Open Journal of Orthopedics
Vol.3 No.3(2013), Article ID:34519,6 pages DOI:10.4236/ojo.2013.33031
Treatment of Bilateral Recurrent Dislocation of Hip Prosthesis with Malpositioned Well-Fixed Shell: A Case Report*
![]()
Orthopedics Department of Coimbra, University Hospital Center, Faculty of Medicine, University of Coimbra, Coimbra, Portugal.
Email: #fernandojudas@gmail.com, luismaxfigueiredo@gmail.com, francisco.m.lucas@gmail.com
Copyright © 2013 Fernando Judas et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received May 5th, 2013; revised June 5th, 2013; accepted June 20th, 2013
Keywords: Hip Prosthesis; Bilateral Recurrent Dislocation; Malpositioned Well-Fixed Shell; Surgical Treatment
ABSTRACT
Dislocations of total hip prostheses cause pain and patient dissatisfaction. Recurrent dislocations are difficult to treat mainly when the acetabular metal shell is well-fixed. The purpose of this article was to describe the surgical technique used for the treatment of a bilateral recurrent posterior dislocation after a cementless total hip prosthesis, caused by excessive inclination of acetabular components, in a 72-year-old patient. On both sides, acetabular metal shell, porouscoated, was well-fixed. Revision of the entire acetabular component could be an appropriate therapeutic option because it was malpositioned. Nevertheless, a conservative operation was performed. The metal shell was left in situ and the preexisting polyethylene liner was removed and replaced by a new undersized cross-linked polyethylene liner, then, cemented into the shell and properly oriented. An acetabular cemented augmentation reinforced by 3 cortical screws was associated with the reconstruction. This report suggests that cementation of new liner into a malpositioned wellfixed metal shell associated with an acetabular cemented augmentation is a simple and safe technique for the management of recurrent hip dislocation, for elderly patients in which it is advisable to avoid a major revision hip surgery by medical comorbidities. Nonetheless, further studies with medium-and long-term follow-up are needed to validate this technique.
1. Introduction
Total hip arthroplasty has become one of the most successful interventions in reconstructive orthopaedic surgery. However, dislocation and prosthetic loosening remain the two most common complications of total hip arthroplasty (THA). According to the registers, dislocation occurs after 0.3% to 10% of primary total hip arthroplasties and after up to 28% of revision total hip arthroplasties [1,2].
Dislocations are cause for pain and dissatisfaction for patients. Several factors may contribute to the risk of dislocation, including malpositioning of one or both prosthetic components, insufficient or weak abductor muscles, inadequate soft-tissue tension, presence of an impingement, incongruence of head and acetabular liner as well as combinations of these factors [3,4]. Component malpositioning and abductor insufficiency are two of the most important recognized causes of recurrent dislocation [5-7].
The diagnosis of dislocation after THA is almost always made by clinical examination and confirmed by radiographic study. Computed tomography is the only method to determine the three-dimensional relationship of the components [8]. The mechanism of the dislocation can be verified by a dynamic fluoroscopic examination.
Most dislocations occur within the first 3 months and are single episodes that can be managed nonoperatively. Late dislocations are more likely to become recurrent and require surgical intervention in order to identify and to correct specific causes for instability [3,9]. When the etiology of the dislocation is multifactorial or unknown, the best surgical technique with which to address it is often a challenging problem for the surgeon.
The surgical options available for treatment of recurent dislocation consist of component revision, modular component exchange, bipolar arthroplasty, use of a larger femoral head, soft-tissue reinforcement, and advancement of the greater trochanter [10-14]. As a last resort, a constrained socket design can be used in which the femoral head is locked into the socket [15]. Removal of the prosthetics components without further reconstruction is another final option and can be indicated in individuals’ cases, noncompliant and elderly debilitated patients.
The purpose of this article was to describe the surgical technique used for the treatment of a bilateral recurrent posterior dislocation after a cementless total hip prosthesis, caused by a malpositioned acetabular component.
2. Case Report
A 72-year-old man had a history of bilateral recurrent prosthesis dislocation. He had a bilateral cementless THA, with a modular metal-on-polyethylene bearing surface. The right THA was implanted twelve years ago and the left THA ten years ago in another orthopaedic institution.
After being asymptomatic for three years, recurrent dislocations of the right THA were reported and treated nonoperatively (about ten dislocations). In the other hip six dislocations were noted (Figure 1).
The patient was observed in our department in October 2011. The medical history included diabetes mellitus type II, hypertension, hyperlipidemia, chronic obstructive pulmonary disease, surgical interventions to cervical and lumbar spine by vertebral stenosis, and had a Body Mass

Figure 1. Anteroposterior radiograph of the left hip of a 72-year-old man, made ten years after the initial procedure, showing a posterosuperior dislocation caused by an excessive inclination of the socket. The patient had a history of bilateral recurrent prosthesis dislocation.
Index of 30.
In order to prevent more dislocations of the prostheses, a bilateral surgical intervention was performed, in two different operative times. The first operation includes the right hip and six months later a similar surgical procedure was performed into the left hip.
Apparently, there was a predisposing dislocation mechanism, preoperative roentgenogram showed augmentation of the inclination angle of the acetabular component in both prosthesis, 56 degrees in the right hip and 60 degrees in the left, and absence of radiolucent lines at the bone-socket interfaces (Figure 2). The femoral components were stable. Revision of the acetabular component was the aim of the operation.
Hips were exposed through a standard posterolateral approach with the patient in the lateral decubitus position, under general anesthesia. Intraoperatively a posterior and superior hip instability was identified as resulting from the combined movements of internal rotation and adduction.
The original polyethylene liner was pried from the metal backing with a curved osteotome and a new liner was cemented into the shell. The shell was further tested to confirm stability by applying pressure to the rim and pulling on the shell with pliers. It was well-fixed showing absence of movement at the bone-shell interface.
A metal screw was removed at the right shell and all screw holes were enlarged with a flexible drill, for cement interdigitation and a better liner fixation. We selected a cross-linked polyethylene liner that was 4 mm smaller than the inner diameter of the existing shell. The back surface of the polyethylene liner was roughened with use of a small burr to ensure the stable fixation of the liner and metal shell.
As the liner must be reoriented with a new inclination and anteversion, we proceeded to the augmentation of the posterior wall of the acetabulum. Then, 3 cortical screws

Figure 2. Both acetabular components were well-fixed. An excessive inclination angles of the acetabular components can be observed, 56 degrees in the right hip and 60 degrees in the left.
(4.5 mm) were implanted in the rim of the acetabulum, about one centimeter from the rim and were paralleled superiorly to the ilium. The heads of the screws protrude about 1.5 cm beyond the acetabular bone (Figure 3).
The inside area of the shell was cleansed and dried. The bone cement was prepared, and when it was doughy in consistency, it was inserted into the shell and placed over the screws, thus connecting and burying them in the cement mass. Then, the liner was cemented into the existing shell with about 40 degrees of inclination and 20 degrees of anteversion. A continuous cement mass connected the upper quadrant of the liner surface and the head screws (Figure 4), and excess cement was removed. The existing 28 mm femoral head was replaced for a new one with the same size.
Once the cement sets, movement of the prosthesis was checked in all directions to confirm that it is stable. In order to improve hip stability, posterior neo-capsule flap and the remaining short external rotators were approximated to the posterior aspect of the abductors and the greater trochanter, using non-absorbable transosseous sutures passed through trochanteric drill holes. In addition, two non-absorbable sutures anchored within the polymethylmethacrylate cement mass were also attached at the bone trochanter. The wound was closed in the standard fashion over closed suction drains.
Postoperatively no complications occurred such as deep or superficial infection or deep vein thrombosis and the patient was recommended to bear weight on the joint as soon as possible, with crutches for the first six weeks. No further dislocation was noted. At the last clinical control, nineteen months of follow-up for the right hip and thirteen months for the left hip, the anteroposterior radiograph showed stability of the bilateral acetabular reconstruction (Figure 5), and the patient was satisfied

Figure 3. Intraoperative image of the acetabular reconstruction. The original polyethylene liner was removed and 3 cortical screws (4.5 mm) were implanted in the rim of the acetabulum. The existing shell was not replaced.
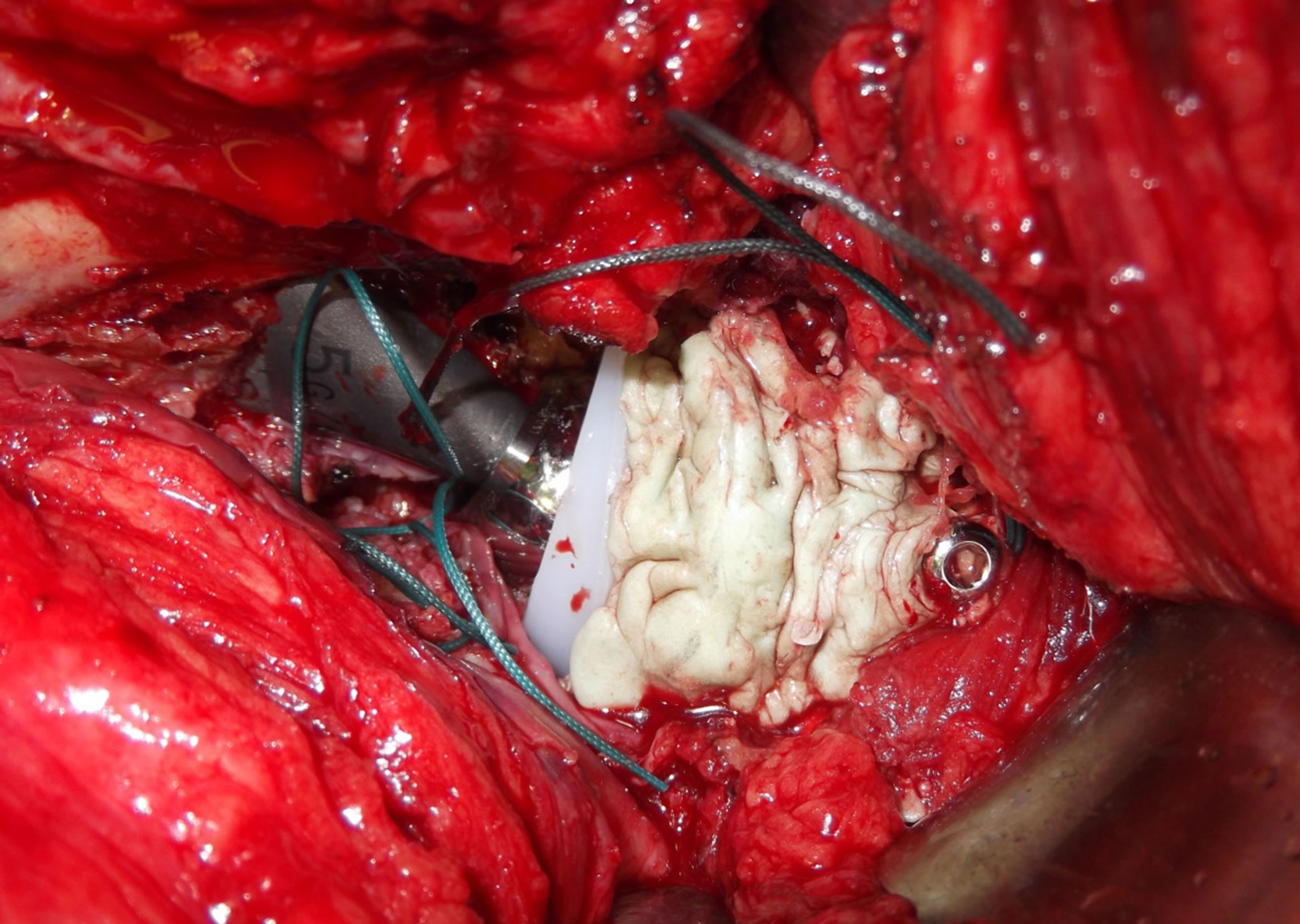
Figure 4. A new undersized cross-linked polyethylene liner was cemented into the shell and properly oriented, about 40 degrees of inclination and 20 degrees of anteversion. A continuous cement mass connected the upper quadrant of the liner surface and the head screws.
with the result of the operations.
3. Discussion
Recurrent instability is a complex problem with multifaceted etiology that requires extensive preoperative planning and availability of multiple surgical options [7]. Despite all of the advances in THA, dislocations still occur and are difficult to treat. Achieving proper acetabular component placement is challenging [16]. In the case an excessive inclination of the acetabular component in both sides was identified, that originated numerous episodes of hip dislocations. Revision of the entire acetabular component could be an appropriate therapeutic option. Nevertheless, we believed that the major problem of the management of this situation was the osseointegration of the acetabular component and the patient condition.
When the acetabular shell orientation is acceptable cementing a new polyethylene liner into a well-fixed metal-backed component is usually a straightforward procedure, and a good option for revision hip arthroplasty. It is useful when a modular polyethylene liner is not available or when the locking mechanism is compromised [17,18].
This technique is not recommended in cases of instability, owing to a high dislocation rate [7,19,20]. The use of a larger femoral head and polyethylene cup in revision surgery for patients with a malpositioned acetabular component is also not recommended [12]. The acetabular shell should be removed if is malpositioned. Revision of the malpositioned component is perhaps the most effective type of surgical intervention in the treatment of recurrent dislocation [6,19]. However, the removal of well-fixed cementless acetabular shell can be

Figure 5. Postoperative radiograph showing the bilateral acetabular reconstruction. An acetabular augmentation (“butée”) composed by a posterosuperior wall of bone cement reinforced by cortical metal screws was created to augment the strength of the surgical reconstruction and to prevent dislocation.
associated with bone loss, bone fracture and bleeding. Normally, it is a demanding operation, time consuming, and requires caution to limit the amount of host bone destruction [19,21,22].
These cases place the surgeon in an operative dilemma. An alternative conservative procedure that minimizes insult is extremely attractive, mainly in the elderly patient. With this aim, orthopaedic surgeons have used superolateral acetabular bone grafting, metallic and cemented acetabular augmentation devices, cemented acetabular augmentation and for cemented acetabular components, segments from an acetabular cup upturned and screwed to the existing cup to contain the femoral head [23-26].
The patient was 72-year-old and comorbidities and for that we used a conservative surgical technique. In both hips the metal shell was maintained, preexisting polyethylene liner was removed and replaced by a new undersized cross-linked polyethylene line with an appropriate orientation. The liner was cemented into the shell.
The concept of cementing a polyethylene liner into a metal shell is not a new one. This technique also has been used in hips with acetabular cages or reconstruction rings and has been associated with a very low dissociaption rate [27,28].
On the basis of our surgical experience with acetabular anti-protrusio cages and acetabular reconstruction rings, dislocation can be avoided by orienting the liner independently of the position of the cage or ring. If the liner is a little uncovered superiorly a buttress of cement is created between the metal implant and the liner.
Similarly, cementing a liner with a correct position in a malpositioned metal acetabular shell leads to uncovered surface of the polyethylene liner, to a buttress of cement and to a mechanical weakness of the reconstruction. The liner is cemented into an eccentric position. With the purpose of augment the strength of the surgical reconstruction and to prevent also dislocation, an acetabular augmentation (“butée”) composed by a posterosuperior wall of bone cement reinforced by 3 cortical metal screws was created.
In addition, closure of the articular space was performed. A good repair of the neo-capsule and remaining short external rotators may reduce the risk of early hip dislocation after a posterior approach. Intraoperatively satisfactory stability of the prostheses movements in all directions was confirmed.
During the last five years we have used these generic surgical principles for the treatment of many dislocations and instabilities of hip prostheses in elderly patients, with satisfactory results.
To our knowledge the use of these technical principles for the treatment of recurrent dislocation of THP, with a malposioned well-fixed metal shell were not well referenced in the orthopaedic literature. Usually, a total revision of the acetabular component is the procedure mostly recommended.
The method we have described is an option that should be considered especially for elderly patients, in which it is advisable to avoid a major revision hip surgery by medical comorbidities. This is a simple, reproducible, non-costly, non-timing consuming and safe technique for the management of a recurrent hip dislocation, caused by malpositioned well-fixed acetabular shell. The risks of surgical complications are minimized. Nonetheless, further follow-up is required to determine if it remains a viable option in mediumand long-term.
4. Conclusion
When recurrent dislocation is originated by malposition of a well-fixed acetabular shell, cementing a new liner with appropriate orientation associated with an acetabular augmentation composed by a posterosuperior wall of bone cement reinforced with cortical metal screws can be a satisfactory option in elderly patients. We believe that this technique provides a straightforward alternative to a complete acetabular revision.
5. Author’s Contributions
The lead author on this paper is F. Judas. He is an experienced hip surgeon, Chief of Service, Professor of the Faculty of Medicine, University of Coimbra, and he works in the Orthopedics Department of Coimbra University Hospital Center. The other authors are also experienced hip surgeons, Graduated Assistants and they works in the Orthopedics Department of Coimbra University Hospital Center. They have participated in the surgery and contributed to the manuscript preparation. All the authors have read and approved the final manuscript. All authors participated fully in the conception, development, and creation of this paper. All authors read and approved the final version of the paper.
6. Acknowledgements
The authors thank J. Faisca, and C. Mariano, for their assistance in this work.
REFERENCES
- N. S. Eftekhar, “Dislocation and Instability Complicating Low Friction Arthroplasty of the Hip Joint,” Clinical Orthopaedics, Vol. 121, 1976, pp. 120-125.
- J. L. Masonis and R. B. Bourne, “Surgical Approach, Abductor Function, and Total Hip Arthroplasty Dislocation,” Clinical Orthopaedics, Vol. 405, 2002, pp. 46-53. doi:10.1097/00003086-200212000-00006
- P. J. Daly and B. F. Morrey, “Operative Correction of an Unstable Total Hip Arthroplasty,” Journal of Bone & Joint Surgery, Vol. 74, No. 9, 1992, pp. 1334-1343.
- J. Parvizi, K. I. Kim, G. Goldberg, G. Mallo and W. J. Hozack, “Recurrent Instability after Total Hip Arthroplasty: Beware of Subtle Component Malpositioning,” Clinical Orthopaedics, Vol. 447, 2006, pp. 60-65. doi:10.1097/01.blo.0000218749.37860.7c
- L. D. Dorr and Z. Wan, “Causes of and Treatment Protocol for Instability of Total Hip Replacement,” Clinical Orthopaedics, Vol. 355, 1998, pp. 144-151. doi:10.1097/00003086-199810000-00015
- J. Parvizi, E. Picinic and P. F. Sharkey, “Revision Total Hip Arthroplasty for Instability: Surgical Techniques and Principles,” Journal of Bone & Joint Surgery, Vol. 90, No. 5, 2008, pp. 1134-1142.
- A. H. Carter, E. C. Sheehan, S. M. Mortazavi, J. J. Purtill, P. F. Sharkey and J. Parvizi, “Revision for Recurrent Instability: What Are the Predictors of Failure?” Journal of Arthroplasty, Vol. 26, No. 6, 2011, pp. 46-52. doi:10.1016/j.arth.2011.03.021
- L. Puri, B. Lapinski, R. L. Wixson, J. Lynch, R. Hendrix and S. D. Stulberg, “Computed Tomographic Follow-Up Evaluation of Operative Intervention for Periacetabular Lysis,” Journal of Arthroplasty,” Vol. 21, No. 6, pp. 78- 82. doi:10.1016/j.arth.2006.05.024
- J. P. Rao and R. Bronstein, “Dislocations Following Arthroplasties of the Hip, Incidence, Prevention, and Treatment,” Orthopedic Review, Vol. 20, No. 3, 1991, pp. 261- 264.
- F. Leiber-Wackenheim, B. Brunschweiler, M. Ehlinger, A. Gabrion and P. Mertl, “Treatment of Recurrent THR Dislocation Using of a Cementless Dual-Mobility Cup: A 59 Cases Series with a Mean 8 Years’ Follow-Up,” Orthopaedics & Traumatology Surgery & Research, Vol. 97, No. 1, 2011, pp. 8-13. doi:10.1016/j.otsr.2010.08.003
- R. Civinini, C. Carulli, F. Matassi, L. Nistri and M. Innocenti, “A Dual-Mobility Cup Reduces Risk of Dislocation in Isolated Acetabular Revisions,” Clinical Orthopaedics, Vol. 470, No. 12, 2012, pp. 3542-3548. doi:10.1007/s11999-012-2428-y
- D. Halley, A. Glassman and R. D. Crowninshield Jr., “Recurrent Dislocation after Revision Total Hip Replacement with a Large Prosthetic Femoral Head. A Case Report,” Journal of Bone & Joint Surgery, Vol. 86A, No. 4, 2004, pp. 827-830.
- K. Stromsoe and K. Eikvar, “Fascia Lata Plasty in Recurrent Posterior Dislocation after Total Hip Arthroplasty,” Archives of Orthopaedic and Trauma Surgery, Vol. 114, No. 5, 1995, pp. 292-294. doi:10.1007/BF00452090
- M. W. Shrader, J. Parvizi and D. G. Lewallen, “The Use of a Constrained Acetabular Component to Treat Instability after Total Hip Arthroplasty,” Journal of Bone & Joint Surgery, Vol. 85A, No. 11, 2003, pp. 2179-2183.
- A. E. Rady, M. K. Asal and A. A. Bassiony, “The Use of a Constrained Cementless Acetabular Component for Instability in Total Hip Replacement,” Hip International, Vol. 20, No. 4, 2010, pp. 434-439.
- Y. C. Ha, J. J. Yoo, Y. K. Lee, J. Y. Kim and K. H. Koo, “Acetabular Component Positioning Using Anatomic Landmarks of the Acetabulum,” Clinical Orthopaedics, Vol. 470, No. 12, 2012, pp. 3515-3523. doi:10.1007/s11999-012-2460-y
- J. J. Callaghan, D. W. Hennessy, S. S. Liu, K. E. Goetz and A. D. Heiner, “Cementing Acetabular Liners into Secure Cementless Shells for Polyethylene Wear Provides Durable Mid-Term Fixation,” Clinical Orthopaedics, Vol. 470, No. 11, 2012, pp. 3142-3147. doi:10.1007/s11999-012-2380-x
- J. P. Wang, W. M. Chen, C. F. Chen, C. C. Chiang, C. K. Huang and T. H. Chen, “Cementation of Cross-Linked Polyethylene Liner into Well-Fixed Acetabular Shells: Mean 6-Year Follow-Up Study,” Journal of Arthroplasty, Vol. 25, No. 3, 2010, pp. 420-424. doi:10.1016/j.arth.2008.12.003
- P. E. Beaule, E. Ebramzadeh, M. LeDuff, R. Prasad and H. C. Amstutz, “Cementing a Liner into a Stable Cementless Acetabular Shell: The Double-Socket Technique,” Journal of Bone & Joint Surgery, Vol. 86A, No. 5, 2004, pp. 929-934.
- T. R. Yoon, J. K. Seon, E. K. Song, J. Y. Chung, H. Y. Seo and Y. B. Park, “Cementation of a Metal-Inlay Polyethylene Liner into a Stable Metal Shell in Revision Total Hip Arthroplasty,” Journal of Arthroplasty, Vol. 20, No. 5, 2005, pp. 652-657. doi:10.1016/j.arth.2005.01.019
- A. Proença, F. Judas, R. Cabral, and N. Canha, “Revision Surgery of Hip Prosthesis, Osteolysis Reconstruction with Bone Allografts,” Orthopaedics Department of Coimbra University Hospitals, Coimbra, 1996.
- F. M. Judas, R. F. Dias and F. M. Lucas, “A Technique to Remove a Well-Fixed Titanium-Coated RM Acetabular Cup in Revision Hip Arthroplasty,” Journal of Orthopaedic Surgery and Research, Vol. 6, No. 31, 2011, pp. 1-5.
- P. Watson, J. R. Nixon and R. A. B. Mollan, “A Prosthesis Augmentation Device for the Prevention of Recurrent Hip Dislocation. A Preliminary Report,” Clinical Orthopaedics, Vol. 267, 1991, pp. 79-84.
- R. Maheshwari, N. H. Kumar, et al., “Unstable Hemiarthroplasty of the Hip-Treated with a Simple Technique of Acetabular Augmentation,” Journal of Arthroplasty, Vol. 22, No. 2, 2007, pp. 231-234. doi:10.1016/j.arth.2006.03.011
- R. K. Marti, H. M. Schuller, M. J. A. van Steijn, “Superolateral Bone Grafting for Acetabular Deficiency in Primary Total Hip Replacement and Revision,” Journal of Bone & Joint Surgery (British), Vol. 76, No. 5, 1994, p. 728.
- S. Olerud and G. Karlstrom, “Recurrent Dislocation after Total Hip Replacement. Treatment by Fixing an Additional Sector to the Acetabular Component,” Journal of Bone & Joint Surgery (British), Vol. 67, No. 3, 1985, p. 402.
- T. J. Gill, J. B. Sledge and M. E. Muller, “The BurchSchneider Anti-Protrusio Cage in Revision Total Hip Arthroplasty: Indications, Principles and Long-Term Results,” Journal of Bone & Joint Surgery (British), Vol. 80, 1998, pp. 946-953. doi:10.1302/0301-620X.80B6.8658
- M. Kerboull, M. Hamadouche and L. Kerboull, “The Kerboull Acetabular Reinforcement Device in Major Acetabular Reconstructions,” Clinical Orthopaedics, Vol. 378, 2000, pp. 155-168. doi:10.1097/00003086-200009000-00025
NOTES
*Conflict of Interests: The authors declare that they have no conflict of interests.
#Corresponding author.

