cause different level of resistance to 14-, 15-, and 16-member macrolides. Furthermore, a number of adhesion genes, including P1, P30, and P116, have been investigated in the adhesive mechanism of MP and explored for diagnostic purposes [10] . The variety of drug resistance may contribute to different areas. Though the macrolides resistance in MPP is quite high in China, macrolides and cephalosporin antibiotics are still the most common drugs used in the treatment of MPP in children. The reason may be that MPP always have concurrent infections. The impact of the resistance to macrolides on the efficacy of treatment with macrolides is thus needed to be investigated.
As in Zhang’s study, young age and underlying congenital heart disease were risk factor with severe CAP for PICU support, among them 11% were severe type of MPP [17] . And long fever course, MOD, large pleural effusion, located right upper lung were the risk factor for severe complications [25] . Infantile patients may have more rapid clinical progression and complications [29] . It has been proposed that cell-mediated immunity play an important role in the progress of MP infection [38] . Thus immune suppressive therapy would be useful. Because corticosteroids have roles of immune regulation and anti-inflammation, it was reported that corticosteroids could improve symptoms and pulmonary lesion rapidly in children with MPP [39] [40] . However, there was no evidence-based report about appropriate use of cortical steroid, in particular, those of dosage, administration route, or duration of treatment [16] . All these reports were cases based and the severity of diseases were different, further controlled double-bland studies to define the optimal methods for corticosteroid use in MP may be necessary.
The results of our study could contribute to better understanding of the epidemiology, clinical, and laboratory characteristics of MPP in Chinese pediatric population. Future studies are encouraged to improve the lab techniques for detecting MP rapidly and specifically, and more multi-center double blind control studies on treatment for MP infection.
Acknowledgements
This study was supported by the grants from the State Key Clinical Department (of Pediatric Lung Diseases 2012) and BCH Young Investigator Program, BCHYIPA-2013-03. We also appreciate the efforts of our colleagues in respiratory medicine department of State Clinical Medical Research Center.
References
- Himmelreich, R., Hilbert, H., Plagens, H., Pirkl, E., Li, B.C. and Herrmann, R. (1996) Complete Sequence Analysis of the Genome of the Bacterium Mycoplasma pneumoniae. Nucleic Acids Research, 24, 4420-4449. http://dx.doi.org/10.1093/nar/24.22.4420
- Zhao, H., Li, S., Cao, L., Yuan, Y., Xue, G., Feng, Y., Yan, C., Wang, L., Fan, Z. and Sun, H. (2014) Surveillance of Mycoplasma pneumoniae Infection among Children in Beijing from 2007 to 2012. Chinese Medical Journal, 127, 1244-1248.
- Ngeow, Y.F., Suwanjutha, S., Chantarojanasriri,
T., Wang, F., Saniel, M., Alejandria, M., et al. (2005) An Asian Study on the Prevalence
of Atypical Respiratory Pathogens in Community-Acquired Pneumonia. International
Journal of Infectious Diseases, 9, 144-153.
http://dx.doi.org/10.1016/j.ijid.2004.06.006 - Nour, M., Trabelsi, A., Maatouk, N. and Hammami, M. (2005) Amplification of P1 and 16S rRNA Genes by Nested PCR for Detection of Mycoplasma pneumoniae in Paediatric Patients. Pathologie Biologie, 53, 9-14. http://dx.doi.org/10.1016/j.patbio.2004.01.002
- Rudan, I., El Arifeen, S., Bhutta, Z.A., Black, R.E., Brooks, A., et al. (2011) Setting Research Priorities to Reduce Global Mortality from Childhood Pneumonia by 2015. PLoS Medicine, 8, Article ID: e1001099. http://dx.doi.org/10.1371/journal.pmed.1001099
- World Health Organization -Western Pacific Region Library.
- World Health Organization -Regional Office for Southe-East Asia Library.
- Ma, Z., Zheng, Y., Deng, J., Ma, X. and Liu, H. (2010) Characterization of Macrolide Resistance in Mycoplasma pneumoniae Isolated from Children in Shanghai, China. Diagnostic Microbiology and Infectious Disease, 67, 355-358. http://dx.doi.org/10.1016/j.diagmicrobio.2010.03.004
- Liu, G., Talkington,
D.F., Fields, B.S., Levine, O.S., Yang, Y. and Tondella, M.L. (2005) Chlamydia Pneumoniae
and Mycoplasma pneumoniae in Young Children from China with Community-Acquired Pneumonia.
Diagnostic Microbiology and Infectious Disease, 52, 7-14.
http://dx.doi.org/10.1016/j.diagmicrobio.2005.01.005 - He, X.Y., Wang, X.B., Zhang, R., Yuan, Z.J., Tan, J.J., Peng, B., Huang, Y., Liu, E.M., Fu, Z., Bao, L.M. and Zou, L. (2013) Investigation of Mycoplasma pneumoniae Infection in Pediatric Population from 12,025 Cases with Respiratory Infection. Diagnostic Microbiology and Infectious Disease, 75, 22-27.
- Cao, B., Zhao, C.J., Yin, Y.D., Zhao, F., Song, S.F., Bai, L., Zhang, J.Z., Liu, Y.M., Zhang, Y.Y., Wang, H. and Wang, C. (2010) High Prevalence of Macrolide Resistance in Mycoplasma pneumoniae Isolates from Adult and Adolescent Patients with Respiratory Tract Infection in China. Clinical Infectious Diseases, 51, 189-194. http://dx.doi.org/10.1086/653535
- Ou, Z.-Y., Zhou, R., Wang, F.-H., Lu, J.-P.,
Xia, J.-Q., Xia, H.-M., Zhang, J.-T., Gong, S.-T., Deng, L., Wu, Z.-H. and Zeng,
Q.-Y. (2008) Retrospective Analysis of Mycoplasma pneumoniae Infection in Pediatric
Fatal Pneumonia in Guangzhou, South China. Clinical Pediatrics, 47, 791-796.
http://dx.doi.org/10.1177/0009922808318339 - Yang, A.M., Song, J.H., Huang, R., Jin, S.J. and Yang, P. (2013) Mycoplasma pneumoniae Infection and Drug Resistance in Children: An Analysis of 1026 Cases. Chinese Journal of Contemporary Pediatrics, 15, 522-525.
- Xin, D., Mi, Z., Han, X., Qin, L.,
Li, J., Wei, T., Chen, X., Ma, S., Hou, A., Li, G. and Shi, D. (2009) Molecular
Mechanisms of Macrolide Resistance in Clinical Isolates of Mycoplasma pneumoniae
from China. Antimicrobial Agents and Chemotherapy, 53, 2158-2159.
http://dx.doi.org/10.1128/AAC.01563-08 - Jiang, Y., Liu, X.J., Qin, X.G., Dong, Y.Q., Dong, X.P. and Xin, D.L. (2013) Drug Resistance of MP and Its Mechanism: A Study of Children in Beijing Distinct in 2011. Chinese Journal of General Practitioners, 16, 3778-3782.
- Lu, A., Wang, L., Zhang, X. and Zhang, M. (2011) Combined Treatment for Child Refractory Mycoplasma pneumoniae Pneumonia with Ciprofloxacin and Glucocorticoid. Pediatric Pulmonology, 46, 1093-1097. http://dx.doi.org/10.1002/ppul.21481
- Zhang, Q., Guo, Z., Bai, Z. and MacDonald, N.E. (2013) A 4 Year Prospective Study to Determine Risk Factors for Severe Community Acquired Pneumonia in Children in Southern China. Pediatric Pulmonology, 48, 390-397. http://dx.doi.org/10.1002/ppul.22608
- Zhao, H., Li, S., Cao, L., Yuan, Y., Xue, G., Feng, Y., Yan, C., Wang, L., Fan, Z. and Sun, H. (2014) Surveillance of Mycoplasma pneumoniae Infection among Children in Beijing from 2007 to 2012. Chinese Medical Journal (English Edition), 127, 1244-1248.
- Cui, S.-N., GU, L. and He, F. (2012) Clinical Observation on Efficacy of Azithromycin Combined with Ceftriaxone Sodium in the Treatment of Refractory Mycoplasma pneumoniae Pneumonia in Children. World Clinical Drugs, 33, 743-747.
- Wu, X.-X., Shen, J. and Zheng, Y.-P. (2013) Observation on Efficacy and Safety of Azithromycin in the Treatment of Mycoplasma pneumonia in Children. Chinese Journal of Nonocomiology, 23, 5798-5800.
- Wu, X.-J. (2014) Clinical Observation of 68 Cases of Azithromycin Injection Treatment of Mycoplasma pneumonia in Children. Chinese Journal of Modern Drug Application, 8, 160-161.
- Zhang, T., Wang, B., Wang, H.Q., Tang, Y.P., Liu, M.L., Peng, S.M., et al. (2014) Correlation between Drug Resistance and Clinical Treatment of Mycoplasma pneumoniae. Chinese Journal of Obstetrics Gynecology and Pediatrics (Electronic Edition), 10, 29-40.
- Sun, X.-Q. (2013) Analysis of Mycoplasma pneumonia in Children and Clinical Features of 216 Cases with Pulmonary Complications. A Guide to Chinese Medicine, 11, 437-438.
- Zhang, Y.-M., Liu, X.-Y. and Jiang, Z.-F. (2010) One-Year Follow-Up Study for Mycoplasma pneumoniae Pneumonia with Pulmonary Atelectasis Complications. Chinese Journal of Practical Pediatrics, 25, 143-146.
- Gao, H., Luo, Z.-X., Luo, J., Xu X.-J., Liu, E.-M. and Fu, Z. (2013) Clinical Risk Factor for Children with Mycoplasma pneumoniae Pneumonia Sequelae. Chongqing Medical University, 38, 165-167.
- Tan, Z.-T. (2013) Study on the Clinical Manifestation and Pathogenesis of Mycoplasma pneumoniae Pneumonia in Children. Maternal and Child Health Care of China, 28, 5467-5468.
- Ke, L.-Q., Wang, F.-M., Li, Y.-J. and Luo, Y.-C. (2013) Epidemiological Characteristics of Mycoplasma pneumoniae Pneumonia in Children. Chinese Journal of Contemporary Pediatrics, 15, 33-36.
- Xu, Y.-C., Zhu, L.-J., Xu, D., Tao, X.-F., Li, S.-X., Tang, L.-F. and Chen, Z.-M. (2011) Epidemiological Characteristics and Meteorological Factors of Childhood Mycoplasma pneumoniae Pneumonia in Hangzhou. World Journal of Pediatrics, 7, 240-244. http://dx.doi.org/10.1007/s12519-011-0318-0
- Liu, X.-Yu., Wei, Z.-Q., Wang, D.-D. and Suo, J.-Y. (2013) Analysis of 46 Cases of Infant Pneumonia Mycoplasma pneumonia. People’s Military Surgeon, 56, 1328-1329.
- Ren, L.-X., Dong, H.-Q., Ning, J., Guo, W. and Wan, L.-Y. (2013) Analysis and Pulmonary Function and Fiberoptic Bronchoscopy Clinical and Imaging Features of Mycoplasma pneumonia in Infants. Guangdong Medical Journal, 34, 2686-2688.
- Shi, X., Yu, F. and Huang, Q.-L. (2014) Clinical Manifestation of Children with Mycoplasma pneumonia. Chinese Journal of Nosocomiology, 206-210.
- Jiao, A.X., Rao, X.C., Jiang, Q.B., Ma, Y.Y., Pan, Y.N., Hu, Y.H. and Liu, X.C. (2010) Comparative Study of Persistent and Non Persistent Pneumonia Mycoplasma pneumonia in Children with Airway Mucosal Injury. Chinese Journal of Evidence-Based Pediatrics, 3, 111-115.
- Lim, W.S., Macfarlane, J.T., Boswell, T.C., Harrison, T.G., Rose, D., et al. (2001) Study of Community Acquired Pneumonia Aetiology (SCAPA) in Adults Admitted to Hospital: Implications for Management Guidelines. Thorax, 56, 296-301. http://dx.doi.org/10.1136/thorax.56.4.296
- Izumikawa, K., Izumikawa, K., Takazono, T., Kosai, K., Morinaga, Y., Nakamura, S., et al. (2014) Clinical Features, Risk Factors and Treatment of Fulminant Mycoplasma pneumoniae Pneumonia: A Review of the Japanese Literature. Journal of Infection and Chemotherapy, 20, 181-185. http://dx.doi.org/10.1016/j.jiac.2013.09.009
- Loens, K., Beck, T., Ursi, D., Overdijk, M., Sillekens, P., Goossens, H., et al. (2008) Development of Real-Time Multiplex Nucleic Acid Sequence-Based Amplification for Detection of Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Legionella spp. in Respiratory Specimens. Journal of Clinical Microbiology, 46, 185-191. http://dx.doi.org/10.1128/JCM.00447-07
- Thurman, K.A., Warner, A.K., Cowart, K.C., Benitez, A.J. and Winchell, J.M. (2011) Detection of Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella spp. in Clinical Specimens Using a Single-Tube Multiplex Real-Time PCR Assay. Diagnostic Microbiology and Infectious Disease, 70, 1-9. http://dx.doi.org/10.1016/j.diagmicrobio.2010.11.014
- Waites, K.B., Balish,
M.F. and Atkinson, T.P. (2008) New Insights into the Pathogenesis and Detection
of Mycoplasma pneumoniae Infections. Future Microbiology, 3, 635-648.
http://dx.doi.org/10.2217/17460913.3.6.635 - Radisic, M., Torn, A., Gutierrez, P., Defranchi, H.A. and Pardo, P. (2000) Severe Acute Lung Injury Caused by Mycoplasma pneumoniae: Potential Role for Steroid Pulses in Treatment. Clinical Infectious Diseases, 31, 1507-1511. http://dx.doi.org/10.1086/317498
- Tamura, A., Matsubara, K., Tanaka, T., Nigami, H., Yura, K. and Fukaya, T. (2008) Methylprednisolone Pulse Therapy for Refractory Mycoplasma pneumoniae Pneumonia in Children. Journal of Infection, 57, 223-228. http://dx.doi.org/10.1016/j.jinf.2008.06.012
- Shen, Y.L., Zhang, J., Hu, Y.H. and Shen, K.L. (2013) Combination Therapy With Immune-Modulators and Moxifloxacin on Fulminant Macrolide-Resistant Mycoplasma pneumoniae Infection: A Case Report. Pediatric Pulmonology, 48, 519-522.
Note List about the Abbreviations
MP: Mycoplasma pneumoniae;
MPP: Mycoplasma pneumoniae pneumonia;
CAP: Community acquired pneumonia;
CNKI: China Knowledge Resource Integrated Database;
TB: Tubercule bacillus;
CRP: C-reactive protein;
ESR: Erythrocyte sedimentation rate;
rRNA: ribosomal ribonucleic acid.
NOTES

*Corresponding author.


