Open Journal of Therapy and Rehabilitation
Vol.2 No.1(2014), Article ID:42919,7 pages DOI:10.4236/ojtr.2014.21002
Prosthetic education: Are occupational therapy students’ needs being met?
![]()
1Department of Kinesiology, San Francisco State University, San Francisco, USA; *Corresponding Author: marilynsfsu@gmail.com
2Department of Physical Medicine and Rehabilitation, Baylor College of Medicine, Houston, USA
Copyright © 2014 Marilyn Mitchell et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Marilyn Mitchell et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received 6 November 2013; revised 9 December 2013; accepted 18 December 2013
KEYWORDS
Arm Prostheses; Occupational Therapy; Academic Training
ABSTRACT
Based on a previous survey on prosthetics and orthotics training in occupational therapy (OT) [1], we developed a 14-question online questionnaire that was made available to the directors of 167 occupational therapy programs (Masters and Ph.D.) in the US and Canada. Fiftytwo surveys were completed for a response rate of 31%. Overall, the results indicated that since the previous survey, little has changed in the amount of time and emphasis OT faculty assign to providing training in prosthetics and orthotics, or in the training experiences, OT students receive. Notably, only a few hours of the total OT curriculum is devoted to training in prosthetics. For the majority of programs (62%) the content was embedded within related classes. Only 32% of programs had a required lecture in prosthetics/orthotics. Despite the lack of time given in the curriculum, 85% of program directors thought that training in prosthetics/orthotics was important or very important. The use of prosthetic simulators was reported as the single most desirable training tool. However, lack of time and overcrowding in the curriculum were cited as the greatest barriers to providing more training to students. We elaborate on these findings, discuss their implications for OT students and practitioners, and provide specific recommendations about how to overcome the barriers and enhance upper limb amputee exposure and knowledge through the prosthetic training experience.
1. INTRODUCTION
An estimated 1.8 million people in the United States live with some form of amputation and this number is expected to more than double by 2050 [2]. The major causes for lower limb amputation are vascular disease, with diabetes-caused vascular disease being the leading factor, and traumatic injury, with the number of amputations increasing dramatically due to injuries in the Iraq and Afghanistan wars. Among those with traumatic amputation from the war, 70% have been upper limb amputations, while 30% have been lower limb amputations. In contrast, in the general population, 95% of those amputations brought on by vascular disease have been of the lower limb, with upper limb amputations consisting of only 5%. Additionally, rates of vascular disease amputations rise steadily with age, particularly in those who are over 65 years old [3]. Due to the changing demographic of the United States population, by 2050, nearly two thirds of those with amputations will be over 65 years of age, compared to the almost equal split of those under and over 65 years old who live with amputations today [2].
Given the increased incidence of upper limb amputations, there is a growing need for occupational therapists to be more knowledgeable in understanding the training principles of conventional and advanced electric prosthetic technology. Significant research investments by the United States government and private manufacturers have resulted in dramatic improvements in upper limb body-powered and electrically controlled prosthetic components. With this emerging technology, it is essential for occupational therapy students to be kept abreast of new developments using comprehensive, meaningful and “hands-on” strategies that will prepare them to help their clients.
But what is the extent of prosthetic training in occupational therapy programs? The last nationwide survey of prosthetic training in OT programs in the United States was conducted in 1992 by Diane Atkins at the request of the National Center for Rehabilitation Research (NCMRR) at the National Institutes of Health (NIH). At that time, there were 76 institutions in 37 states offering Baccalaureate degrees, Post-Baccalaureate certificates, and Master’s degree programs in occupational therapy training programs. In that survey, it was reported that an average of 3 - 5 hours, of a typical occupational therapy program, was devoted to prosthetic training. The majority of the teaching experience in prosthetics was spent in lecture, in laboratory, viewing video tapes and listening to invited speakers. Atkins also found that OT students rarely worked in a hands-on manner with people with amputations.
We were interested in following up on Atkins’s previous findings to determine whether any major changes have occurred in the OT curriculum regarding prosthetic education. In an attempt to extend her initial survey, we were also interested in whether students have experience working with prosthetic simulators. It was argued many years ago that a simulated prosthesis could be used to help train physical and occupational therapists on the operational control of upper-extremity, body powered prostheses as well as provide insight into the physical and psychological challenges faced by the person with amputation [4]. A simulated prosthesis could be useful to parents of children with amputations in sensitizing them to difficulties in operating the device. Bitterman speculated that individuals with an amputation might use the device on their sound side while awaiting fabrication of the actual prosthesis to gain insight into its use [4]. In fact, evidence has been provided that bilateral transfer of this type can occur using a prosthetic simulator [5].
In summary, the major purpose of our survey was to establish whether the extent of OT training in prosthetics has changed since the Atkins survey [1]. In addition, we provide recommendations on how prosthetic training might be enhanced for OT students and professionals.
2. METHODS
Research Design. The current survey was designed to follow up on the original Atkins survey [1]. This survey was made available to Directors of occupational therapy programs throughout the United States and Canada. The survey utilized a cross-sectional research design that is typically used to determine the frequency or prevalence of a particular attribute [6].
Participants. The participants were OT Directors from OT schools throughout the United Stated and Canada who responded to the survey. This research project was conducted with respect to the ethical considerations and principles enunciated in the World Medical Association Declaration of Helsinki regarding human experimentation.
Procedures and Data Collection. The survey was located on a laboratory website at San Francisco State University (The Neuromuscular Control Laboratory). In June of 2011, emails were initially sent to the directors of the167 accredited masters and doctoral level OT programs in the United States and Canada using the information available at the American Occupational Therapy website (http://www.aota.org) and the Canadian Association of Occupational Therapists website (http://www.caot.ca). The emails asked the directors to participate and instructions were provided on how to access the survey. To help maximize the return rate, follow-up emails were sent to non-responding programs in August and November of 2011. Reminder emails have been shown to increase response rates for these types of surveys [7,8]. In pilot testing the survey, we estimated that the time to complete the survey was approximately 10 minutes. The survey questions are shown in the Appendix.
Data Analysis. For each cross-sectional question in the survey, the frequency of OT directors’ specific responses to each of the questions was tabulated. The comments made by the responding OT directors to the four open ended questions were tabulated and grouped into categories. The frequencies of responses made in the categories were then tabulated.
3. RESULTS
Fifty-two surveys were completed (all from Masters programs) for a response rate of 31% (similar to Atkins’ rate of return). Eighty five percent of the programs responded that prosthetics training was “very important/ important” and 14% responded that it was “somewhat important”. An overwhelming number of programs provide prosthetic training during related classes (62%), but few programs utilize a specific lecture in prosthetics (32%). Four percent of the programs provide no prosthetic training in their curriculum. Figure 1 indicates how prosthetic training is provided by those programs who offer it (see Figure 1). Most programs use lectures to provide prosthetic training. About half of the programs utilize hands-on prosthetic use with video and auditory tapes. A smaller percentage of the programs use a prosthetic simulator, incorporate clinic visits, have discussions with individuals with upper limb loss, and provide online supplements. One hundred percent of the programs devote <5% of the curriculum to prosthetic training.
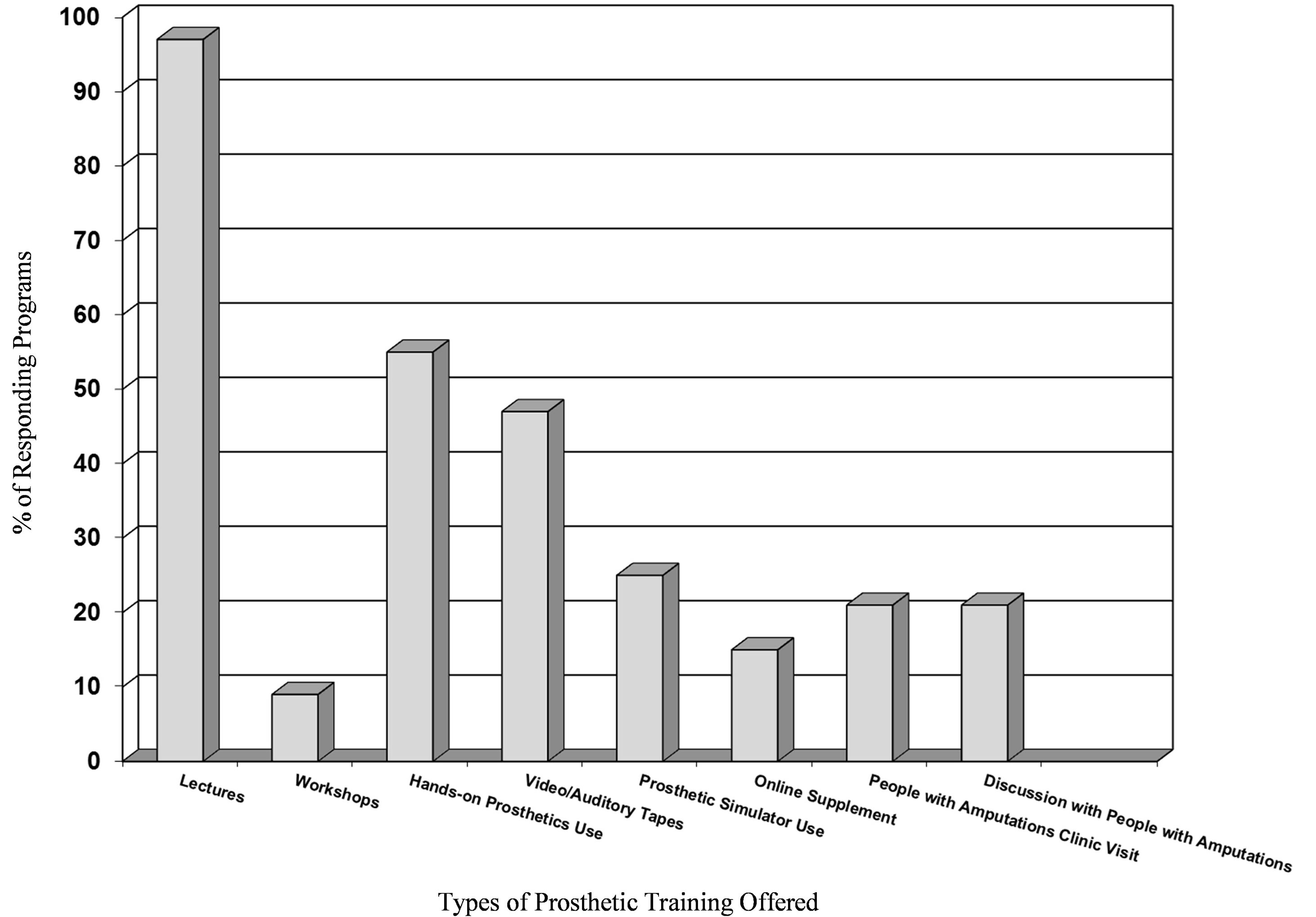
Figure 1. The percentage of responding masters level OT programs (n = 52) offering various types of training and teaching aids.
Figure 2 illustrates the number of hours of training devoted to prosthetics in the responding OT programs (see Figure 2). Nearly 60% of the programs devote 3 - 5 hours or less in the curriculum to prosthetic training. A much smaller percentage (19%) of programs offer 6 - 8 hours or more of prosthetic training. 69% of the programs focus on both upper and lower extremity prosthetics and 31% focus only on upper extremity prosthetics with no programs focusing only on lower extremity prosthetics. Of those programs devoted to both, an overwhelming number focus at least half or more of the time on upper extremity prosthetics. 98% of the programs focus on both body-powered and myoelectric prosthetics with only 2% focused on only body-powered.
Figure 3 provides information on the type of training that OT programs would like to add to their current curriculum (see Figure 3). The most popular addition would be the use of a prosthetic simulator. The next most popular addition would be more online supplements and actual interaction with upper limb amputees in the form of clinic visits or discussion. Finally, a slightly smaller percentage of the programs would like more hands-on prosthetic use, as well as the use of video and audio tapes.
The last part of the survey asked OT directors to provide the responses to the following open-ended questions. We attempted to categorize and quantify their answers.
1) Why do you think prosthetic training is important? Nearly 42% of the OT directors responded that students should have a basic knowledge of prosthetics. Nearly 38% responded that occupational therapists will encounter individuals with prosthetic devices and/or amputations throughout their career. A smaller percentage stated that occupational therapists play a major role in pre-prosthetic training, follow-up training, and prosthetic use in activities of daily living (ADL), and that there is an increased need for prosthetic training based on the increasing population of amputees (such as returning veterans).
2) Would the use of a prosthetic simulator facilitate prosthetic training? (YES/NO, please specify with details). Sixty nine percent responded “Yes”, and 19% responded that they already have a prosthetic simulator that is either “too simple, old or unsophisticated”. Seven percent responded “No”. Notable comments were:
● “A prosthetic simulator would be useful but these devices are often cost prohibitive”;
● “It is difficult for students to understand how prosthetic devices work without using one”;
● “Students learn empathy and understanding through using a prosthetic simulator”.
3) Would the student experience be enhanced by
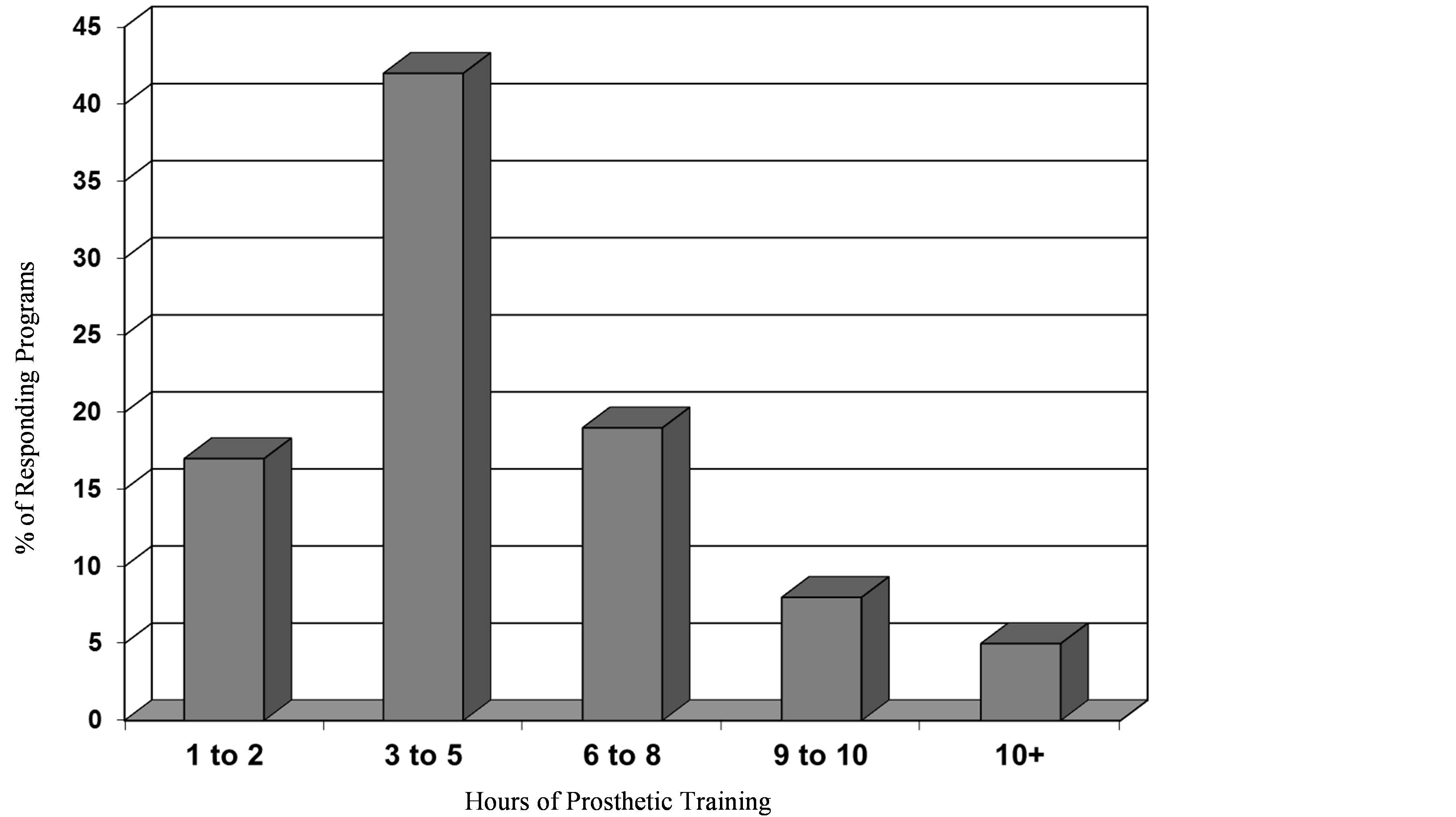
Figure 2. The percentage of responding masters level OT programs (n = 52) offering various hours of prosthetic training and teaching aids in their curriculum.
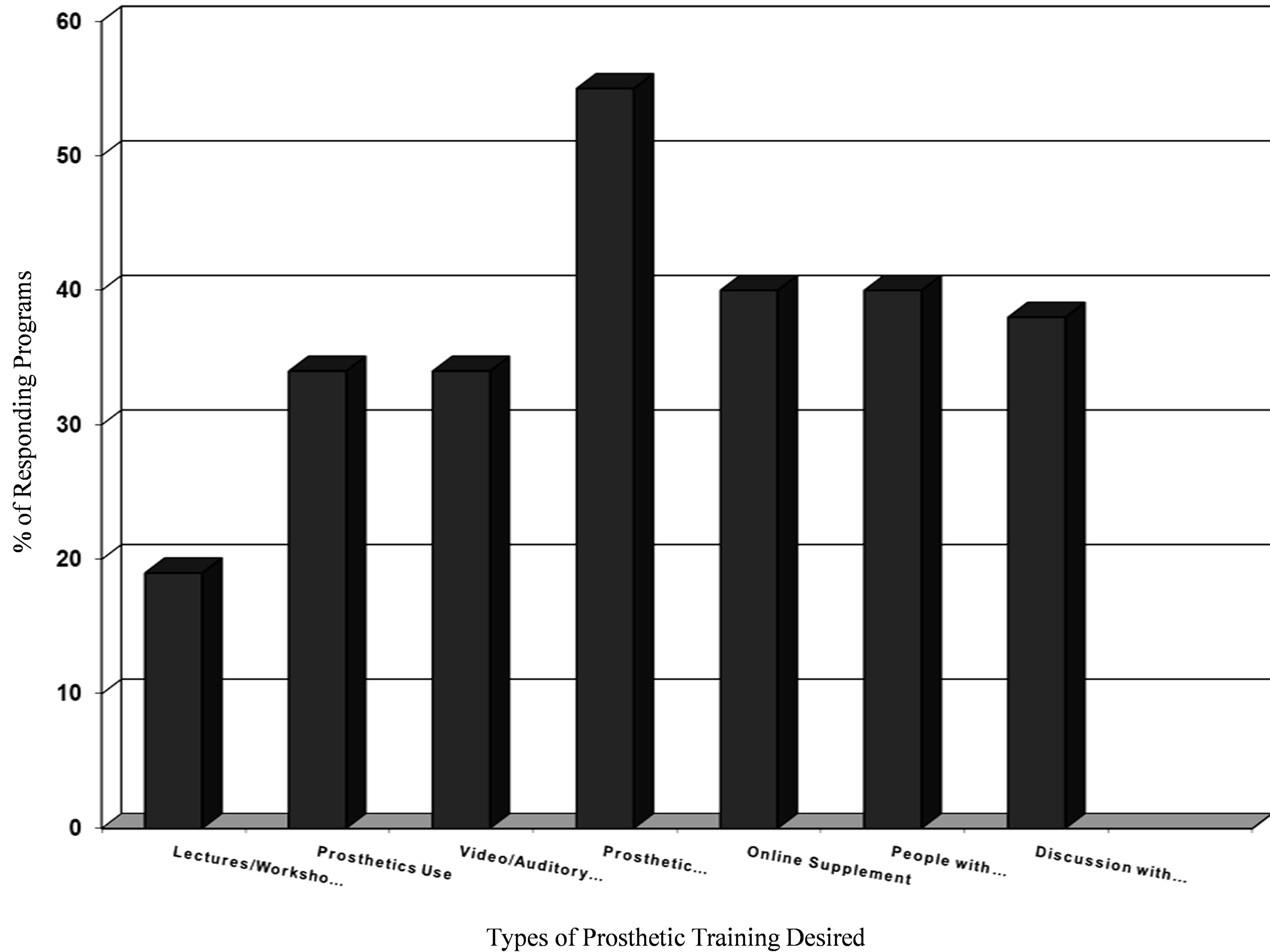
Figure 3. The percentage of responding masters level OT programs (n = 52) desiring various types of training and teaching aids.
additional prosthetic training? Eighty eight percent responded “Yes”, or probably, <4% responded “No”, 21% responded there was not enough time in the curriculum to devote to prosthetic training and something else in the curriculum would have to be cut to make room for prosthetic training. Only 7% responded that adequate training is already provided.
4) What changes would you recommend to future prosthetic training and design? Thirteen per cent of the OT directors who responded to this question said that more repository materials should be available for teaching. Four of the directors suggested more case study-based learning. Other suggestions were more and better videos, more online material, more hands-on experience with prosthetic simulators and an increase in interaction with professionals and clients in the prosthetic community.
4. DISCUSSION
The current survey indicates that a large percentage (60%) of the OT programs devote only 3 - 5 hours or less to prosthetic training. One hundred percent of the programs devote <5% of their entire curriculum to prosthetic training. These results are very similar to those found by Atkins (1992) over 20 years ago [1]. It is safe to conclude the amount of time spent on prosthetic training in OT programs has not significantly changed over this time period. Only a few programs devote more time to prosthetics in their curriculum, though it is not clear why some programs offer more prosthetic training than others. This disparity is not due to a lack of interest in prosthetics or to the perception that prosthetic training is unimportant as evident from the questionnaire and open-ended questions. Eighty five per cent of the programs responded that prosthetics training was “very important/important” and 14% responded that it was “somewhat important”. In the open-ended questions the OT directors provided a number of reasons why they thought prosthetic training was important. One possible reason for the limited training in most programs is that prosthetic training may not be considered a high priority, despite its perceived importance, because of the sheer volume of topics covered in contemporary OT curriculums. One limitation of our survey is that we did not ask the OT directors to prioritize the content of their curriculum. Another possible reason for the limited training is that prosthetic training has not historically been a major part of the OT curriculum and it may have been difficult to add it to an already comprehensive program that focuses on more traditional areas.
How is prosthetic training administered in OT programs, and are there aspects of the training that OT directors would like to see enhanced? Most programs use a lecture style format for prosthetic training, but audio and video tapes are also used to deliver information on prosthetics. In some programs, actual or simulated prostheses are used to enhance instruction. However, only a small percentage of programs allow for students to interact with actual prosthetic users in their classes (21%) or during clinical visits (21%). Furthermore, only 32% of the programs have a class strictly devoted to prosthetics. Most OT programs embed their prosthetic training in other related classes.
What kinds of curricular aids could help improve the curriculum in prosthetic training? The OT directors responded that the single most important addition would be the use of a prosthetic simulator. While a quarter of the programs use such a device, over half of the directors believe adding a prosthetic simulator to their curriculum would be desirable. This finding reflects the argument made by Bitterman (1968) many years ago that the prosthetic simulator can be used to help train physical and occupational therapists on the operational control of upper-extremity, body powered prostheses [4]. To our knowledge, however, there are no prosthetic simulators on the market readily available to OT programs. It is likely that most simulators are locally made, or manufactured in-house by the OT programs. Clearly, a prosthetic simulator that uses similar components and motions to control (e.g. prehensor, cabling system, shoulder harness) a prosthesis used by a person with an amputation would be desirable. In addition, a simulator that could be adapted to different arm dimensions, across different users, right and left sides, and also different functions such as voluntary opening and voluntary closing would be desirable.
5. RECOMMENDATIONS
Based on the results of this survey, we believe that prosthetic training in OT schools of higher learning is inadequate given the prevalence of upper limb loss and the emerging technological advances that have occurred in this field within the past 5 years. It is incumbent upon OT schools to expose the OT student to both conventional, body-powered, as well as advanced state-of-the-art electric prostheses. However, several of the OT directors responded that there is simply not enough time in their current curriculum to add or increase prosthetic training. One option, suggested by Atkins [1], is to offer 1 - 2-day prosthetic workshops directly to the OT class at the college and university level. Or, if, sanctioned by the American Occupational Therapy Association (AOTA), more advanced workshops could be offered in various cities throughout the United States that would allow the OT student and practitioner to be exposed to a more advanced prosthetic training experience. While only 9% of the OT programs responded that they include workshops in their curriculum, nearly 20% responded that adding workshops would be desirable. This type of extracurricular workshop could take many forms and include a wide range of topics. For example, a prosthetic workshop could certainly include the description of various types of prosthetic devices most commonly used in the clinical environment to help increase the student’s knowledge of the various component parts of the device and their function. As indicated by the results of a different survey [9], people with amputations who use a prosthesis are not only aware of the components of a prosthesis but also can evaluate the effectiveness of these components. A better understanding of the component parts of the prosthesis and their function gained through participation in a prosthetic workshop would also benefit the OT student and practitioner allowing them to better address the needs of individuals with upper limb loss. Prosthetic simulators could feature prominently in workshops by providing practitioners with firsthand experience using the three commonly used prosthetic devices (cosmetic, body-powered, and myoelectric). This segment of the workshop would ideally consist of devoting a portion of the curriculum to becoming somewhat proficient with various simulated prosthetic devices, including those of both the transradial (TR) and transhumeral (TH) varieties. Most adults become minimally proficient with prosthetic devices after 5 to 10 hours of continuous use [10]. Ideally the OT student or practitioner should reach this level of proficiency as well. This could be accomplished by acquainting the student with the basic operations of the prosthesis during the workshop and then making the simulators available to “check out” at the student’s home institution. We feel that it is necessary for the OT student and therapist to have firsthand acquaintance with the devices to develop realistic expectations about the capabilities and limitations of the devices. In developing this rationale, we feel that the therapists will be able to better convey this information to the patient, thereby reducing the risk of unrealistic expectations and rejection of the device altogether [1].
These workshops could include other training supplements desired by the OT directors, audio and video tapes, on-line supplements and even visitations by people with amputations. Offering live and perhaps even online workshops that could lead to special certification is one way to address the obvious need for OT students and professionals to increase their knowledge and understanding of prosthetics.
Implications for Occupational Therapy Education and Practice:
● The emerging field of technologically advanced upper limb prostheses places occupational therapists “on the front line” of ensuring that individuals with upper limb loss are comprehensively trained in prosthetic utilization.
● Occupational Therapy colleges and universities offer, on average, only 3 - 5 hours of lectures and overview of the upper limb amputation experience, and the prosthetic training that is required to utilize these prostheses effectively.
● Sixty-nine percent of the respondents indicated that prosthetic simulators would add to the student’s learning experience. Additional videos and learning materials could be developed by skilled upper limb practitioners that could be incorporated in the occupational therapy curriculum.
● Additional exposure to upper limb amputee rehabilitation could be offered in 1 - 2-day workshops that could be given at OT schools of higher learning. These workshops could include an invitation to local OT practitioners as well. Experienced upper limb prosthetists, physicians and experienced occupational therapists could demonstrate the team approach. Individuals with upper limb amputations would be included in this comprehensive experience as well.
● As a result of these recommendations, occupational therapy students would be better prepared to meet the challenges of this advanced technology, and better informed as to how to approach and train the upper limb amputee in a more skilled and knowledgeable manner.
ACKNOWLEDGEMENTS
The results of this manuscript were presented at the AOTA annual conference at San Diego, April 27, 2013.
REFERENCES
- Atkins, D.J. (1992) Training in prosthetics and orthotics: The occupational therapy experience. Prosthetic and Orthotic Research for the Twenty-First Century: Report of a Research Planning Conference, Bethesda, 23-25 July 1992, 55-60.
- Ziegler-Graham, K., MacKensie, E.J., Ephraim, P.L., Travison, T.G. and Brookmeyer, R. (2008) Estimating the prevalence of limb loss in the United States: 2005-2050. Archives of Physical Medicine and Rehabilitation, 89, 422-429. http://dx.doi.org/10.1016/j.apmr.2007.11.005
- Dillingham, T.R., Pezzin, L.E. and MacKenzie, E.J. (2002) Limb amputation and limb deficiency: Epidemiology and recent trends in the United States. Southern Medical Journal, 95, 875-883.
- Bittermann, P. R. (1968) An upper-extremity prosthesis for the non-amputee. The American Journal of Occupational Therapy, 23, 210.
- Weeks, D.L., Wallace, S.A. and Anderson, D.I. (2003) Training with an upper-limb prosthetic simulator to enhance transfer of skill across limbs. Archives of Physical Medicine and Rehabilitation, 84, 437-443. http://dx.doi.org/10.1053/apmr.2003.50014
- Lavrakas, P.J. (2008) Encyclopedia of survey research methods. Sage Publications, Inc., Thousand Oaks.
- Sheehan, K.B. and Hoy, M.G. (1997) E-mail surveys: Response patterns, process and potential. Proceedings of the 1997 Conference of the American Academy of Advertisers.
- Sheehan, K.B. and McMillan, S.J. (1999) Response variation in e-mail surveys: An exploration. Journal of Advertising Research, 39, 45-54.
- Atkins, D.J., Heard, D.C.Y. and Donovan, W.H. (1996) Epidemiologic overview of individuals with upper-limb loss and their reported research priorities. Journal of Prosthetics and Orthotics, 8, 2-11. http://dx.doi.org/10.1097/00008526-199600810-00003
- Carroll, K. and Edelstein, J. (2006) Prosthetics and patient management: A comprehensive clinical approach. Slack Incorporated, Thorofare.
APPENDIX
● Occupational Therapy Survey Questions
● What is the name of your Institution? (While we asked for the name of the institution, our email to the Directors made it clear that institution names would be kept anonymous in any related reports or manuscripts).
● Program Type (Masters/Doctoral)
● How important is training in prosthetics to an Occupational Therapist? (Very Important, Important, Somewhat Important, Not Important)
● How do you provide training in prosthetics?
o Not at all o Specific required class o Specific elective class o During other related classes o Other
● Does your training include? (check all that apply):
o Lectures o Workshops o Hands-on prosthetic use o Video and auditory tapes o Prosthetic Simulator o Use Online supplement o People with amputations clinic visit o Discussion with people with amputations o Other__________________
● What percentage of your total curriculum is devoted to training in prosthetics?
o <5% o 5% o 10% o 15% o 20% o 25+%
● How much time is devoted to training in prosthetics?
o 1 - 2 hours o 3 - 5 hours o 6 - 8 hours o 9 - 10 hours o 10+ hours
● Is your program focused on upper extremity, lower extremity or both?
● If your program is devoted to BOTH, what % of time is devoted to upper-limb? (10%, 20%, 30%, 40%, 50%, 60%, 70%, 80%, 90%)
● What type of prosthetic use is covered in your program?
o Body-Powered o Myoelectric o Both
● Which of the following would you be interested in adding to your training? : Lecture Workshops o Hands-on prosthetic use o Video and audio tapes o Prosthetic simulator use o Online supplement o People with amputations o clinic visits o Discussion with people with amputations o Other ___________________
● Why do you think prosthetic training is important? (open-ended)
● Would the use of a prosthetic simulator facilitate prosthetic training? (YES/NO, please specific with details) (open-ended)
● Would the student experience be enhanced by additional prosthetic training? (open-ended)
● What changes would you recommend to future prosthetic training and design? (open-ended)

