World Journal of Cardiovascular Diseases
Vol.4 No.2(2014), Article ID:42803,6 pages DOI:10.4236/wjcd.2014.42007
Effect of intravenous gamma globulin on shortand mid-term clinical outcome in acute viral myocarditis in children
Section of Pediatric Cardiology, Department of Pediatrics and Child Health, Aga Khan University Hospital, Karachi, Pakistan
Email: mehnaz.atiq@aku.edu
Copyright © 2014 Mehnaz Atiq et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Mehnaz Atiq et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received 29 October 2013; revised 15 December 2013; accepted 23 December 2013
KEYWORDS
Acute Myocarditis; Intravenous Gamma Globulins; Congestive Heart failure
ABSTRACT
Acute viral myocarditis is an extremely diverse disease with a predictable good outcome with supportive therapy. The objective of this study was to look at the clinical outcome of patients receiving additional intravenous gamma globulin compared to those receiving conventional anti-congestive therapy alone. Patients and methods: This is a retrospective review of charts of children admitted with acute myocarditis. Group 1 was children who received intravenous gamma globulin (IVIG) along with conventional anti-congestive therapy. Group 2 were patients who received the conventional anticongestive therapy alone. Short-term outcome was survival to hospital discharge, and midterm outcome was improvement of left ventricular ejection fraction at 6 months and one year follow-up. Results: A total of 36 patients were enrolled and 18 were males. The mean age of all patients was 2.3 ± 2.6 years and the mean duration of illness for the whole group was 6.7 ± 3.8 days. Group 1 comprised of 16 patients. There was no difference in short-term outcome with mortality of 2 patients in Group1 (12.5%) and 3(15%) in Group 2 (p = 0.2). At intermediate term follow up, recovery of ejection fraction in Group 1 was in 4/14 (28%) and in Group 2 it was 9/17 (55%) and at 12 months it was 10/13 (77%) in Group 1 and 15/16 (94%) in Group 2 (p = 0.02 and 0.19 respectively). Conclusion: Acute myocarditis has a high spontaneous cure rate. Our study did not show any significant difference in the short-term or midterm outcome between children receiving IVIG compared to those who did not.
1. INTRODUCTION
Acute viral myocarditis is an extremely diverse disease in its presentation and outcome. Clinical manifestations range from nonspecific systemic symptoms to cardiogenic shock and sudden death. The pathogenesis of myocarditis has been extensively studied in murine models. Direct cytopathic effect of a cardiotropic virus rapidly progresses to the subsequent phase of immunologic activation [1]. The former leads to myofibril death due to direct viral invasion and the latter causes continued immune mediated myocardial damage. The natural history, however, is good and predictable, making influence of treatment strategies skeptical [2]. There are variable reports on the use of high dose intravenous gamma globulin (IVIG) in children and adults with acute myocarditis [3-9]. In many centers, IVIG has become the standard therapy of choice for adults and children with acute viral myocarditis. The objective of this study was to look at the clinical outcome of patients receiving additional intravenous gamma globulin compared to those receiving conventional anti-congestive therapy alone.
2. PATIENTS AND METHODS
Charts of children admitted with acute myocarditis during the last five years were reviewed. A proforma addressing the symptoms, duration, hemodynamic status, cardiac enzymes, electrocardiographic tracings, radiological abnormalities, echocardiographic findings, medical treatment, mechanical ventilation, complications and shortterm and mid-term outcome was made.
The diagnosis of acute viral myocarditis was made when there was an evidence of acute myocardial dysfunction by history, physical exam, chest X-ray, electrocardiogram (ECG) and echocardiogram associated with an elevation of cardiac enzymes such as creatinine phosphokinase MB fraction (CK-MB) and cardiac troponin I. We excluded patients with possible dilated cardiomyopathy by history, physical examination or investigations. Also children with acute congestive heart failure secondary to enteric fever, sepsis, Kawasaki disease, acute kidney injury, thalassemia major, inborn error of metabolism, skeletal myopathy and cardiotoxic chemotherapeutic drug were excluded.
Abnormalities on chest X-ray included cardiomegaly and pulmonary edema. Cardiomegaly was diagnosed if the cardiothoracic (CT) ratio was >50% in upright films and >60% in infants with supine shoots. Pulmonary edema was graded as evolving when streaky infiltrates were seen fanning out from the lung hila in “butterfly fashion” or frank, when all lung fields had homogenous opacities. Abnormalities on ECG included low voltage QRS complexes in limb leads, ST segment and T wave changes and arrhythmias. Echocardiographic examination included measurements of left ventricular dimension and function from M-mode and two-dimensional images in the parasternal long-axis view. Fractional shortening and ejection fraction were considered normal if the values were more than 28% and 60% respectively. Color flow mapping was used to evaluate the valve regurgitation and its severity. Presence of pericardial effusion and intraventricular thrombi were noted. In eleven patients, a right ventricular endomyocardial biopsy was performed. The nonconformity in some tests was due to physicians’ preferences.
Patients were grouped into two: Group 1 was children who received intravenous gamma globulin (IVIG) along with conventional anti-congestive therapy. The dose of IVIG was a single dose of 2 gm/Kg. Group 2 was patients who received the conventional anticongestive therapy alone. The administration of IVIG was based on clinical severity and on physician’s discretion. Some clinicians would use it in all patients and some only those with shock or arrhythmias. Short-term outcome was survival to hospital discharge, and intermediate term outcome was at 6 months and one year follow-up. Echocardiography was done on admission, on discharge, 1 month, 6 months, 9 months, 12 months and half yearly thereafter. Patient was considered recovered (if left ventricular ejection fraction was 60%), improved but not recovered, static or deteriorating.
3. STATISTICAL ANALYSIS
Data was computed on Statistical Package for Social Sciences (SPSS version 19). Most of the results were expressed as mean (± SD). Between the groups, analysis of quantitative variables was done with independent sample Students, “t” test and categorical variables were performed with chi-square. Recovery curves were generated using the Kaplan-Meir method. The level of significance of p < 0.05 was chosen for all statistical comparisons.
4. RESULTS
A total of 36 patients were enrolled in the study of which 18 were males. Sixteen patients were in Group 1 and they received additional IVIG to conventional therapy whereas 20 children in Group 2 received conventional anti-congestive therapy. The mean age of all patients was 2.3 ± 2.6 years (range 4 months to 13 years). The mean duration of illness in the whole group was 6.7 ± 3.8 days (range 12 hours - 30 days). The chief presenting symptoms are listed in Table 1. The mean age of children in Group 1 was 2.39 ± 3.46 years and 2.36 ± 1.75 years in Group 2.There were 11 (69%) females and 5 (31%) males in Group 1 and 7 (35%) female and 13 (65%) males in Group 2. Chest X-Ray showed cardiomegaly in 70%, evidence of mild pulmonary edema in 20 (56%) and frank pulmonary edema in 10 (28%). Electrocardiography showed low voltage QRS complexes and/or ST-T changes in all patients. Six patients had ventricular ectopic beats and one had ventricular tachycardia.
The two groups were compared with respect to clinical, investigational, treatment and outcome parameters (Table 2). There was no statistical difference found in the mean age and duration of illness. The symptoms in the two groups did not differ either. The mean left ventricular ejection fraction for all patients was 27% ± 9.3% and fractional shortening was 13.9% ± 5.0%. Both the groups received intravenous inotropes with milrinone or dobutamine, furosemide, angiotensin converting enzyme (ACE) inhibitor and carvedilol (after stabilization of blood pressure) in the acute phase. The mean duration of stay was 6.7 ± 3.8 days. Children receiving IVIG were in the hospital for a significantly longer time (9.1 ± 4.2 versus 4.9 ± 3.4. p = 02).
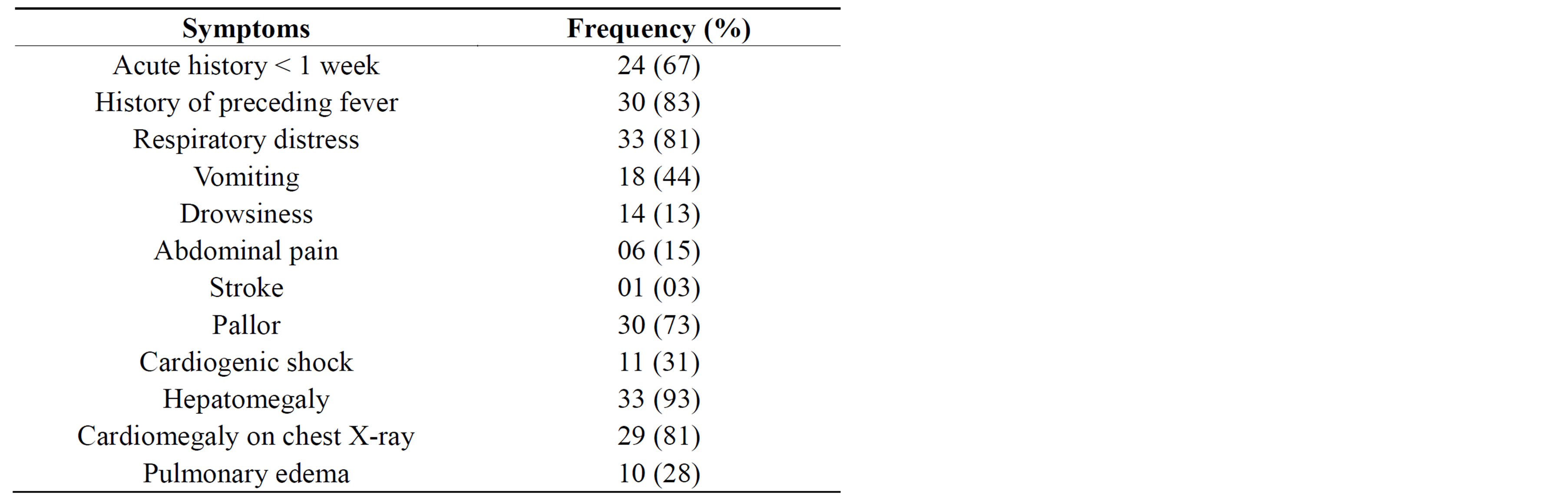
Table 1. Symptoms and signs at presentation in all children.
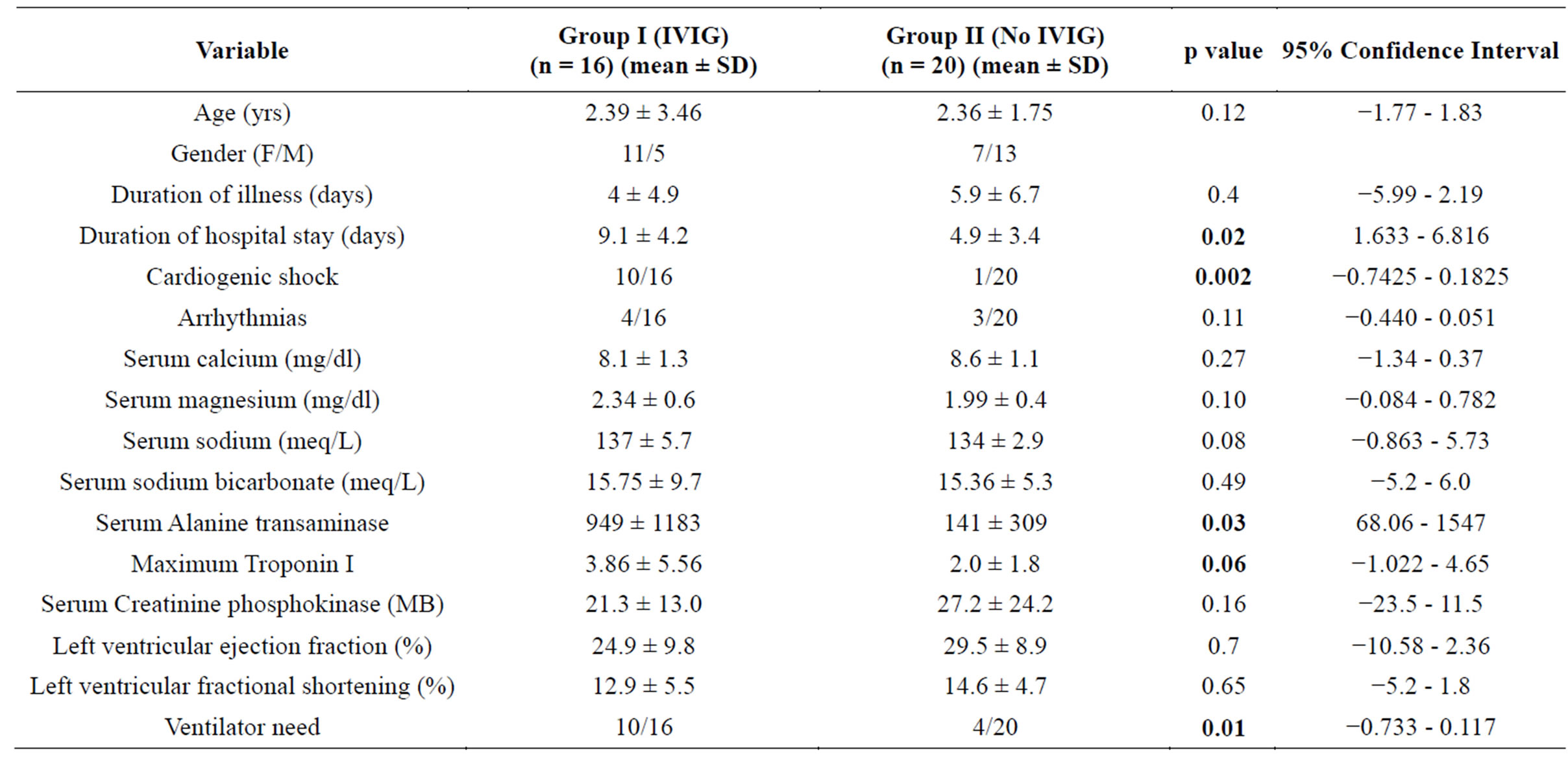
Table 2. Comparison of variables between study groups.
There was no difference in short-term outcome with mortality of 2 patients in Group 1 (12.5%) and 3 (15%) in Group 2 (p = 0.2). One patient had stroke in Group 2. At mid-term follow up, recovery of ejection fraction in group 1 was in 4/14 (28%) and in Group 2 it was 9/17 (55%) and at 12 months it was 10/13 (77%) in Group 1 and 15/16 (94%) in Group 2 (p = 0.02 and 0.19 respectively). The Kaplan-Meir recovery curve showed a significantly earlier mean recovery time in Group 2 (260.45 ± 25.11 days) compared to Group 1 (319.25 ± 24.45 days) (Log rank Mantel Cox comparison between groups, p = 0.025) (Figure 1). One patient was lost to follow up in both groups after 6 months.
5. DISCUSSION
Acute myocarditis is a non-ischemic immune mediated inflammatory disorder and the most common cause is infection with a cardiotropic virus [10]. Children with mild myocarditis may be asymptomatic with spontaneous resolution of the insidious disease [11]. Fulminant myocarditis presents with severe heart failure, cardiogenic shock, and if not treated aggressively, carries a high mortality, up to 45% [12-14]. However, recovery in this subset of children is paradoxically very high [15-18]. Despite well studied morbidity and mortality, clear clinical guidelines for management of acute viral myocarditis are lacking [19,20].
In the European Study of Epidemiology and Treatment of Cardiac Inflammatory Diseases (ESETCID), 72% of patients presented with dyspnea, 32% had chest pain, and 18% had arrhythmias [21]. In our study, dyspnea was present in 80% of patients and arrhythmia seen in 19%.
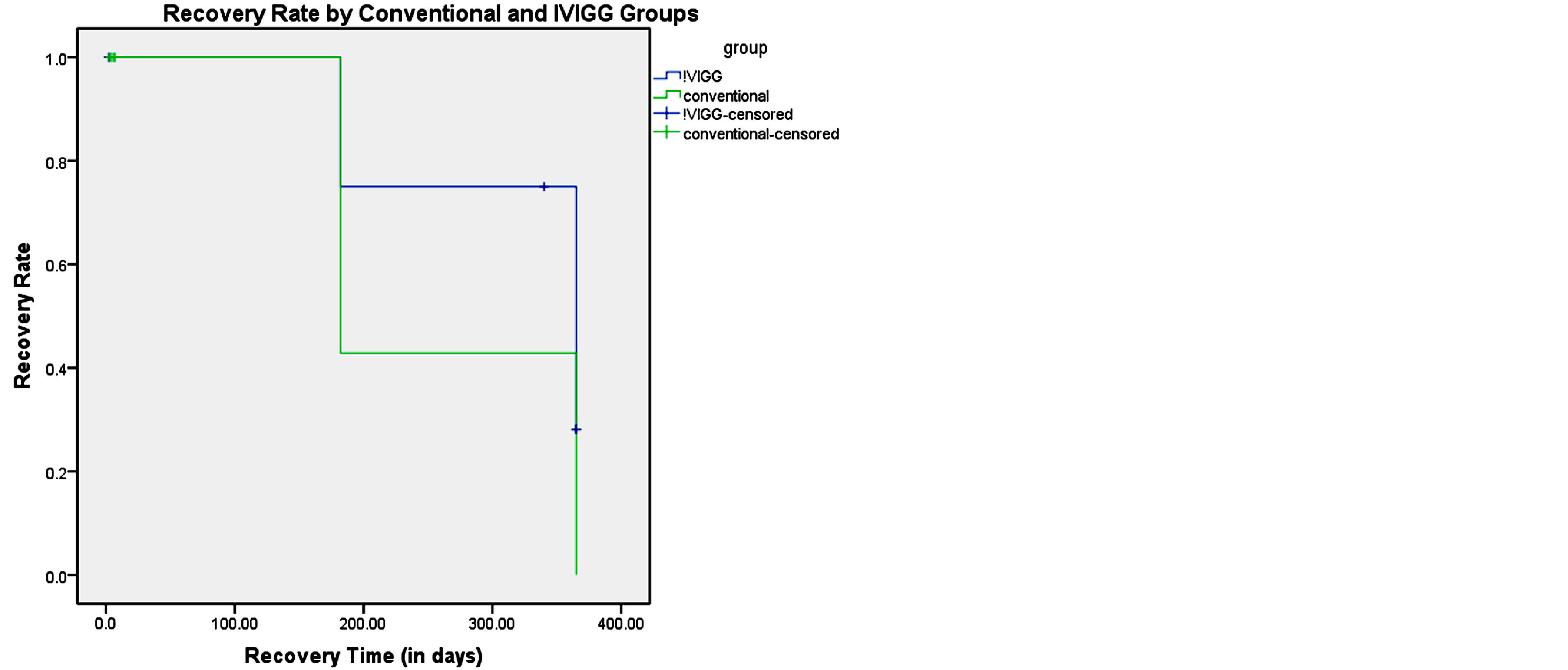
Figure 1. Kaplan Meir recovery curve.
Log rank (Mantel-Cox) overall comparison; Mean recovery time in Group 1 = 319. 25 ± 24.45 days, in Group 2 = 260. 45 ± 25.11 days, p = 0.025.
In a report by Blauwet and Cooper [2], clinical presentation varied with age, the most fulminant presentation was in infants, who present with non-specific symptoms of poor feeding, lethargy and respiratory distress. Older children may complain of abdominal pain, chest pain, cough, fatigue.
Electrocardiographic abnormalities were reported in only 47% of adult and pediatric cases in the form of non-specific ST-T wave changes and 55% had new onset arrhythmias [2,22]. We found changes in all our patients either ST-T waves or low voltage QRS amplitude. Left ventricular systolic dysfunction (less commonly affected were diastolic and index of global function) is the commonly used echocardiographic abnormality. In fulminant myocarditis, the left ventricular wall thickness may be preserved with smaller cavity as compared to insidious onset myocarditis in which the wall thickness may be thin [23]. Right ventricular systolic dysfunction is relatively uncommon but is a strong predictor for death or cardiac transplant [24].
Spontaneous improvement in myocardial systolic function has been reported to occur in 70% of children [3]. In a study reported by McNamara et al., most of the improvement occurred within the first 6 months [25]. The present study showed that in children receiving conventional therapy alone, 55% improved in the first six months and 90% in one year.
Optimum treatment of acute myocarditis is probably unknown, but the management approach varies according to disease severity. For acute presentation, the mainstay of therapy is largely supportive with anti-congestive medications because of the known natural improvement. Conventional therapy includes diuretics, angiotensin-converting enzyme inhibitors, beta-blockers, and low dose digoxin [2]. In fulminant cases, aggressive management of shock with ventilator support and mechanical assist devices has yielded good results [18]. Intensive care therapy with mechanical ventilation was required in 14/36 (39%) of cases.
Several uncontrolled trials of immunosuppression with steroids, cytotoxic drugs, monoclonal antibodies (OKT3) and immunoglobulin have been reported [4,7,9,10,14,26]. These modalities had shown improvement in inflammatory exudates within the myocardium but in many reports, it did not translate into significant improvement in myocardial function or long term survival [1,21]. Investigators have even reported relapse after discontinuation of immunosuppressive therapy [26].
Intravenous immunoglobulin has antiviral, anti-inflammatory and immune modulating effects and may suppress proinflammatory cytokines (TNF, INF, interleukins, release of nitric oxide) and reduce oxidative stress [2,27,28]. Numerous observational studies and case reports are found in favor of use of IVIG in acute viral myocarditis [3,5], but no randomized controlled trials testifying its beneficial role are found to recommend its routine use in children [29]. In one of the earlier studies conducted in 21 children, intravenous immunoglobulin (2 g/kg) demonstrated a trend for better survival in the immunoglobulin treated group when compared to controls receiving conventional treatment [4]. IVIG has shown to have significantly benefitted children presenting with fulminant myocarditis either in cardiogenic shock or complete heart block [4,7,9,30]. In our study 80% (2/10) children presenting with cardiogenic shock recovered with aggressive management which also included IVIG.
Robinson et al. reviewed adults in Cochrane database and found only one relevant study in adults with acute viral myocarditis and did not find any beneficial effect of IVIG [31]. Similarly English et al. [32] did not find any benefit of IVIG alone or in combination with steroids in their patients in context with short-term or long term outcome, mortality, complete or incomplete recovery. Kim and colleagues [1] similarly found no statistical difference in the clinical outcome of children receiving IVIG. Klugman and colleagues [8] found no advantage of IVIG which was used in 49% of 216 children with acute myocarditis. In our series we did not find any statistical difference in the shortand midterm outcome in children who received IVIG. However in our series patient selection was not randomized and the sicker ones received IVIG. Lee et al. [27] have reported 45% mortality in patients with fulminant myocarditis. This was definitely reduced in our study, where this mortality was 12.5%. On the other hand, time to recovery was shorter in the conventional group.
Despite the lack of supportive clinical data for its use, IVIG is a part of standard therapy for the treatment of acute viral myocarditis in children and adults. A large randomized controlled trial is required to substantiate the benefit of IVIG in children. Until such trials we may be able to identify children who may have predictable bad outcome, providing rationale for use of IVIG. Clinical and investigational criteria for adverse outcome include tachycardia, hypotension, elevated C reactive protein and cardiac enzymes, wide QRS complexes on ECG, left ventricular end diastolic dimension and very low ejection fraction on echocardiography [3,27]. Fuse et al. found significant low systolic and diastolic blood pressures, high pulmonary capillary wedge pressures, more need for mechanical ventilation, and elevated protein sFas and sFas-L (type II transmembrane proteins belonging to tumor necrosis factor family, involved in cell apoptosis and immune regulation) in patients who died of acute viral myocarditis [20]. The electrocardiographic predictors of poor outcome and sudden cardiac death include abnormal QRS complexes, northwest QRS axis, new onset left bundle branch block, pseudo-infarct pattern of ST elevation, ventricular arrhythmias [16]. Mendes et al. found right ventricular dysfunction as an independent risk factor for poor outcome [24].
Limitation of this study was the small number in each group and the non conformity in management between consultants. The study compared use of IVIG in sicker children and the prolonged hospital stay may have been due to that itself.
6. CONCLUSION
Acute myocarditis is a potentially life threatening disease in children but has a high spontaneous cure rate. IVIG has been used to treat acute viral myocarditis, but its role has to be defined. Our study did not show significant difference in the short or midterm outcome between children receiving or not receiving IVIG. A large randomized controlled trial is required to establish the benefit and advocate routine use of IVIG in childhood myocarditis.
ACKNOWLEDGEMENTS
We would like to acknowledge the kind assistance provided by Iqbal Azam in statistical analysis in our study.
REFERENCES
- Kim, H.J., Yoo, G.H. and Kil, H.R. (2010) Clinical outcome of acute myocarditis in children ccording to treatment modalities. Korean Journal of Pediatrics, 53, 745- 752. http://dx.doi.org/10.3345/kjp.2010.53.7.745
- Blauwet, L.A. and Cooper, L.T. (2010) Myocarditis. Progress in Cardiovascular Diseases, 52, 274-288. http://dx.doi.org/10.1016/j.pcad.2009.11.006
- D’Ambrosio, A., Patti, G., Manzoli, A., Sinagra, G., Di Lenarda, A., Silvestri, F. and Di Sciascio, D. (2001) The fate of acute myocarditis between spontaneous improvement and evolution to dilated cardiomyopathy: A review. Heart, 85, 499-504. http://dx.doi.org/10.1136/heart.85.5.499
- Drucker, N.A., Colan, S.D., Lewis, A.B., Beiser, A.S., Wessel, D.L., Takahashi, M., Baker, A.L., Perez-Atayde, A.R. and Newburger, J.W. (1994) Gamma-globulin treatment of acute myocarditis in the pediatric population. Circulation, 89, 252-257. http://dx.doi.org/10.1161/01.CIR.89.1.252
- Frustaci, A., Chimenti, C., Calabrese, F., et al. (2003) Immunosuppressive therapy for active lymphocytic myocarditis: Virological and immunologic profile of responders versus nonresponders. Circulation, 107, 857-863. http://dx.doi.org/10.1161/01.CIR.0000048147.15962.31
- Haque, A., Bhatti, S. and Siddiqui, F.J. (2009) Intravenous immune globulin for severe acute myocarditis in children. Indian Pediatr, 46, 810-811.
- Kim, H.S., Sohn, S., Park, J.Y. and Seo, J.W. (2004) Fulminant myocarditis successfully treated with high dose immunoglobulin. International Journal of Cardiology, 96, 485-486. http://dx.doi.org/10.1016/j.ijcard.2003.05.037
- Klugman, D., Berger, J.T., Sable, C.A., He, J., Khandewal, S.G. and Slonim, A.D. (2010) Pediatric patients hospitalized with myocarditis: A multi-institutional analysis. Pediatric Cardiology, 31, 222-228. http://dx.doi.org/10.1007/s00246-009-9589-9
- Takeda, Y., Yasuda, S., Miyazaki, S., Daikoku, S., Nakatani, S. and Nonogi, H. (1998) High-dose immunoglobulin G therapy for fulminant myocarditis. Japanese Circulation Society, 62, 871-872. http://dx.doi.org/10.1253/jcj.62.871
- Kendirli, T., Nacar, N., Ciftci, E., Belgemen, T., Ince, E., Atalay, S. and Tutar, E. (2003) Cardiac Troponin I in acute myocarditis treated with a 12-hour infusion of high dose intravenous immunoglobulin. J Ankara Med School, 25, 89-94.
- Parrillo, J.E. (2001) Inflammatory cardiomyopathy (Myocarditis): Which patients should be treated with anti-inflammatory therapy? Circulation, 104, 4-6. http://dx.doi.org/10.1161/hc2601.092124
- Batra, A.S. and Lewis, A.B. (2001) Acute myocarditis. Current Opinion in Pediatrics, 13, 234-239. http://dx.doi.org/10.1097/00008480-200106000-00004
- Levi, D. and Alejos, J. (2001) Diagnosis and treatment of pediatric viral myocarditis. Current Opinion in Cardiology, 16, 77-83. http://dx.doi.org/10.1097/00001573-200103000-00001
- Tang, W.H.W. and Ooi, H.H. (2010) Myocarditis: Current treatment overview. Journal of Cardiac Failure, 16, E176-E179.
- McCarthy, R.E., Boehmer, J.P., Hruban, R.H., Hutchins, G.M., Kasper, E.K., Hare, J.M. and Baughman, K.L. (2000) Long-Term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. The New England Journal of Medicine, 342, 690-695. http://dx.doi.org/10.1056/NEJM200003093421003
- Morgera, T., Di Lenarda, A., Dreas, L., et al. (1992) Electrocardiography of myocarditis revisited: Clinical and prognostic significance of electrocardiographic changes. American Heart Journal, 124, 433-467. http://dx.doi.org/10.1016/0002-8703(92)90613-Z
- Schultz, J.C., Hilliard, A.A., Cooper Jr., L.T. and Rihal, C.S. (2009) Diagnosis and treatment of viral myocarditis. Mayo Clinic Proceedings, 84, 1001-1009.
- Vashist, S. and Singh, G.K. (2009) Acute myocarditis in children: Current concepts and management. Current Treatment Options in Cardiovascular Medicine, 1, 383- 391. http://dx.doi.org/10.1007/s11936-009-0039-z
- Burch, M. (2004) Immune suppressive treatment in paediatric myocarditis: Still awaiting the evidence. Heart, 90, 1103-1104. http://dx.doi.org/10.1136/hrt.2004.034082
- Fuse, K., Kodama, M., Okura, Y., Ito, M., Hirono, S., Kato, K., Hanawa, H. and Aizawa, Y. (2000) Predictors of disease course in patients with acute myocarditis. Circulation, 102, 2829-2835. http://dx.doi.org/10.1161/01.CIR.102.23.2829
- Hufnagel, G., Pankuweit, S., Richter, A., Schonian, U. and Maisch, B. (2000) The European Study of Epidemiology and Treatment of Cardiac Inflammatory Diseases (ESETCID). First epidemiological results. Herz, 25, 279- 285. http://dx.doi.org/10.1007/s000590050021
- Durani, Y., Egan, M., Baffa, J., et al. (2009) Pediatric myocarditis: Presenting clinical characteristics. The American Journal of Emergency Medicine, 27, 942-947. http://dx.doi.org/10.1016/j.ajem.2008.07.032
- Felker, G.M., Boehmet, J.P., Hruban, R.H., Hutchins, G.M., Kasper, E.K., Baughman, K.L. and Hare, J.M. (2000) Echocardiographic findings in fulminant acute myocarditis. Journal of the American College of Cardiology, 36, 227-232. http://dx.doi.org/10.1016/S0735-1097(00)00690-2
- Mendes, L.A., Dec, G.W., Picard, M.H., Palacios, I.F., Newell, J. and Davidoff, R. (1994) Right ventricular dysfunction: An independent predictor of outcome in patients with myocarditis. American Heart Journal, 128, 301-307. http://dx.doi.org/10.1016/0002-8703(94)90483-9
- McNamara, D.M., Holubkov, R., Starling, R.C., Dec, G.W., Loh, E., Torre-Amione, G., et al. (2001) Controlled trial of intravenous immune globulin in recentonset dilated cardiomyopathy. Circulation, 103, 2254-2259.
- McNamara, D.M., Starling, R.C., Dec, G.W., et al. (1999) Intervention in myocarditis and acute cardiomyopathy with immune globulin: Results from the randomized placebo controlled IMAC trial. Circulation, 100, I-21.
- Lee, C.H., Tsai, W.C., Hsu, C.H., Liu, P.Y., Lin, L.J. and Chen, J.H. (2006) Predictive factors of a fulminant course in acute myocarditis. International Journal of Cardiology, 109, 142-145. http://dx.doi.org/10.1016/j.ijcard.2005.04.014
- Magnani, J.W. and Dec, G.W. (2006) Myocarditis: Current trends in diagnosis and treatment. Circulation, 113, 876-890. http://dx.doi.org/10.1161/CIRCULATIONAHA.105.584532
- Wheeler, D.S. and Kooy, N.W. (2003) A formidable challenge: The diagnosis and treatment of viral myocarditis in children. Critical Care Clinics, 19, 365-391.
- Tsai, Y.G., Ou, T.Y., Wang, C.C., Tsai, M.C., Yuh, Y.S. and Hwang, B. (2001) Intravenous gamma-globulin therapy in myocarditis complicated with complete heart block: Report of one case. Acta Paediatr Taiwan, 42, 311-313.
- Robinson, J., Hartling, L., Vandermeer, B., Crumley, E. and Klassen, T.P. (2005) Intravenous immunoglobulin for presumed viral myocarditis in children and adults. Cochrane Database of Systematic Reviews, 25, Article ID: CD004370.
- English, R.F., Janosky, J.E., Ettedgui, J.A. and Webber, S.A. (2004) Outcomes for children with acute myocarditis. Cardiology in the Young, 14, 488-493. http://dx.doi.org/10.1017/S1047951104005049

