Open Journal of Thoracic Surgery
Vol.4 No.1(2014), Article ID:43412,4 pages DOI:10.4236/ojts.2014.41002
Glomus Tumors of the Lung: Diagnostic Considerations and Treatment
Joshil V. Lodhia1, Thomas D. Christensen1,2, Simon E. Trotter3, Ehab S. Bishay1
1Department of Thoracic Surgery, Heart of England Foundation Trust, Birmingham, UK
2Department of Cardiothoracic and Vascular Surgery & Institute of Clinical Medicine, Aarhus University Hospital, Aarhus, Denmark
3Department of Histopathology, Heart of England Foundation Trust, Birmingham, UK
Email: joshil.lodhia@nhs.net
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 29 December 2013; revised 29 January 2014; accepted 7 February 2014
ABSTRACT
Glomus tumors derive from the glomus cell around arteriovenous anastomosis. These are rare tumors and when found are most common in the deep dermis of the extremities. In rarer cases still they have been reported to be found in the lung. These are most commonly incidental findings of solitary lesions of the lung with a pre-operative differential diagnosis of non-small cell carcinomas and carcinoids. Due to the rare nature of these tumors, they are rarely considered in the differential diagnosis and are also often misdiagnosed at the time of frozen section. We present three cases of glomus tumors of the lung with emphasis on the consideration of the method of diagnosis, histological findings and management.
Keywords:Lung Cancer; Glomus Tumor; Surgical Therapy

1. Introduction
Glomus tumors are benign tumors arising from arteriovenous anastomoses which are frequently found in the deep dermis of the extremities. They are very rare tumors comprising of less than 2% of all soft tissue lesions [1] . Outside the common sites, they can occur in the gastrointestinal tract, mediastinum, bone, adrenal glands, central nervous system, uterus and vagina. Glomus tumors can be categorized into benign or malignant. The benign subtypes are solid glomus tumors [2] .
It has been reported to be found in the lung however these are very rare. Ariizumi et al. presented a case of glomus tumor of the lung and summarized the previous 32 cases described in literature [3] . We add to this by further describing the preoperative findings, such as positron emission tomography (PET) findings, as these have not previously been discussed. We present three cases of glomus tumors of the lung with respect to diagnosis, histology findings and management.
2. Case Reports
2.1. Case One
A 62-year-old male with an incidental finding of a 1.8 cm left lower lobe lesion. This lesion was noted to be PET negative. He is a fit lifelong non-smoker with good pre-operative lung function. He underwent an uncomplicated left sided video assisted wedge resection during which the frozen section suggested carcinoid with clear margins. Due to this reason he did not undergo a lobectomy. Formal histology revealed a 15 mm nodule composed of spindle cell proliferation with oval band nuclei and indistinct cytoplasmic borders (Figure 1). It was negative for cytokeratin and neuroendocrine markers. The tumor did however stain with smooth muscle actin immunoreagent and vimentin (Figure 2). The microscopic findings were in keeping with a glomus tumor. Following the procedure he was followed up in an outpatient clinic setting and informed that no further treatment was required for this lesion.
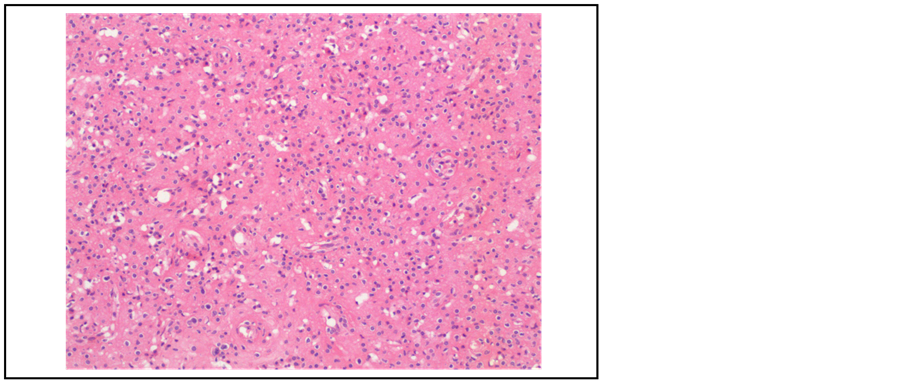
Figure 1. Hematoxylin and eosin stain (×10) of case one demonstrating spindle cells with oval band nuclei and indistinct cytoplasmic borders.
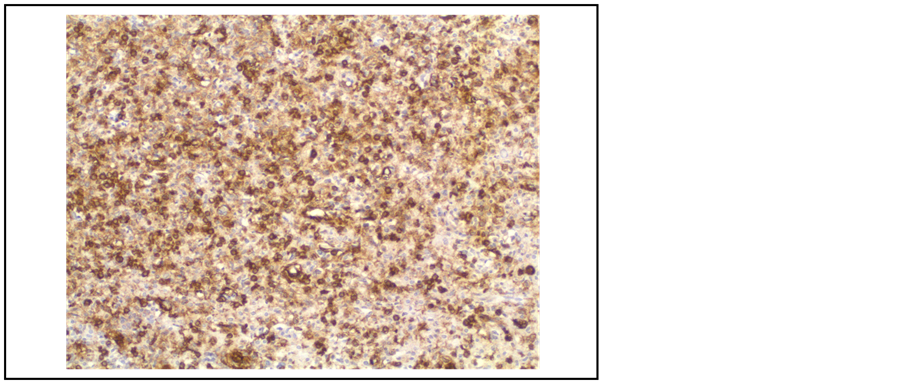
Figure 2. Immunochemistry of case one demonstrating the diffuse antibody recognition of smooth muscle isoform of actin.
2.2. Case Two
A 51-year-old male who was investigated for a cough was noted to have a right upper lobe lesion. PET scan revealed this lesion to be mildly active (SUV max 2.9). He is an ex-smoker of 15 pack years. He underwent an uncomplicated wedge excision of the right upper lobe. The frozen section suggested a non-small cell lung cancer with clear margins. Importantly it was noted to be low grade and therefore it was decided not to proceed to a lobectomy. Formal histology revealed no necrosis or mitotic activity. It was positive for smooth muscle actin while cytokeratin, desmin and the neuroendocrine markers were negative. It was classed as a glomus tumor. He was followed up in outpatient clinic with no further treatment needed.
2.3. Case Three
A 64-year-old male presented with an incidental finding of a nodule in the right upper lobe. He is an ex-smoker with a smoking history of 40 pack years. He underwent a right thoracotomy and frozen section which suggested a carcinoid however could not rule out the possibility of an invasive carcinoma. An upper lobectomy was therefore carried out. Formal histology confirmed the lesion was composed of a monotonous proliferation of round to oval cells, which were negative for cytokeratin, S100 and neuroendocrine markers. The cells were strongly reactive for smooth muscle actin. These findings were in keeping with a glomus tumor. He was followed up in an outpatient clinic and no further treatment was required.
3. Discussion
We have presented three cases of the rare glomus tumor in the lung, where the greatest challenge was obtaining the diagnosis and hence performing the most appropriate resection. Due to their paucity, glomus tumors are rarely included in the differential diagnosis of other lung malignancies. These glomus tumors are challenging with respect to their histopathological diagnosis and therefore treatment is varied.
These nodules are often found incidentally on a CXR which leads to further investigation by the means of a CT and PET scan. Prior to surgery the most common differential diagnoses for these lesions are non-small cell lung cancers. They are investigated and treated as such. The group of patients that have the glomus tumors is predominantly younger and may not have the traditional risk factors in terms of smoking history [3] . The CT scan often reveal a solitary lesion and the PET scan shows low or no metabolic activity. No cases have associated mediastinal lymphadenopathy or metastasis and therefore they often proceed to surgical resection.
At frozen section these tumors are felt to be non-small cell lung cancers or carcinoid. Frozen section in two of our cases suggested a carcinoid and was therefore only subjected to a limited resection such as a wedge resection. The third case underwent a lobectomy due to frozen section findings.
Biopsies of this lesion including at the point of frozen section often suggest carcinoid, adenoma or haemangiomas. It is only at the point of immunohistochemistry that the differential diagnoses are excluded. The formal histopathological investigations reveal features of smooth muscle, importantly with no necrosis or mitotic activity (Figure 1). Immunohistochemistry shows staining for smooth muscle actin and vimentin (Figure 2). They are negative for TTF-1, cytokeratins, desmin and neuroendocrine markers. Carcinoid tumors are positive for cytokeratin and neuroendocrine markers and sclerosing haemangiomas are positive for TTF-1, cytokeratin and surfactant apoprotein A.
Following the operation the diagnosis is often confirmed via formal histopathology and immunohistochemistry. Solid glomus tumors have not been suggested to spread to mediastinal lymph nodes or recur following resection therefore we suggest no adjuvant therapy nor long term follow up.
4. Summary
In summary, glomus tumors of the lung are very rare, often seen in younger, non-smoking patients encountered as an incidental finding. A small nodule is found in the CT scan, and the PET scan is usually negative. Diagnosis is not accurate in either biopsies or frozen section, so they are treated as their differential diagnosis. Treatment is accordingly resection. The diagnosis is first established with the formal histopathological investigation, and no further treatment nor follow-up is needed.
Conflicts of Interest Statement
Thomas D. Christensen has done lectures supported by AstraZeneca, Boehringer Ingelheim, Pfizer, and Takeda.
References
- Shugart, R.R., Soule, E.H. and Johnson, E.W. (1663) Glomus Tumour. Surgery, Gynaecology and Obstetrics, 117, 334-340
- Hohenforst, W., Woitow, M., Zarogoulidis, P., Machairiotis, N., Gschwendtner, A., Huang H., et al. (2012) Glomus Tumour in the Lung Parenchyma. Journal of Thoracic Disease, 4, 663-666.
- Ariizumi, Y., Koisumi, H., Hoshikawa, M., Shinmyo, T., Ando, K., Mochizuki, A., et al. (2012) A Primary Pulmonary Glomus Tumour: A Case Report and Review of Literature. Case Reports in Pathology, 2012, Article ID: 782304.

