Open Journal of Clinical Diagnostics
Vol.3 No.3(2013), Article ID:37212,7 pages DOI:10.4236/ojcd.2013.33015
Sonographic evaluation of the post-operative rotator cuff: Does tendon thickness matter?
![]()
1Radiology Department, Clinique Mutualiste La Sagesse 4 Place Saint Guénolé, Rennes, France
2Orthopaedic Department, Clinique Mutualiste La Sagesse 4 Place Saint Guénolé, Rennes, France
3Texas A&M Health Sciences Center, Temple, USA
4Sport Medicine Department, Clinique Mutualiste La Sagesse 4 Place Saint Guénolé, Rennes, France
Email: *jeremy.lasbleiz@gmail.com
Copyright © 2013 J. Lasbleiz et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 13 May 2013; revised 13 June 2013; accepted 20 June 2013
Keywords: Rotator Cuff; Sonography; Postoperative Imaging; Arthroscopy; Postoperative Evaluation
ABSTRACT
The goal of this work is to determine whether sonographic measures of tendon thickness correlate with post-operative functional parameters or re-tear rates. 53 consecutive patients with supraspinatus tears on MRI were examined by an orthopedic surgeon to determine: preand post-operative patient pain (via Constant-Murley scale), night time pain, maximum force production by the affected arm (in pounds), and range of motion deficits. Post-operative ultrasound at 3 and 12 months following surgery was performed to evaluate for recurrent tear and to measure tendon thickness. Post-operative tendon thickness was inversely related to patient age (r = −0.24; p < 0.05). Statistically significantly decreased thickness was observed with Snyder type C lesions (4.2 mm versus 5.1 mm for type A and B; p < 0.05). Tendon thickness decreased post-operatively from 3 to 12 months (r = −0.31; p < 0.05). Only two recurrent tears occurred, preventing statistical assessment of the prognostic value of tendon thickness. Post-operative tendon thickness did not successfully predict post-operative functional outcomes or pain levels (p > 0.05). Normal postoperative tendon thickness of the rotator cuff decreases from 3 to 12 months following surgery. Thickness is reduced in patients with more severe tears and in older patients but does not correlate with post-operative patient pain or functional outcomes.
1. INTRODUCTION
Recurrent rotator cuff tears following primary repair remain a relatively common event. The incidence of rotator cuff retear following injury varies widely in the literature ranging from 14% to 94% [1-3]. As such, the imaging evaluation of the post-operative rotator cuff remains critical. However, imaging of the post-operative rotator cuff presents a number of unique challenges. While MRI identifies pre-operative rotator cuff tears with high diagnostic accuracy, the technique is often limited secondary to metallic susceptibility artifact and the potentially confounding appearance of associated granulation and inflammatory tissue [4].
Ultrasound has been suggested as a cost-effective alternative to MR for evaluation of the rotator cuff allowing a dynamic functional as well as structural evaluation [5]. In the post-operative setting, the presence of a gap or defect within the cuff tendon by sonography has long been recognized as a reliable indicator for cuff re-tear [6]. However, the normal post-operative appearance of the rotator cuff has not yet been assessed in detail.
A number of previous studies have attempted to correlate imaging parameters with functional outcomes following rotator cuff repair [7-9]. For the most part such attempts have been unsuccessful. Recently, a group of authors examined several MR parameters, including tendon thickness and signal intensity, in a cohort of postoperative patients [10]. In that study, no statistically significant correlation was seen between any MRI parameter and clinical outcome.
Because ultrasound allows for a real-time, dynamic evaluation of the rotator cuff with greater spatial resolution than MRI, ultrasound may offer a more detailed evaluation of the rotator cuff. The aim of the present study is to extend the investigation of the aforementioned work, examining the normal post-operative appearance of the rotator cuff tendons sonographically. We hypothesize that imaging parameters, specifically tendon thickness, will correlate with clinical outcome when assessed sonographically due to the real-time evaluation and increased spatial resolution of ultrasound relative to MRI.
2. MATERIALS AND METHODS
2.1. Study Population
This study was approved by the local institutional review board (IRB) and we received informed consent from each participant in our study. Patient recruitment occurred from September 2009 to November 2010. 53 consecutive patients diagnosed with supraspinatus or combined supraspinatus and infraspinatus tears by shoulder MR were included. Inclusion criteria were the presence of a full or partial thickness tear confirmed on pre-operative shoulder Arthro-CT. Exclusion criteria included patients under the age of 18 and patients in which surgery was contraindicated (i.e. irreparable or subscapularis tears, previous surgery).
2.2. Pre-Operative Evaluation
The patients were assessed pre-operatively by an orthopedic surgery with 25 years of experience. The patient was asked to identify the delay (in days) between their initial injury and clinical presentation. Pre-operative daytime and night time pain were assessed. Maximum preoperative force on a JOB-Test movement under resistance of both arms was assessed with a KERN CH50 K50 device (KERN & Sohn Gmbh, D-72336 Balingen Germany). This device reports maximum force in pounds (lbs). The strength of the arm affected by the rotator cuff tear was denoted by a ratio of the maximum force produced by the affected arm to the maximum force generated by the contralateral arm.
2.3. Operative Evaluation
All patients underwent surgery performed by a single orthopedic surgeon. The supraspinatus tendon tear was staged surgically utilizing the Synder classification (Southern Californian Orthopedic Institute, SCOI, classification system) [11]. In this system, type A tears involve the articular surface, type B tears the bursal surface, and type C tears are complete. The tears were repaired via arthroscopicsurgery utilizing a standard technique [12,13]. The number of helical and Versalok (Depuy Orthopaedics Warsaw, IN) anchors utilized were recorded.
2.4. Post-Operative Evaluation
The post-operative evaluation was performed by an independent physician one year following surgery (Range: 332 to 385 days). Force and deficit measurements were conducted similarly. The patient was asked if they experienced night time pain. Daytime pain was graded via the pain component of the Constant-Murley score on a scale of 0 (no pain) to 15 (severe pain) [13].
2.5. Imaging Evaluation
Radiographic evaluation of the shoulder was performed on average at 1 month following surgery (mean 32 days, range 28 to 35 days). These were interpreted by a single radiologist with 10 years experience. On the outlet frontal view, the subacromial interval was calculated in millimeters. On the same view, the scaphohumeral arch variance was measured (Figure 1). A repeat radiographic examination was performed 11 months later (mean 333 ± 46.6 days later) at the time of the patient’s 1 year clinical followup. At approximately 3 months (range: 84 to 97 days) and 1 year following surgery a sonographic evaluation was performed of the rotator cuff by the same radiologist. The 1 year post-surgery follow-up was performed on the same day of the patient’s clinical follow-up. The sonography machine was a Voluson E8 General Electric (first date of use September 2008). Standardized positioning was utilized for the sonographic evaluation performed for assessment of supraspinatus tendon thickness. The supraspinatus tendon thickness was assessed in a paracoronal slice with the ultrasound probe aligned with the greater tuberosity. Maximum supraspinatus tendon thickness was determined sonographically as illustrated in Figure 2.
2.6. Statistical Analysis
As the number of recurrent rotator cuff tears was low (n = 2), for statistical analysis, tendons exhibiting re-tears were excluded so as not to confound results. Means and standard deviations were calculated for each variable. All
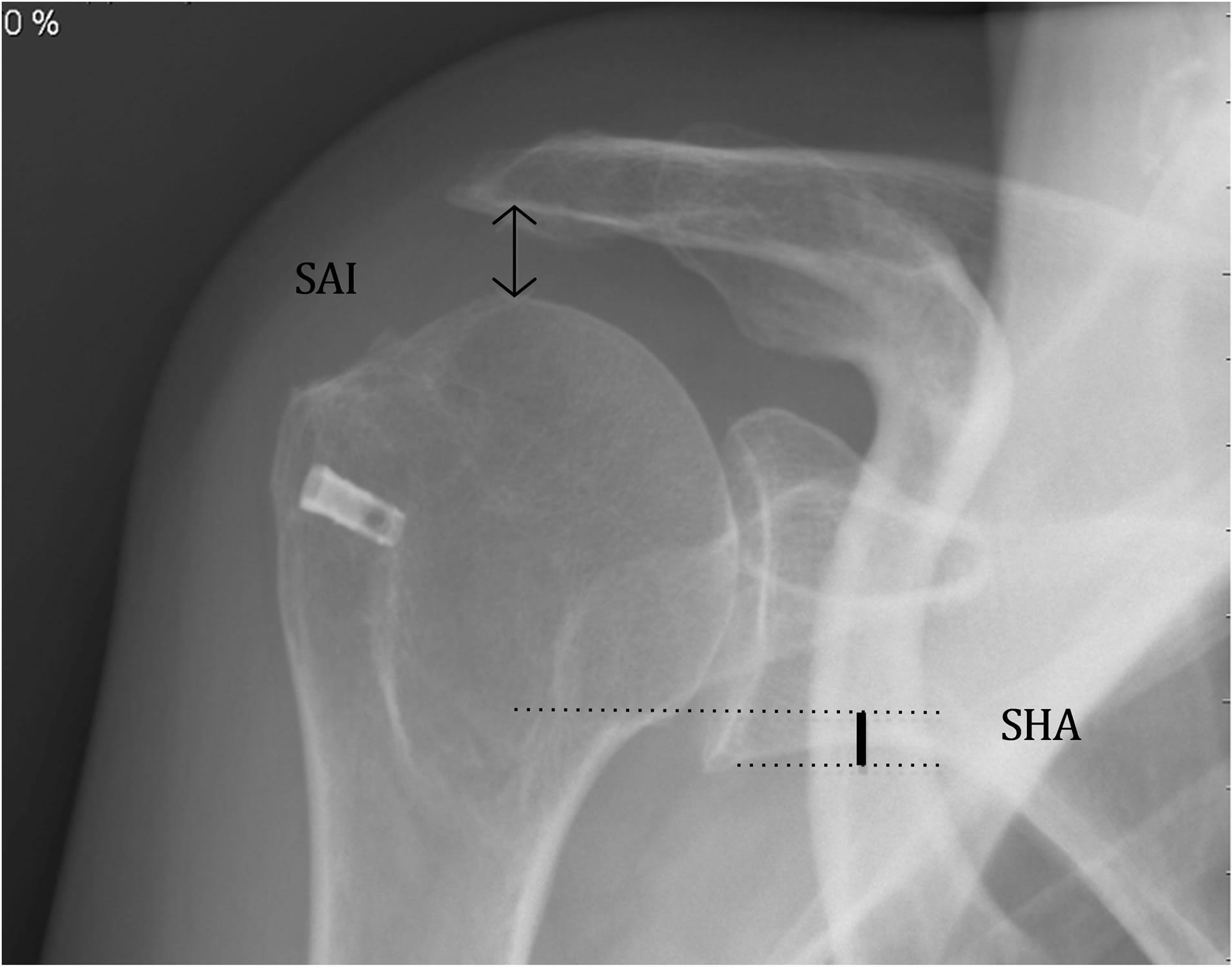
Figure 1. Postoperative radiography of the shoulder, frontal view with measurement of the subacromial interval (SAI, arrow) the scapulo-humeral arch (SHA, line).
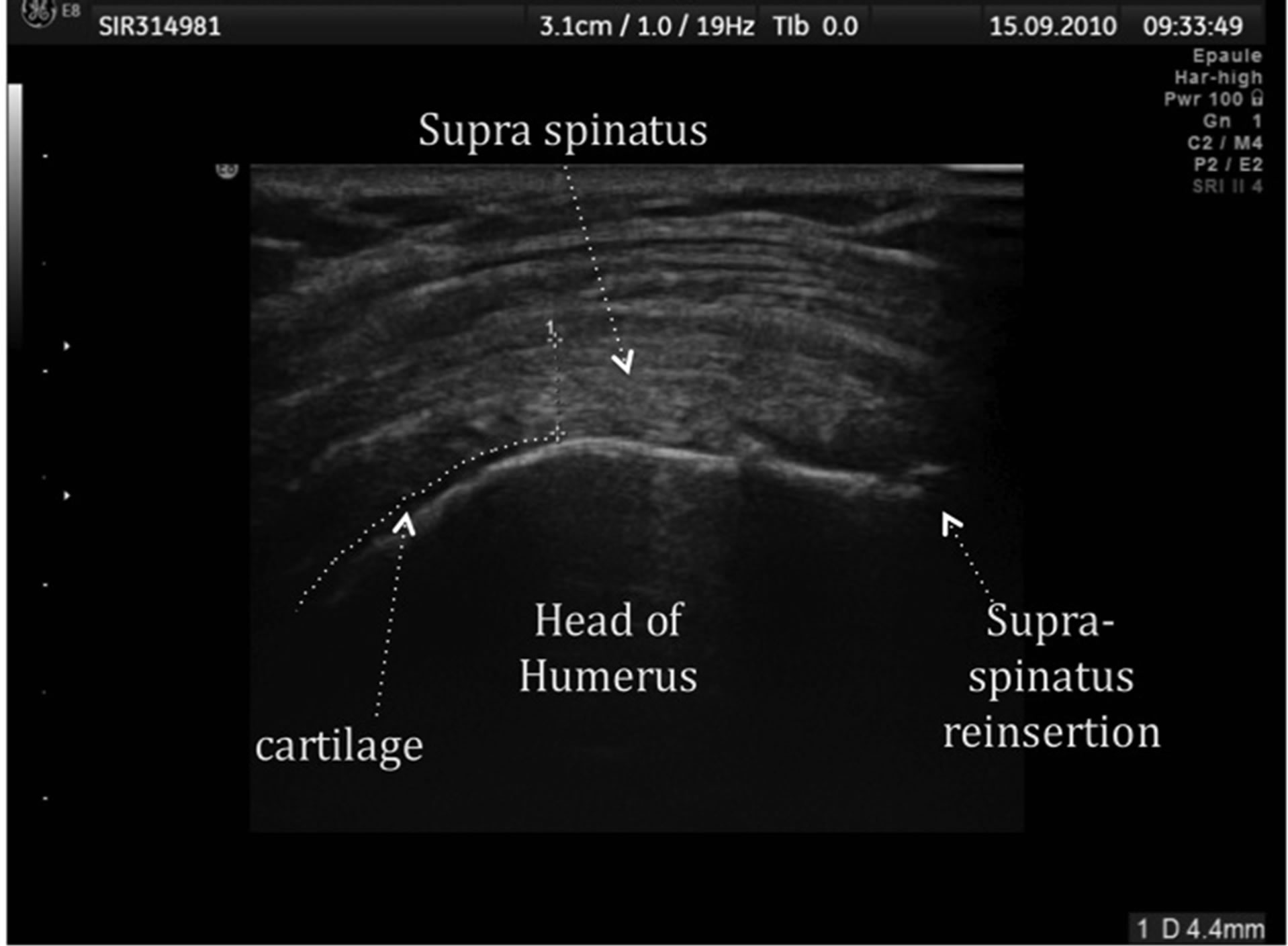
Figure 2. Paracoronal sonographic image on which supraspinatus tendon thickness measurements were obtained.
calculations were performed in SPSS (v16.0). For all statistical analyses p-values less than 0.05 were taken to be statistically significant. A paired t-test was used to assess differences in imaging parameters (tendon thickness and radiographic measurements), clinical deficits, and clinical force at the different time points at which these variables were assessed. A Pearson correlation was performed assessing change in tendon thickness over time versus the delay between sonographic evaluations. Similar correlations were performed between tendon thickness and patient age, post-operative deficit, and postoperative maximum force. Differences in deficits, force, and tendon thickness were compared among Synder classification categories preand post-treatment utilizing a repeated measures 1-way ANOVA test with a post-hoc least square differences test. Tendon thickness of patients with residual diminished force and residual pain was compared to those of patients without these attributes.
3. RESULTS
Of the 53 patients, 21 women and 32 men were included in the statistical analysis. Two men in the study (3.6% = 2/55) experienced a re-tear during the course of the study. The mean patient age was 59.3 years (range: 41 - 73 years). 12/53 (22.6%) of lesions were diagnosed as Snyder type A lesions at surgery, 25/53 (47.2%) as type B lesions, and 16/53 as type C lesions (30.2%). The mean duration between followup sonographic examinations was 273.7 ± 8.4 days and 305.8 ± 18.0 between radiographic exams.
3.1. Clinical Parameters
Pre-operative force assessed relative to the contra-lateral extremity was 59.7% ± 3.9% versus post-operative force of 85.6% ± 1.8%. This increase was statistically significant (p < 10−5). Changes in force by lesion type are detailed in Figure 3.
A statistically significant effect was seen between preand post-operative values (p < 10−3); however, no statistically significant differences were seen between Snyder lesion types (p > 0.2). Pre-operative deficit was 42.4% ± 3.3% versus 16.2% ± 1.9% post-operative (p < 10−8). Changes in deficits by lesion type are detailed in Figure 4. A statistically significant effect was seen between preand post-operative values (p < 10−3), and type C lesions demonstrated greater deficits than type B lesions (p < 0.05). Pre-operatively, all patients reported daytime pain (53/53 = 100%) and 96% (51/53) nighttime pain. Post-operatively, 45.2% (24/53) of patients experienced daytime pain and 13.2% (7/53) experienced nighttime pain. Post-operative pain was experienced in 58% (7/12) of Synder class A patients, 44% (11/25) of Synder class B patients, and 37.5% (6/16) of Synder class C patients. Average post-operative pain level did not statistically significantly differ among patients (Synder A = 1.6, Synder B = 1.0, Synder C = 1.5; p > 0.05).
3.2. Imaging Evaluation
The subacromial (RadTAC) and scaphohumeral arch (RadCINT) intervals were not statistically significantly different between either Snyder classification groups at
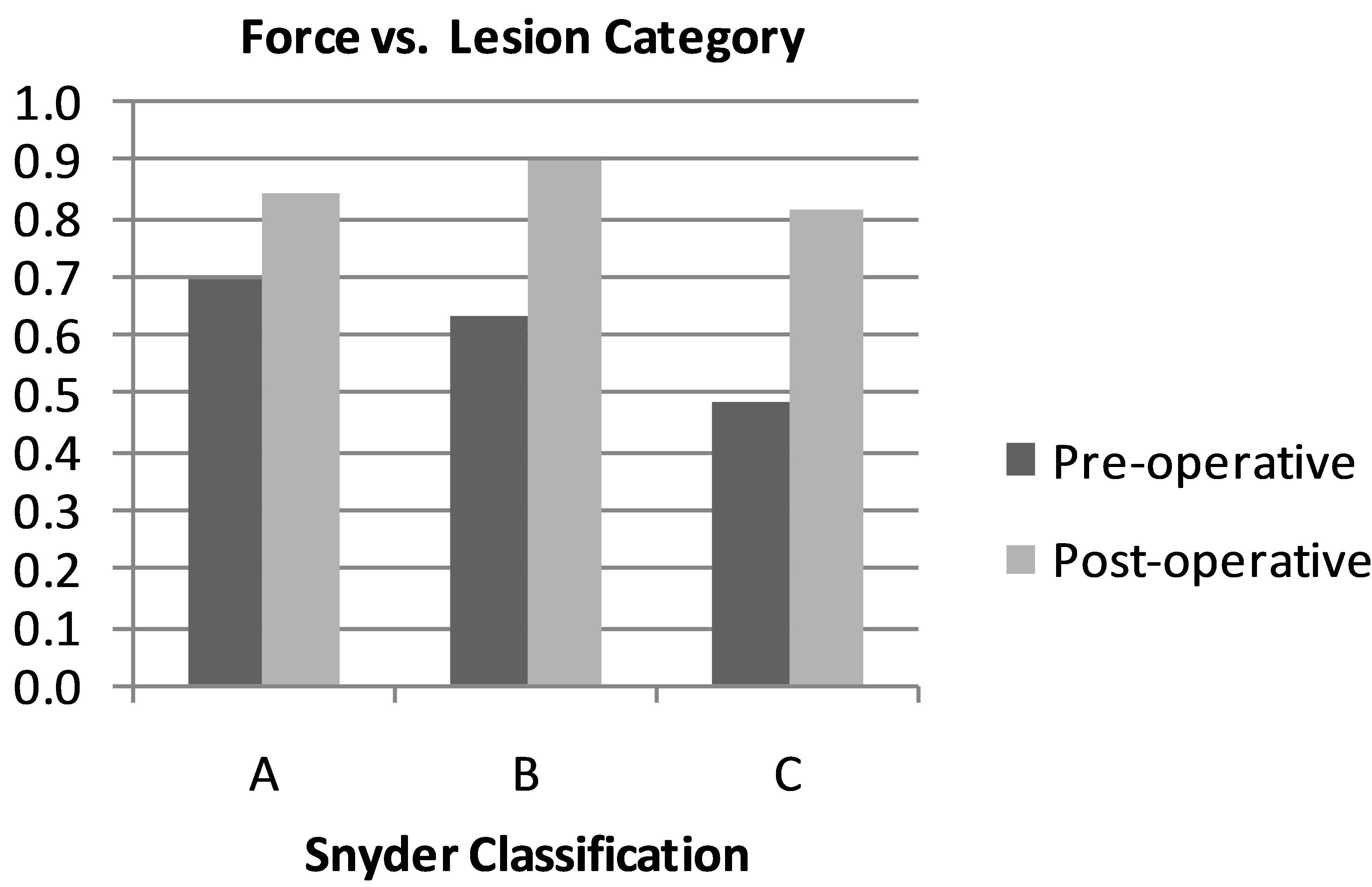
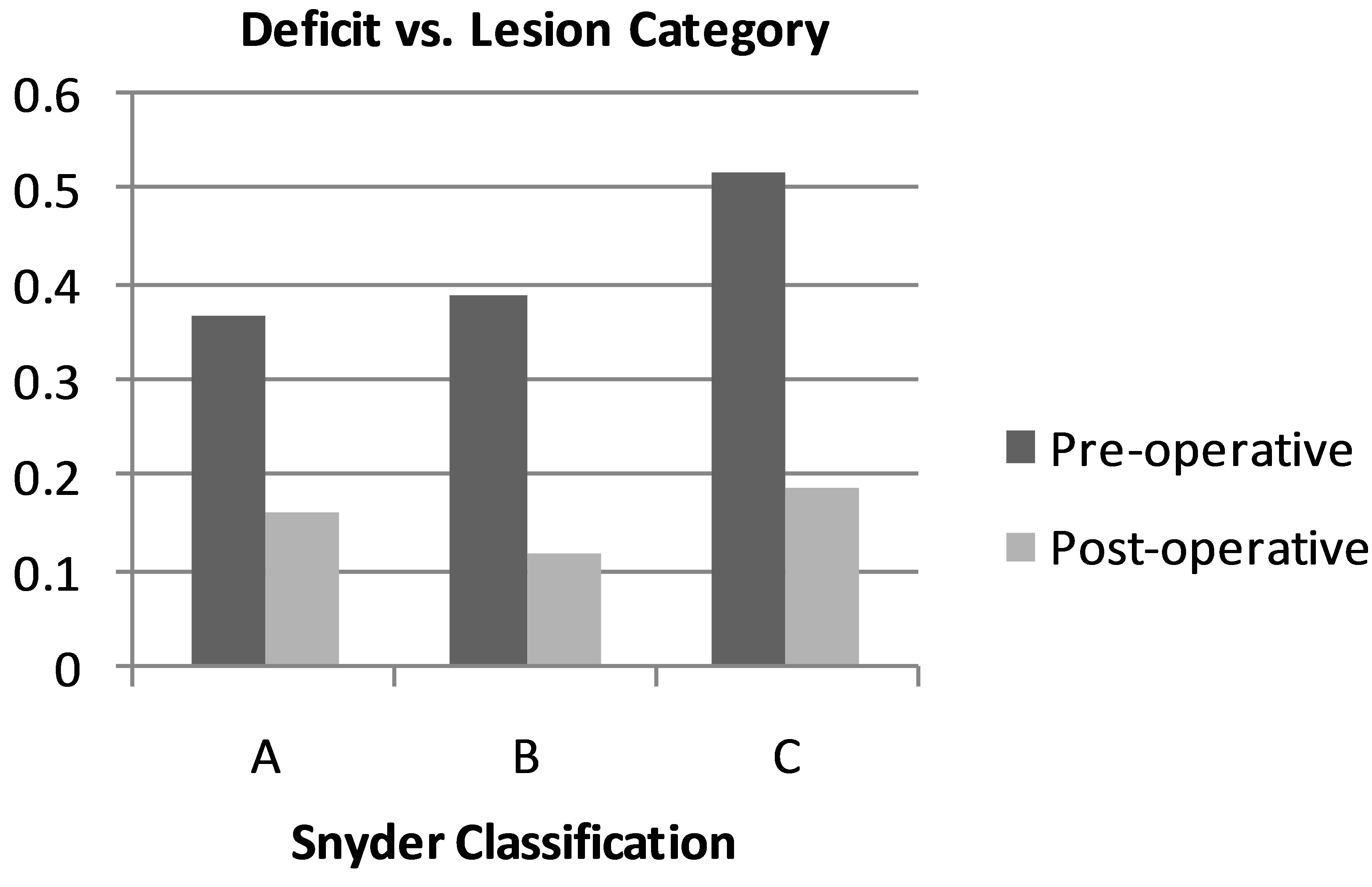
Figure 3. Changes in force, as measured relative to strength of the contralateral arm, and deficit preand post-operatively among the classes of rotator cuff tears observed.
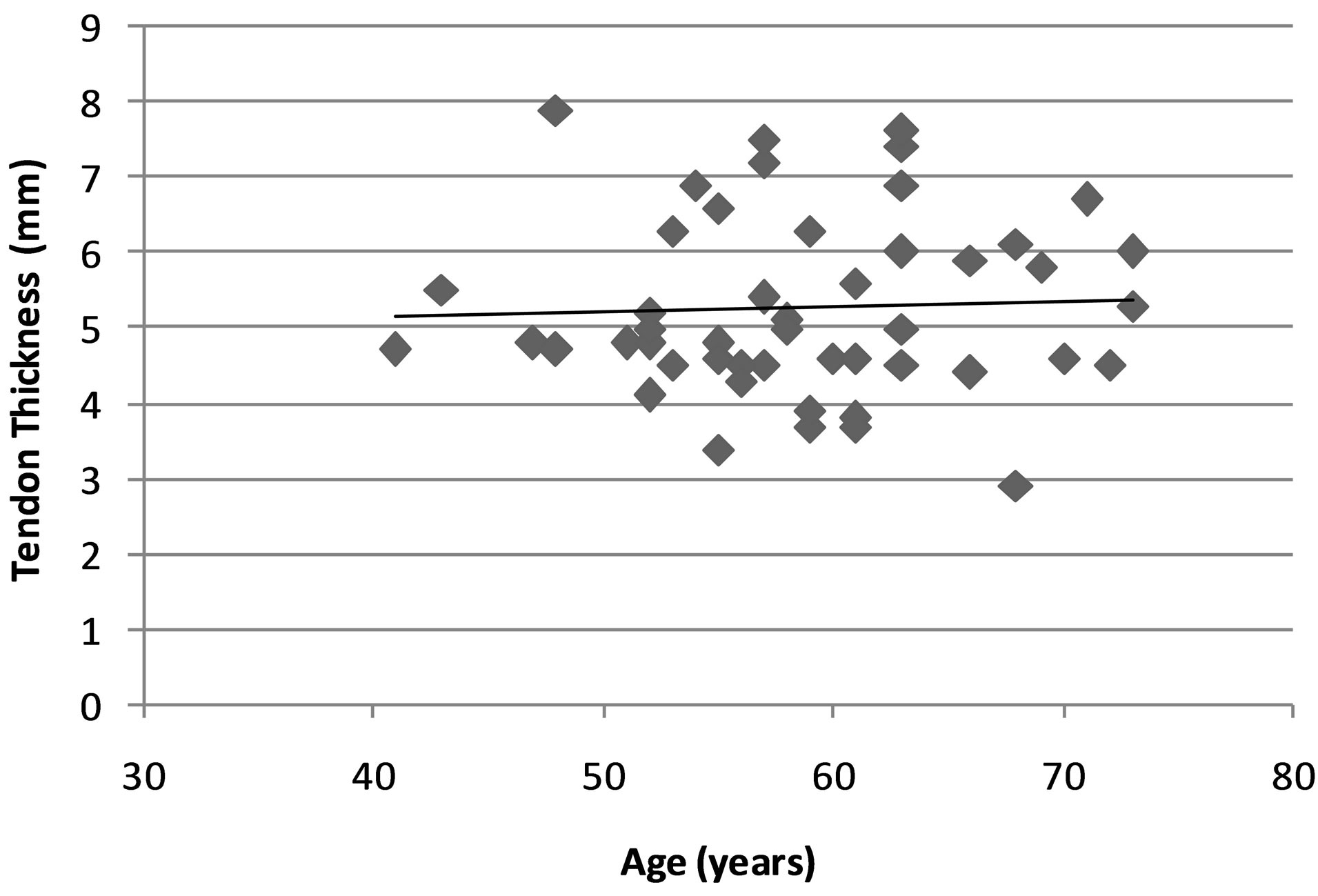
Figure 4. Tendon thickness versus patient age at 3 month postoperative followup. No statistically significant correlation was observed (p > 0.05).
either evaluated time point. This is detailed in Table 1.
The relationship between patient age and post-operative tendon thickness was first examined. There was no statistically significant correlation between patient age and post-operative tendon thickness at 3 months (r = 0.02; p = 0.8) as shown in Figure 5. There was a statistically significant inverse relationship between patient age and post-operative tendon thickness at 1 year (r = −0.24; p < 0.05) as illustrated in Figure 6.
Tendon thickness was assessed at 3 and 12 months for each Snyder classification group. No statistically significant effect was seen between 3 and 12 month post-operative values (p = 0.1). Statistically significantly lower tendon thickness values were seen with Snyder type C lesions versus type A and B lesions (p < 0.05). This is illustrated in Figure 7. An inverse correlation between tendon thickness and time between measurements was observed (r = −0.31, p < 0.05) as shown in Figure 8. There was no statistically significant difference in tendon thickness at either evaluated time point in patients with or without post-operative pain (time 1: p = 0.3, time 2: p = 0.9). This is illustrated in Figure 8. A non-statistically significant inverse correlation was seen between 3-month tendon thickness and residual pain scale rating (r = −0.21; p = 0.14). No statistically significant correlation was observed between 1 year tendon thickness and pain scale rating (r = −0.05 p = 0.7). No statistically significant correlation was observed between post-operative force at 3 months (r = 0.16; p = 0.3) or 1 year (r = 0.1; p = 0.4). No statistically significant differences were seen in 3- month or 1 year tendon thickness between patients with complete recovery of force (respectively, 5.6 ± 0.3 mm and 4.7 ± 0.3 mm) and a residual strength deficit (respectively, 5.2 ± 0.2 and 4.9 ± 0.1; p = 0.3). No statistically significant correlation was observed between post-operative deficit at 3 months (r = −0.15; p = 0.3) or 1 year (r = −0.12; p = 0.4).
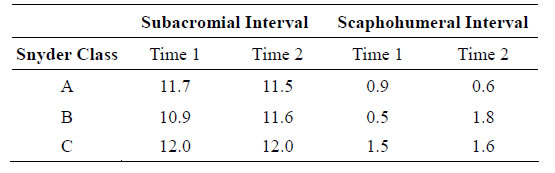
Table 1. Radiological measurements: subacromial space and scapulohumeral variance by lesion type.

Figure 5. Tendon thickness versus patient age at 1 year postoperative follow-up. A statistically significant inverse correlation was observed (p < 0.05).
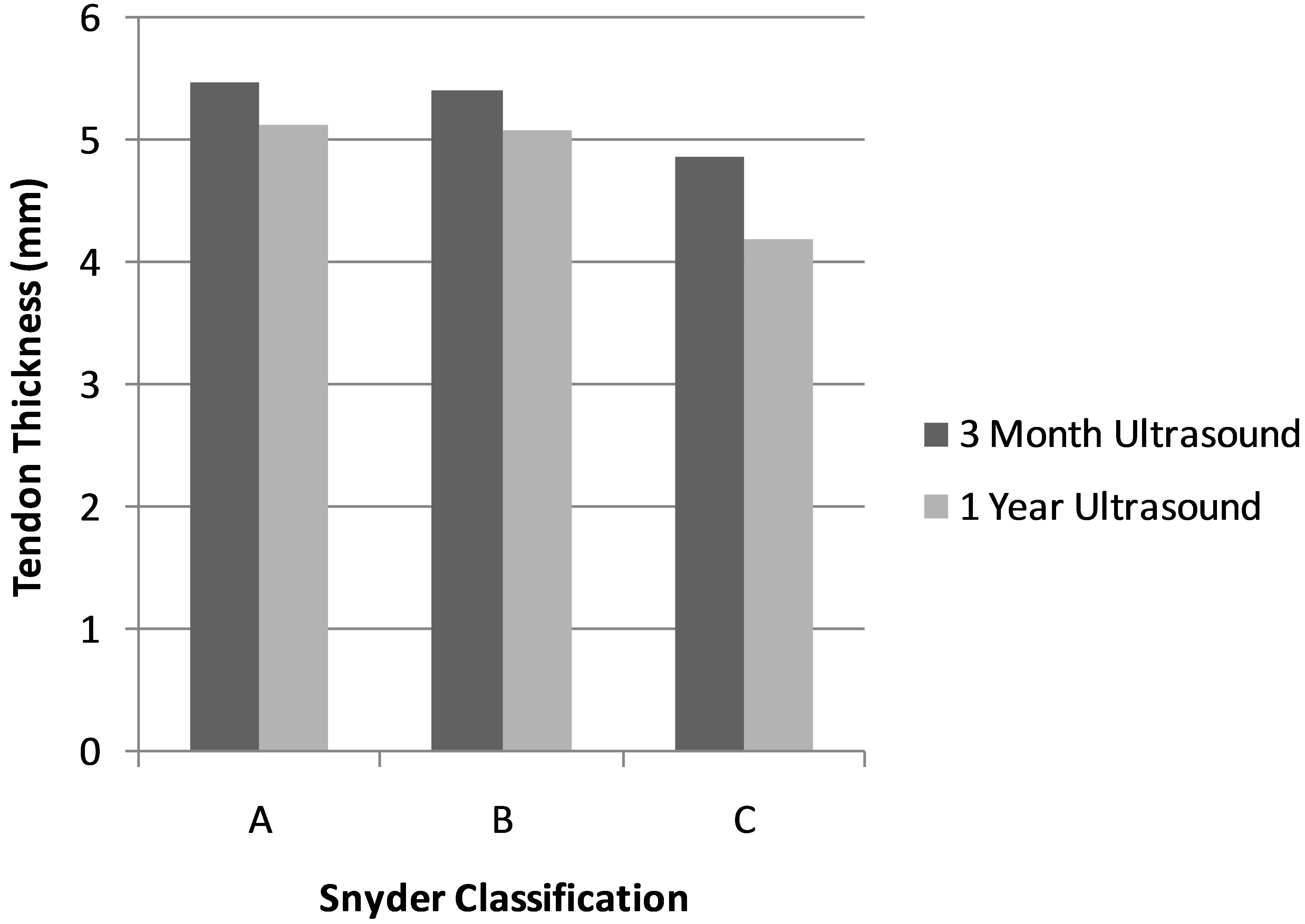
Figure 6. Tendon thickness at different post-operative timepoints separated by Snyder class.
4. DISCUSSION
Interest in ultrasound for the preand post-operative evaluation of rotator cuff tendon tears has increased in recent years [14,15]. While the appearance of post-operative rotator cuff re-tears has been known in the literature for many years [6], assessments in the post-operative setting have generally focused on whether an intact tendon is present. More recent investigations have examined post-operative cuff vascularity [16]; however, descriptions of normal post-operative tendon thickness are lacking. The present study examines for the first time sonographically changes in the post-operative thickness
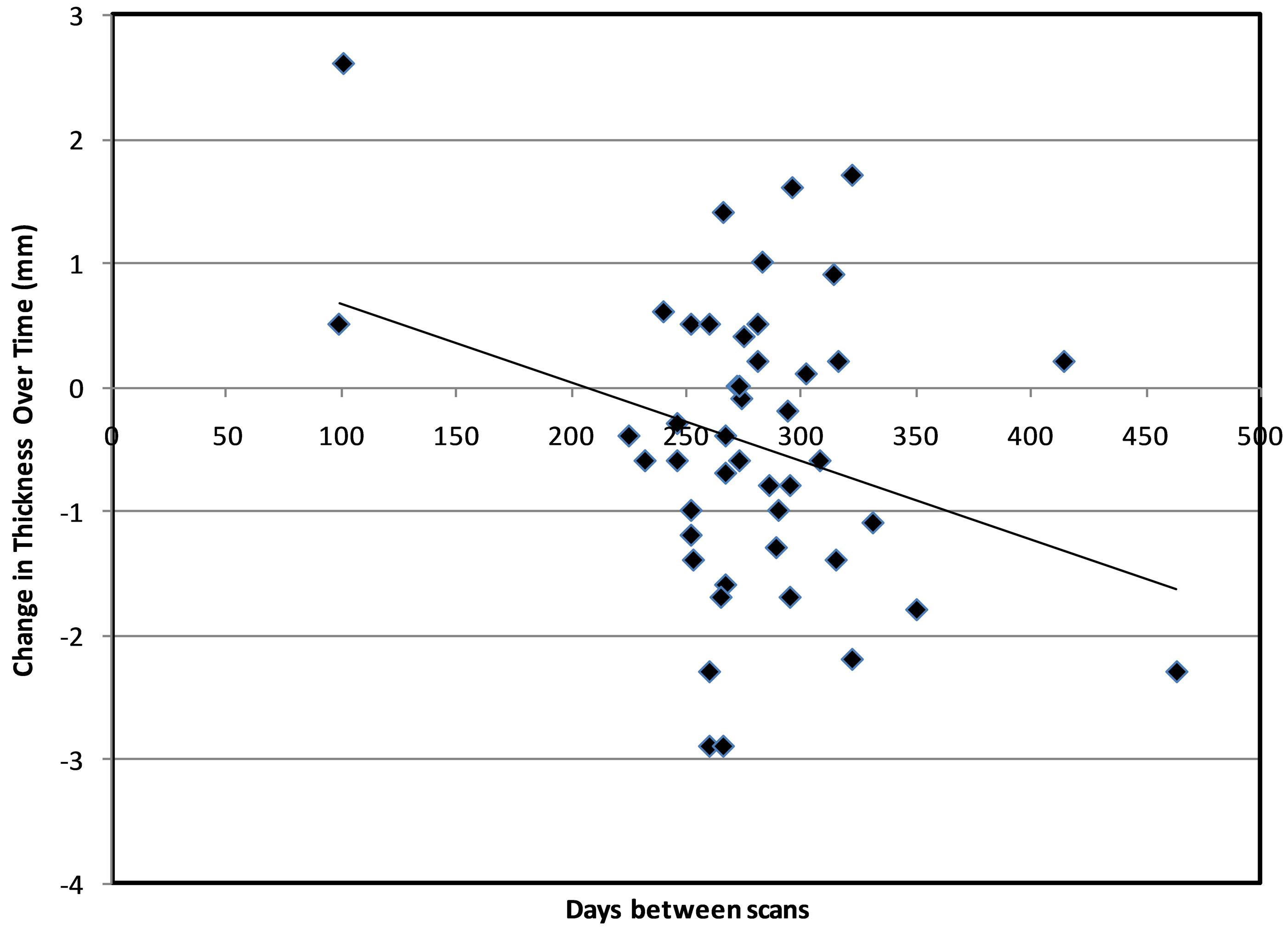
Figure 7. Change in tendon thickness (mm) over time. A statistically significant negative trend was observed (p < 0.05).
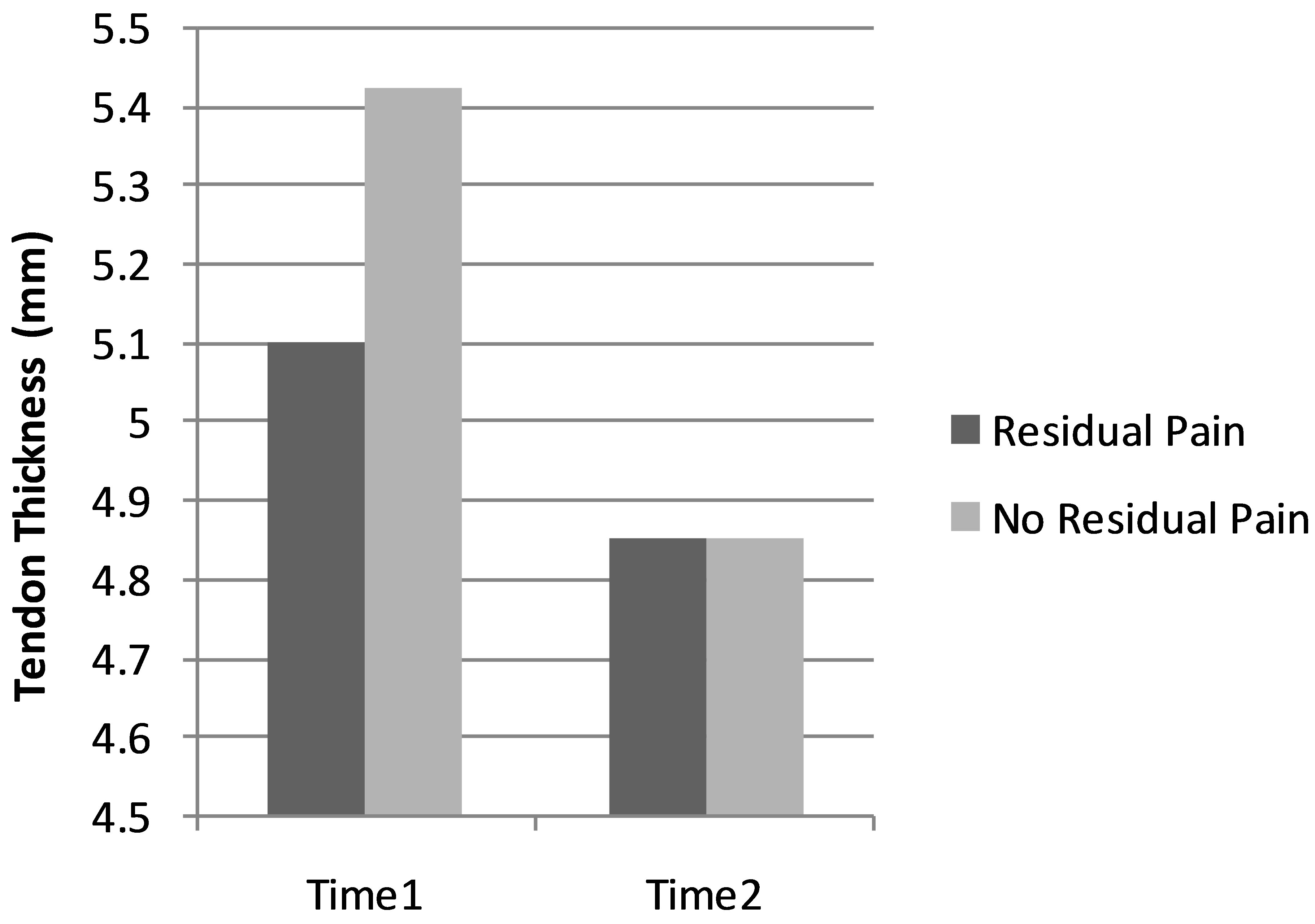
Figure 8. Graph demonstrating the residual post-operative pain does not correspond to tendon thickness as measured on ultrasound (p > 0.05).
of the supraspinatus tendon over time, reporting several novel findings.
First, post-operative tendon thickness with Snyder type C tears appears to be less than for other types of tears. This finding has not been previously reported in the literature and may relate to difficulties repairing completely ruptured tendons (Synder C) versus less severe injuries. While type C tears exhibited overall worse preoperative deficits, post-operatively there was no statistically significantly differences in pain, deficits, or force between the tear types. Differences in tendon thickness were not found to correlate with any of the aforementioned clinical outcome measures. Although, a similar study assessing the post-operative MR appearance of rotator cuff reported similar findings with respect to tendon thickness [10], the hypothesis of this work was that greater spatial resolution and the real-time evaluation offered with sonography would yield different results.
That work also found the tendon footprint size and tendon signal intensity to be unrelated to clinical outcome. The present study characterizes changes in postoperative supraspinatus tendon thickness over time, finding a tendency for decreased thickness later in the postoperative course. In the ANOVA analysis, there were no statistically significant differences in tendon thickness between the two serial ultrasounds, when accounting for the timeframe lapsed between the studies, a statistically significant trend toward decreased thickness over time was observed. The previous report on serial changes in post-operative tendon thickness utilizing MR demonstrated variable results [10].
Differences in supraspinatus tendon thickness have been previously observed on the basis of patient age [17] and systemic disease [18,19]; although, these were not studies examining the post-operative rotator cuff. The presence of conditions such as diabetes and amyloidosis, which have been associated with tendon thickening, was not formally assessed in this study. A study by Yu et al. reported tendon thickness measured on ultrasound in asymptomatic patients to increase with patient age [17]. In the present work, no correlation was observed between age and tendon thickness as measured on 3-month ultrasound follow-up. However, subsequent measurements revealed a negative correlation between patient age and tendon thickness. The mechanism behind this is unclear, but may relate diminished vascularity and/or healing in older patients. There was also a non-statistically significant trend towards decreased tendon thickness thickness from the 3rd to 12th post-operative month, which may relate to decreasing tendon inflammation and/ or edema later in the post-operative course.
The published rate of post-operative rotator cuff retears varies widely. In the present study, post-operative re-tears were present only in 2 of 53 cases (3.8%), a rate on the low-end of that reported in the literature [10]. The number of tears observed was too small in this study to draw any definite conclusions. In the two observed retear cases, the first occurred prior to the initial sonographic evaluation and the second after the final sonogram. The tendon thicknesses measured in the latter case were approximately 4 mm, which is well-within the range of observed normal post-operative values reported herein. It remains unclear whether a thin post-operative tendon predisposes to re-tear.
Sonographic evaluation of the repaired rotator cuff at or near the third post-operative month is important as the clinical examination at this time period may be limited secondary to immobility and pain. Moreover, the majority of recurrent rotator cuff tears occur within the first 3 months of surgical repair [20]. This is also the time during which the patient’s in our practice typically begin undergoing more intense physical therapy utilizing resistance training. Early detection of such tears may obviate extensive rehabilitation being pursued on patients with re-tears who will require surgery anyway. As a cautionary measure, our clinical approach to patients with sonographic supraspinatus thickness less than 4 mm postoperatively has been cautious with careful progression in physical activity and activities of daily living. While we have found this approach to be useful in our practice, further evaluation of its efficacy is warranted.
The limitations of this study include its retrospective nature and the relatively small number of patients included. Other morphological tendon characteristics, such as echogenicity, were not directly assessed. Ideally, further study would be undertaken to identify sonographic features of the supraspinatus tendon predicting re-tear. With respect to this, however, the small number of retears present in this study remains a limitation.
In conclusion, the thickness of the repaired supraspinatus tendon decreases over time post-operatively. Overall, diminished tendon thickness as assessed by ultrasound is associated with Synder category C rotator cuff tears and patient age. Post-operative tendon thickness does not appear to predict clinical outcome.
REFERENCES
- Miller, B.S., Downie, B.K., Kohen, R.B., et al. (2011) When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. The American Journal of Sports Medicine, 39, 2064-2070. doi:10.1177/0363546511413372
- Bishop, J., Klepps, S., Lo, I.K., et al. (2006) Cuff integrity after arthroscopic versus open rotator cuff repair: A prospective study. Journal of Shoulder and Elbow Surgery, 15, 290-299. doi:10.1016/j.jse.2005.09.017
- Galatz, L.M., Ball, C.M., Teefey, S.A., et al. (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. The Journal of Bone & Joint Surgery, 86-A, 219-224.
- Zlatkin, M.B. (2002) MRI of the postoperative shoulder. Skeletal Radiology, 31, 63-80. doi:10.1007/s00256-001-0460-1
- Sipola, P., Niemitukia, L., Kroger, H., et al. (2010) Detection and quantification of rotator cuff tears with ultrasonography and magnetic resonance imaging—A prospective study in 77 consecutive patients with a surgical reference. Ultrasound in Medicine and Biology, 36, 1981- 1989. doi:10.1016/j.ultrasmedbio.2010.09.001
- Crass, J.R., Craig, E.V. and Feinberg, S.B. (1986) Sonography of the postoperative rotator cuff. American Journal of Roentgenology, 146, 561-564. doi:10.2214/ajr.146.3.561
- Klepps, S., Bishop, J., Lin, J., et al. (2004) Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. The American Journal of Sports Medicine, 32, 1716-1722. doi:10.1177/0363546504265262
- Oh, J.H., Kim, S.H., Ji, H.M., et al. (2009) Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy, 25, 30-39. doi:10.1016/j.arthro.2008.08.010
- Liu, S.H. and Baker, C.L. (1994) Arthroscopically assisted rotator cuff repair: Correlation of functional results with integrity of the cuff. Arthroscopy, 10, 54-60. doi:10.1016/S0749-8063(05)80293-2
- Crim, J., Burks, R., Manaster, B.J., et al. (2010) Temporal evolution of MRI findings after arthroscopic rotator cuff repair. AJR American Journal of Roentgenology, 195, 1361-1366. doi:10.2214/AJR.10.4436
- Snyder, S. (2003) Arthroscopic classification of rotator cuff lesions and surgical decision making. Shoulder arthroscopy. Lippincott Williams, and Wilkins, Philadelphia, 201-207.
- Burkhart, S.S. and Lo, I.K. (2006) Arthroscopic rotator cuff repair. Journal of the American Academy of Orthopaedic Surgeons, 14, 333-346.
- Constant, C.R. and Murley, A.H. (1987) A clinical method of functional assessment of the shoulder. Clinical Orthopaedics and Related Research, 214, 160-164.
- Seagger, R., Bunker, T. and Hamer, P. (2011) Surgeonoperated ultrasonography in a one-stop shoulder clinic. Annals of the Royal College of Surgeons of England, 93, 528-531. doi:10.1308/147870811X13137608454939
- Gamradt, S.C., Gallo, R.A., Adler, R.S., et al. (2010) Vascularity of the supraspinatus tendon three months after repair: Characterization using contrast-enhanced ultrasound. Journal of Shoulder and Elbow Surgery, 19, 73-80. doi:10.1016/j.jse.2009.04.004
- Cadet, E.R., Adler, R.S., Gallo, R.A., et al. (2012) Contrast-enhanced ultrasound characterization of the vascularity of the repaired rotator cuff tendon: Short-term and intermediate-term follow-up. Journal of Shoulder and Elbow Surgery, 21, 597-603. doi:10.1016/j.jse.2011.04.001
- Yu, T.Y., Tsai, W.C., Cheng, J.W., et al. (2012) The effects of aging on quantitative sonographic features of rotator cuff tendons. Journal of Clinical Ultrasound, 40, 471-478. doi:10.1002/jcu.21919
- Jadoul, M., Malghem, J., Vande Berg, B., et al. (1993) Ultrasonographic detection of thickened joint capsules and tendons as marker of dialysis-related amyloidosis: A cross-sectional and longitudinal study. Nephrology Dialysis Transplantation, 8, 1104-1109.
- Akturk, M., Karaahmetoglu, S., Kacar, M., et al. (2002) Thickness of the supraspinatus and biceps tendons in diabetic patients. Diabetes Care, 25, 408. doi:10.2337/diacare.25.2.408
- Kluger, R., Bock, P., Mittlbock, M., et al. (2011) Longterm survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. The American Journal of Sports Medicine, 39, 2071-2081. doi:10.1177/0363546511406395
NOTES
*Corresponding author.

