Open Journal of Endocrine and Metabolic Diseases
Vol.2 No.3(2012), Article ID:21496,4 pages DOI:10.4236/ojemd.2012.23005
Administration of Levothyroxine 45 - 60 Minutes before Breakfast Improves Biochemical Availability as Evidenced by Reduced Thyrotropin Levels
Department of Diabetes and Endocrinology, Peterborough City Hospital, Peterborough, UK
Email: *samoyibo@yahoo.co.uk
Received April 8, 2012; revised June 1, 2012; accepted June 20, 2012
Keywords: Levothyroxine; Thyrotropin; Bioavailability
ABSTRACT
Introduction: Serum Thyrotropin (TSH) level is used to assess adequacy of levothyroxine dosing for patients with hypothyroidism. Some patients have raised TSH levels despite being on an adequate dose of levothyroxine (100 mcg/day - 200 mcg/day). Aim: To evaluated the effect of advising patients to take their levothyroxine 45 - 60 minutes before breakfast on raised serum TSH levels. Patients and Methods: Rather than increase the dose, patients with raised TSH levels were asked to take their levothyroxine at least 45 - 60 minutes before breakfast and other oral medications. Thyroid Function Tests were assessed at base line and repeated after two months. Results: Data from ten patients who presented between 2008 and 2010 were analyzed (9 females, 1 male): with median (IQR) age: 39 (33 - 49) years and duration of hypothyroidism: 6 (3 - 7.8) years. Median (IQR) levothyroxine dose was 175 (144 - 250) mcg, serum free-Thyroxine (free-T4): 13 (10.5 - 17.1) pmol/L and serum TSH: 12.63 (6.2 - 48.3) mIU/L. After two months all patients demonstrated biochemical improvement; a decrease in serum TSH to 3.15 (0.4 - 6.1) mIU/L accompanied by an increase in serum free-T4 to 17.7 (14.8 - 21.3) pmol/L. Both changes were statistically significant (p < 0.05 and p < 0.01, respectively). The median (IQR) percentage TSH reduction was 83.5 (40.3 - 95.8) mIU/L and this bore no significant correlation with the initial TSH level (rs = 0.2, p = 0.58). Conclusion: Changing levothyroxine administration to 45 - 60 minutes before breakfast and other oral medications reduced TSH levels by 40% - 96% in all patients. We recommend this advice for all patients with hypothyroidism on adequate doses of levothyroxine but still appear biochemically under-replaced.
1. Introduction
Patients with hypothyroidism need life-long thyroid hormone replacement in the form of levothyroxine Sodium. It is generally taken once a day, but because of its long half life (6 - 7 days), there is a suggestion that it can be given once a week when there is an issue with compliance [1]. The dose of levothyroxine required is usually guided by the serum Thyroid Stimulating Hormone (Thyrotropin, TSH) levels (normal range: 0.3 - 4.2 mIU/L) and patient’s symptoms. The optimal dose of levothyroxine is generally said to be achieved when the patient’s serum TSH level is less than or equal to 2.5 mIU/L, and most patients require 1.6 microgram per kilogram body weight to achieve this [2]. Although not routinely tested, it is envisaged that the serum free Thyroxine (free-T4) will be within the normal range (12 - 22 pmol/L).
Despite being on an adequate dose of levothyroxine (100 - 200 mcg daily), some patients still present with symptoms of hypothyroidism and have persistently elevated serum TSH levels. A majority of these patients expect an increase in the dose of the levothyroxine when they go to see their general practitioner or endocrinologist and some patients have requested the addition of tri-iodothyronine to their levothyroxine. In our practice, we anecdotally noticed marked improvement in the thyroid hormone biochemical profile, in several patients after simply changing the timing of levothyroxine ingestion and this prompted us to follow up such patients.
There is data that suggest that the serum bioavailability of levothyroxine is not only dependent upon the compliant intake of levothyroxine tablets but also on other factors which affect bioavailability including concomitant ingestion of food and other oral medications and intestinal malabsorption [3].
2. Aim
We report a retrospective study, which assesses the effect of asking patients to take their levothyroxine tablets in the morning, 45 - 60 minutes before breakfast or other tablets on persistently raised serum TSH levels.
3. Patients and Methods
3.1. Patients
Eleven patients who take levothyroxine replacement therapy for hypothyroidism were referred to the endocrinologist because of persistently raised serum TSH levels, despite frequent increases in levothyroxine dose between 2008 and 2010. The cause of hypothyroidism was either primary (autoimmune hypothyroidism) or secondary to previous radioiodine treatment for Graves’ disease. None of the patients were taking any other medication that was known to disturb or reduce the intestinal absorption of levothyroxine. Additionally, none of these patients had a record of gastrointestinal disease related to malabsorption syndrome.
3.2. Methods
All patients had been taking their levothyroxine tablets along with their breakfast or just a few minutes before, except for one who took levothyroxine at bedtime. They had been on the same dose for at least three months. At presentation, a blood sample was taken for baseline serum TSH and free-T4 levels as well as serum vitamin B12, Folate, Ferritin, Calcium and Tissue Transglutaminase antibodies as a simple screening tool for malabsorption.
Rather than increase the dose of levothyroxine for these patients, we asked them to take their levothyroxine tablets earlier in the morning, at least 45 - 60 minutes before their breakfast or any other tablets. A blood sample for serum TSH and serum free-T4 was taken from each patient at the start and two months after the intervention: All samples were taken between 8:30 and 9:30 in the morning before taking their morning dose of levothyroxine and assayed within 3 hours of collection.
The baseline and post-intervention serum TSH levels (and serum free-T4 if available) were compared as paired data for each patient. Only data from patients who did both the baseline and post-intervention blood test were used for analysis.
3.3. Statistical Analysis
All group data were presented as a median (Inter-quartile range, IQR). The Wilcoxon Signed Rank test was used to detect differences in blood results between baseline and post-intervention. The Spearman’s rho (rs) test was used to detect any correlation between paired differences and baseline blood results. A p-value of <0.05 was considered statistically significant, and all tests were two-tailed.
4. Results
After the intervention, one patient did not do the postintervention blood test. Therefore, data from 10 patients (9 females and 1 male) was analyzed.
Table 1 shows the baseline data for the patient group. The median (IQR) age for the patient group was 39 (33 - 49) years and the duration of hypothyroidism was 6 (3 - 7.8) years. Eight of the patients had primary (autoimmune) hypothyroidism while two patients had hypothyroidism secondary to radioiodine treatment for previous Graves’ disease.
The median (IQR) levothyroxine dose at the time of presentation for the patient group was 175 (144 - 250) mcg and the dose per kilogram bodyweight was 2.2 (1.9 - 2.6) mcg/kg. The baseline serum TSH was 12.63 (6.2 - 48.3) mIU/L, with a baseline free-T4 of 13 (10.5 - 17.1) pmol/L.
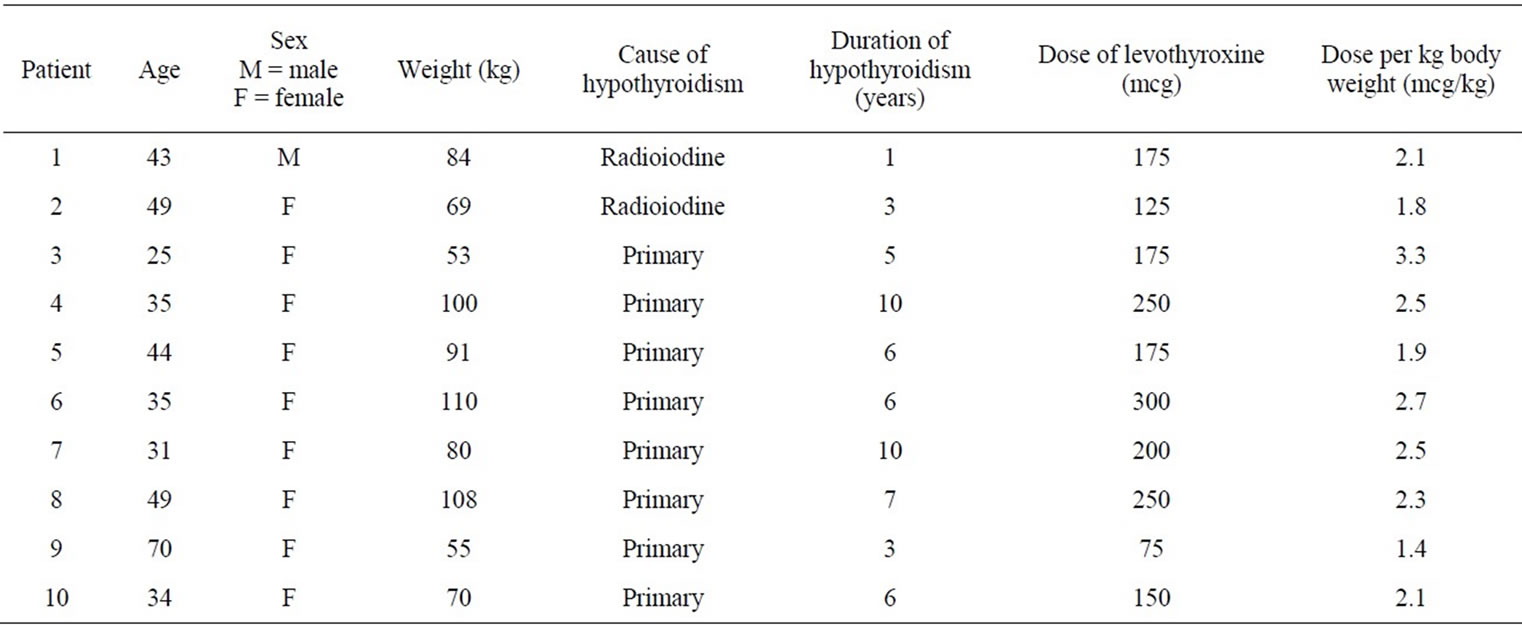
Table 1. Baseline data for the group of patients.
After two months, all patients demonstrated improvement in their blood results. There was a statistically significant reduction (Figure 1) in the median (IQR) serum TSH level to 3.15 (0.4 - 6.1) mIU/L (p < 0.01). The median (IQR) percentage TSH reduction was 83.5 (40.3 - 95.8) and this bore no significant correlation with the initial (baseline) TSH level (rs = 0.2, p = 0.58).
Although paired baseline and post-intervention serum free-T4 data was obtained for only 6 of the 10 patients, there was still a statistically significant corresponding increase (Figure 2) in the serum free-T4 level to 17.7 (14.8 - 21.3) pmol/L (p < 0.05).
5. Discussion
Our patient group were mainly females who took their levothyroxine tablets along with breakfast and other tablets, apart from one patient who took levothyroxine tablets at
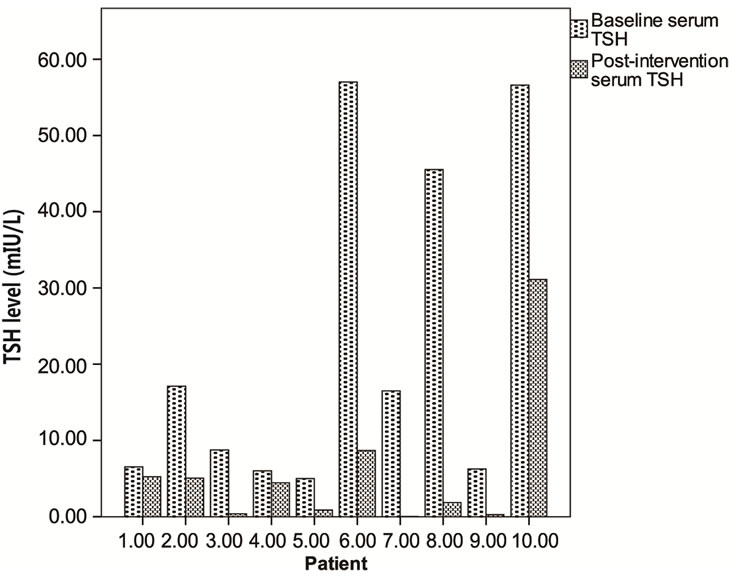
Figure 1. Baseline and post-intervention serum TSH levels for the patients.
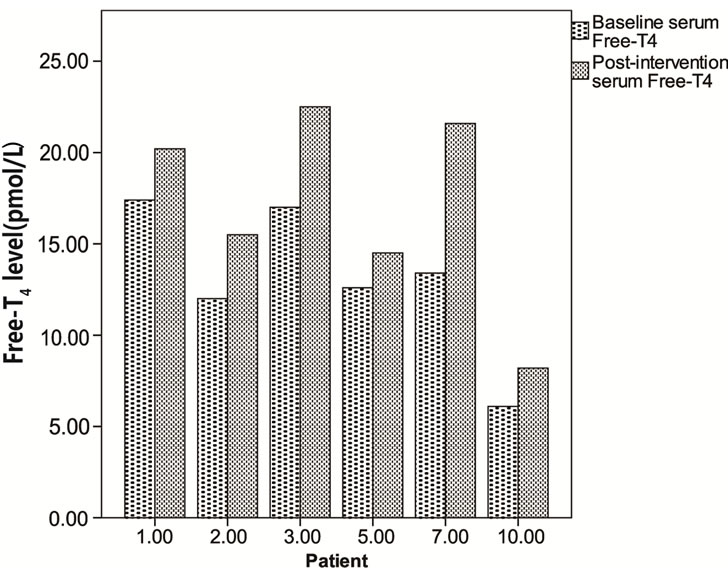
Figure 2. Baseline and post-intervention serum free-T4 levels for six patients.
bed time. When asked about this, they said that they were never instructed otherwise. These patients had very high serum TSH levels that would suggest poor drug compliance, but there was no putative reason to doubt compliance in this patient group. Additionally, routine blood tests carried out at the time of the baseline serum TSH did not suggest any evidence of intestinal malabsorption.
Levothyroxine sodium is the standard thyroid hormone replacement therapy for treating patients with hypothyroidism. The dose is usually adjusted according to patient’s symptoms and the serum TSH level, with the aim of keeping the serum TSH level towards the lower half of the reference range (0.4 - 2.5 mIU/L) [4]. Patients are usually followed up by their general practitioners, and when on a stable dose they need biochemical assessment (TSH assay) only once a year, but may require additional TSH assays two to three months after a change in their levothyroxine dose.
The product literature for levothyroxine does mention that patients should take the tablet before food, but a majority of patients when asked, take their levothyroxine with their breakfast. Previous studies have suggested that certain food substances (e.g., soy, coffee, fibre) may bind to and decrease the absorption of levothyroxine in the gastrointestinal tract [5-7].
A previous study has suggested that thyroid hormone profiles are better when levothyroxine is taken at night when compared to taking it in the morning, and that this was likely due to better gastrointestinal absorption of levothyroxine at night [8]. However, the patients in that study initially took their tablets thirty minutes before breakfast, and the possibility that a thirty minute gap may still be too close to breakfast and other medications needs to be contemplated, as suggested in another study [9].
In our study we had one patient who took her levothyroxine tablet at bedtime. Even this patient had marked biochemical (serum TSH) improvement when she changed to taking her tablets 45 - 60 minutes before breakfast.
Malabsorption of levothyroxine can occur after intestinal bypass surgery, liver cirrhosis, congestive cardiac failure, lactose intolerance, coeliac disease and when ingested with other medications, such as Calcium Carbonate, Lovastatin, Cholestyramine, Ferrous Sulphate, Aluminium Hydroxide and Proton Pump Inhibitors [10]. The patients in our study were not on any of these medications and did not have any of these co-morbidities. Another important factor is whether the patient is actually taking the levothyroxine tablets in the first place. This phenomenon, known as pseudomal absorption is a well recognised and growing problem [11].
This study is not without limitations. It was a small, uncontrolled retrospective study and we therefore cannot ascertain whether just seeing the endocrinologist alone might be enough to account for these changes by improving compliance, irrespective of the timing of the dose. A randomised controlled study would be required to assess this further. Additionally, there was no other method for establishing prior compliance to taking levothyroxine other than to ask the patient. Supervised administration of levothyroxine would need to be incorporated into a randomised controlled study to eliminate any doubts of poor compliance.
6. Conclusion
This retrospective study has demonstrated that reminding patients to take their levothyroxine on an empty stomach, at least 45 - 60 minutes before breakfast will not only improve the absorption of the tablet, but also avoid the need for continued dose increments. A large doubleblinded, randomised, cross-over study will be needed to justify whether taking levothyroxine at bedtime is biochemically better than taking it first thing in the morning, 45 - 60 minutes before breakfast.
REFERENCES
- S. K. Grebe, R. R. Cooke and H. C. Ford, “Treatment of Hypothyroidism with Once Weekly Thyroxine,” Journal of Clinical Endocrinology and Metabolism, Vol. 82, No. 3, 1997, pp. 870-875. doi:10.1210/jc.82.3.870
- L. H. Fish, H. L. Schwartz, J. Cavanaugh, M. W. Steffes, J. P. Bantle and J. H. Oppenheimer, “Replacement Dose, Metabolism, and Bioavailability of Levothyroxine in the Treatment of Hypothyroidism. Role of Triiodothyronine in Pituitary Feedback in Humans,” The New England Journal of Medicine, Vol. 316, 1987, pp. 764-770. doi:10.1056/NEJM198703263161302
- K. W. Wenzel and H. E. Kirschsieper, “Aspects of the Absorption of Oral L-Thyroxine in Normal Man,” Metabolism, Vol. 26, No. 1, 1977, pp. 1-8. doi:10.1016/0026-0495(77)90121-4
- B. Vaidya and S. H. Pearce, “Management of Hypothyroidism in Adults,” British Medical Journal, Vol. 337, 2008, p. a801. doi:10.1136/bmj.a801
- D. S. Bell and F. Ovalle, “Use of Soy Protein Supplement and Resultant Need for Increased Dose of Levothyroxine,” Endocrine Practice, Vol. 7, No. 3, 2001, pp. 193- 194.
- S. Benvenga, L. Bartolone, M. A. Pappalardo, A. Russo, D. Lapa, G. Giorgianni, G. Saraceno and F. Trimarchi, “Altered Intestinal Absorption of L-Thyroxine Caused by Coffee,” Thyroid, Vol. 18, No. 3, 2008, pp. 293-301. doi:10.1089/thy.2007.0222
- Y. Liel, I. Harman-Boehm and S. Shany, “Evidence for a Clinically Important Adverse Effect of Fiber-Enriched Diet on the Bioavailability of Levothyroxine in Adult Hypothyroid Patients,” Journal of Clinical Endocrinology and Metabolism, Vol. 81, No. 2, 1996, pp. 857-859. doi:10.1210/jc.81.2.857
- N. Bolk, T. J. Visser, A. Kalsbeek, R. T. van Domburg and A. Berghout, “Effects of Evening vs Morning Thyroxine Ingestion on Serum Thyroid Hormone Profiles in Hypothyroid Patients,” Clinical Endocrinology, Vol. 66, 2007, pp. 43-48.
- S. Benvenga, L. Bartolone, S. Squadrito, F. Lo Giudice and F. Trimarchi, “Delayed Intestinal Absorption of Levothyroxine,” Thyroid, Vol. 5, No. 4, 1995, pp. 249-253. doi:10.1089/thy.1995.5.249
- L. Liwanpo and J. M. Hershman, “Conditions and Drugs Interfering with Thyroxine Absorption,” Best Practice and Research Clinical Endocrinology and Metabolism, Vol. 23, No. 6, 2009, pp. 781-792. doi:10.1016/j.beem.2009.06.006
- V. Srinivas and S. O. Oyibo, “Levothyroxine Pseudomalabsorption and Thyroxine Absorption Testing with Use of High-Dose Levothyroxine: Case Report and Discussion,” Endocrine Practice, Vol. 16, No. 6, 2010, pp. 1012-1015. doi:10.4158/EP10224.CR
NOTES
*Corresponding author.

