Open Journal of Obstetrics and Gynecology
Vol.3 No.4A(2013), Article ID:33030,9 pages DOI:10.4236/ojog.2013.34A002
Professional’s skills in assessment of perineal tears after childbirth—A systematic review
![]()
1Centre for Person-Centred Care, Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
2Department of Obstetrics and Gynecology, Østfold Hospital Trust, Fredrikstad, Norway
3Department of Obstetrics and Gynecology, Perinatal Center, Sahlgrenska University Hospital, Gothenburg, Sweden
Email: ann.morris@so-hf.no
Copyright © 2013 Ann Morris et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 28 March 2013; revised 27 April 2013; accepted 5 May 2013
Keywords: Perineum Injuries; Perineal Tears; Obstetrics/Midwifery Education; Clinical Competence; Review; Childbirth
ABSTRACT
Perineal tears are one of the most common complications of vaginal births and may cause discomfort and pain long time after childbirth. Visual and digital examination of perineal tears is the most common way to assess and classify a perineal tear. Recent research indicates that many tears diagnosed are misclassified. The aim of this systematic literature review was to outline research that investigates healthcare professionals’ clinical knowledge in assessment and classification of perineal tears in connection with childbirth. Searches were performed in PubMed and CINAHL. Six studies on the topic were identified and used to collect data for questionnaires. An integrative review was used in the analysis. Poor knowledge in perineal anatomy and lack of training in clinical assessment and classification of perineal trauma was evident among both physicians and midwives. These findings indicate that healthcare providers lack adequate knowledge and that they make incorrect assessments and errors in classification of perineal tears. The training in assessment and classification is crucial. Midwives are in a unique position to improve the standard of care in this field since they are often the first and many times the only to assess the injury.
1. INTRODUCTION
Perineal tears are the most common complications of vaginal births. The true incidence of perineal tears is not known for several reasons, for instance incomplete assessment by clinicians [1,2], confusion about definitions [3] and variation in practices and reporting on minor perineal tears [4,5]. Two British studies [4,6] describing the incidence of all tears found that approximately 85% of the women had some form of tear after birth. Not all of them required suturing [4].
Pain in the perineum is common after vaginal birth whether the woman had a tear or not [7,8]. Women can experience pain and discomfort related to perineal tears for weeks and even months after delivery [9,10]. Persisting perineal pain can inhibit the woman from being fully mobile and sitting comfortably. This might influence the women’s ability to bond to and breastfeed the baby [11]. Dyspareunia after childbirth is common and seems related to the severity of the trauma sustained [12,13]. The connection between perineal third or fourth degree tears and anal incontinence after childbirth is well documented. Although significant incontinence only affects a minority of women, its symptoms may have devastating effects on the quality of life for the women affected [14]. A dilemma with health problems related to perineal tears is that women do not necessarily address the problem at postnatal controls. Problems such as perineal pain, sexual dysfunction and incontinence are often only disclosed when specifically asked for [9].
The midwives assess, classify and suture most tears classified as perineal first or second degree tears [4,15] and episiotomies. A physician is required if there is a suspicion that the tear involves the anal sphincter muscles, perineal tear grade three or four, or an otherwise complicated tear, for example a tear that bleeds so much that it makes suturing difficult [15]. Visual and digital examination of the wound is the most common way to assess and classify a perineal tear [16]. However several studies indicate that many tears diagnosed with this method are misclassified [1,2,17,18]. After the introduction of anal ultrasound as a diagnostic method it was discovered that a large proportion of women without clinically detected sphincter tears had defects to the anal sphincter on ultrasound scan [17].
There is no congruence in what can be considered the golden standard when diagnosing perineal tears [19]. Women with second degree tears are the group most likely to develop anal incontinence postpartum, suggesting the possibility that a proportion of anal sphincter tears remain undetected at delivery [20]. The suggested reason for the extent of the clinically undetected sphincter tears is, apart from the fact that bleeding and tissue oedema make the diagnoses difficult, that many healthcare providers have too little training in perineal assessment and basic anatomy [2,21].
The aim of this systematic literature review was to outline research that investigates healthcare professionals’ clinical knowledge in the assessment and classification of perineal tears in connection with childbirth.
2. METHODS
The literature searches were performed between May 2012 and Mars 2013 in the electronic databases PubMed and CINAHL. Articles between 1983 and 2012 were viewed. The search terms were: perineum; perineum/ injuries; perineal tears; perineal laceration; perineal rupture; perineal trauma; “perineal second degree tears”; perineal first degree tear; perineal third degree tear; episiotomy, anal canal injuries; obstetric perineal tears; assessment; audit; “professional knowledge”; obstetrics education; midwifery education; gynaecology education; obstetric standards; midwifery standards; obstetric skill; midwifery skill; obstetric labour complications/diagnosis; classification; evaluation. Combinations of these key words were also used. English language was used as a limitation when searching for articles. At the start the search also included studies in Swedish, Danish and Norwegian but later English was used as language limitation as no studies of interest were found in these languages.
The total search resulted in 1154 articles. Included studies should intend to investigate healthcare professionals’ knowledge in assessment by digital and visual examination of perineal tears after childbirth. Excluded were studies which only indirectly examined the clinical competence in assessment and classification of perineal tears, for example studies aiming to find different methods to assess perineal tears or studies trying to find the true incidence of occult perineal tears grade III and IV. Two of the authors (AM, AD) independently reviewed all citations by 1) title, 2) abstract and 3) full text. The majority could be excluded just by the title or after reading the abstract. The references of all included articles were also reviewed and one article was found this way [22], see Figure 1. Several articles read in full text were ex-
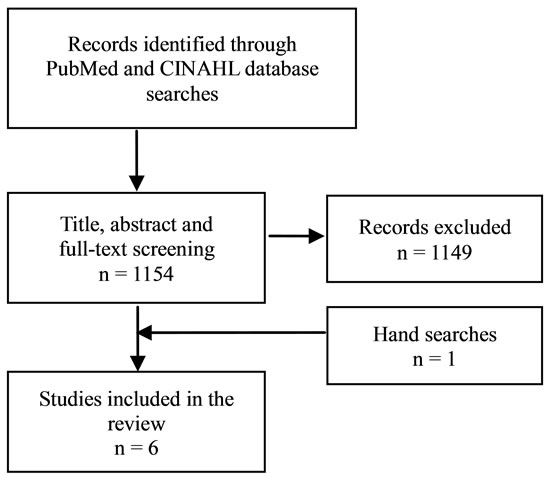
Figure 1. Flow diagram of screening process.
cluded because they did not meet the inclusion criteria. For example a study of McLennan et al. [23] was excluded because it did not investigate the current knowledge or perception of knowledge but whether residents had received formal training or didactics in episiotomy or perineal repair.
An integrative review focuses on results of research and integrates the findings from individual studies. It attempts to integrate and draw conclusions from studies using different methods enabling an overall conclusion to be made and the findings to be generalised to other populations with broader confidence [24]. Evaluation of included studies was guided by a literature review protocol by Polit and Beck [25, pp. 112-114].
3. FINDINGS
Six studies on the topic of healthcare professionals’ knowledge in assessing and classifying perineal tears (Table 1) were identified [22,26-30], see description of included studies in Table 2. In all studies data were collected through questionnaires. In one study the questionnaire was filled out in the course of an interview to make sure the questions were correctly understood [30]. All studies also assessed other aspects of perineal management, for example knowledge in repair, which are not presented here since the focus of this review is assessment and classification. Studies that address the issue of knowledge in perineal anatomy were also included in the result. Five of the studies were from the UK and one was carried out in Spain.
The presentation of included studies was divided into three parts; 1) a quality assessment of included studies (see Table 3), 2) a short summary of the studies’ results presented in three categories; anatomy, classification, perception on knowledge and training in perineal assessment and finally 3) a synthesis of the results.
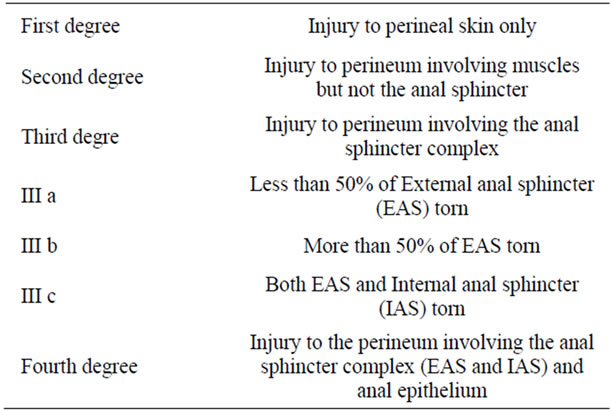
Table 1. Classification of perineal injury grade 1 - 4.
3.1. Anatomy
Two studies investigated the midwives’ and doctors’ knowledge in pelvic anatomy. Both studies indicate poor knowledge in perineal anatomy.
Cornet et al. [27] investigated residents’ own perception of knowledge in perineal anatomy. A majority (62%) of the residents thought their knowledge in pelvic floor anatomy was inadequate. Sultan et al. [30] asked both doctors and midwives if they knew the muscles cut during an uncomplicated episiotomy. Of participants 69% of doctors and 25% of the midwives stated they knew which muscles were cut but over half of the ones stating they knew the muscles named them incorrectly.
3.2. Classification
Four studies analysed how well perineal tears were classified. All these studies indicate that many midwives and/or doctors classified perineal tears incorrectly.
The study of Mutema [28] was the only study that investigated classification of first degree tears as well as all the other tears. It established that more than a third of the midwives in two different hospitals did not know the correct classification of a perineal tear grade one. The situation was better for second degree tears but varied more between the two hospitals. In one hospital 30% of the midwives did not know the correct classification of a second degree tear while in the other hospital only 6% classified perineal tears grade two incorrectly. The percentages of correct answers decreased with the more severe tears and less than half of the midwives knew the correct classification of a perineal third degree tear. More than two thirds did not know the correct classification of a perineal tear grade four.
Andrews et al. [22] investigated whether a one day hands-on workshop in repair of episiotomy and second degree tears changed the clinical practice by improving participants’ ability to accurately classify obstetric anal sphincter injuries (OASI) and manage perineal trauma according to best practice. Due to a small number of participating doctors, midwives and doctors were analysed together. Most of the participants had performed more than 30 second degree perineal tear repairs before entering the course. Before the course the correct answers to questions on classification varied from 45% to 80% and after the course the proportion of correct answers ranged from 67% to 89%.
Fernando et al. [29] performed a systematic review of the literature and a survey of current practice among obstetricians and members of the Association of Coloproctologists in the UK. About 11% of consultants and 9% of trainees did classify second degree tears as “not defined”. Three per cent of consultants and 5% of the trainees classified them as third degree perineal tears. A further 33% of the consultants classified a third degree tear as a second degree tear as did 22% of the trainees. There was a regional difference in the misclassification. The literature review revealed a lack of consistency in the classification of perineal tears when 65 obstetric texts in the Royal College of Obstetrics and Gynaecology (ROCG) library were analysed.
Sultan et al. [30] found that when midwives and doctors were asked to classify perineal tears 92% of the doctors and 99% of the midwives described first, second and third degree perineal tears. The remainder also mentioned fourth degree perineal tears. On questions about how midwives described injuries to different anatomic structures the percentage of correct classification varied from 61% to 84%. A further 15% of midwives thought all extended episiotomies and torn urethras were third degree perineal tears. The percentage of correct answers in classification among doctors ranged from 44% to 93%. None of the doctors thought all extended episiotomies were third degree perineal tears but 8% thought a torn urethra was considered to be a third degree perineal tear.
3.3. Perceptions on Knowledge and Training in Perineal Assessment and Classification
All six studies in this review addressed the matter of doctors and/or midwives own perception of training and current knowledge in anatomy and classification of perineal tears. All included studies showed that a majority of midwives and doctors recognise that their knowledge and training in perineal assessment and classification is poor.
A survey of Bick et al. [26] addressed the issue on how well midwives in the UK implement evidence based guidelines in their practice. The midwives were asked how confident they felt in assessing perineal trauma. Around a third of the midwives (34.3%) felt confident in assessing perineal trauma “all” the time; 55% were confident “most” of the time and 10.7% felt confident “some of the time”. No midwives reported that they “never” felt confident. There was a significant positive correlation
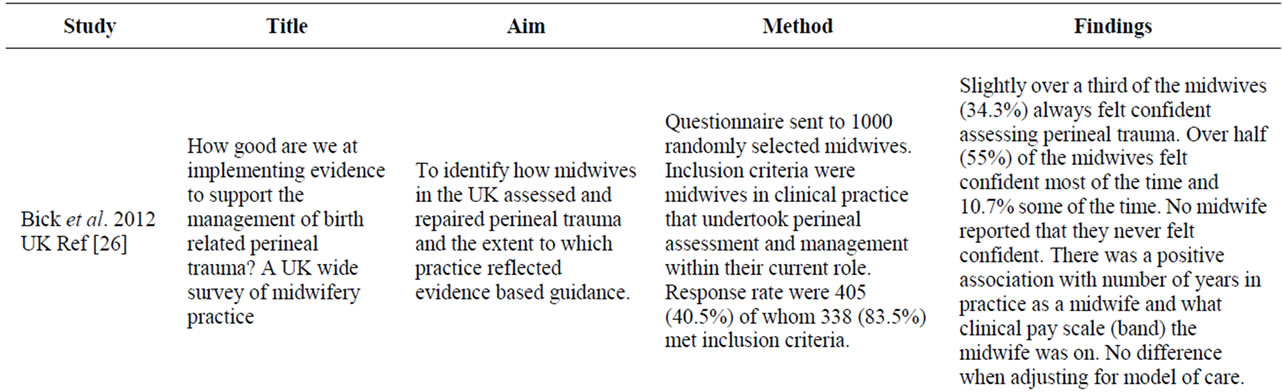
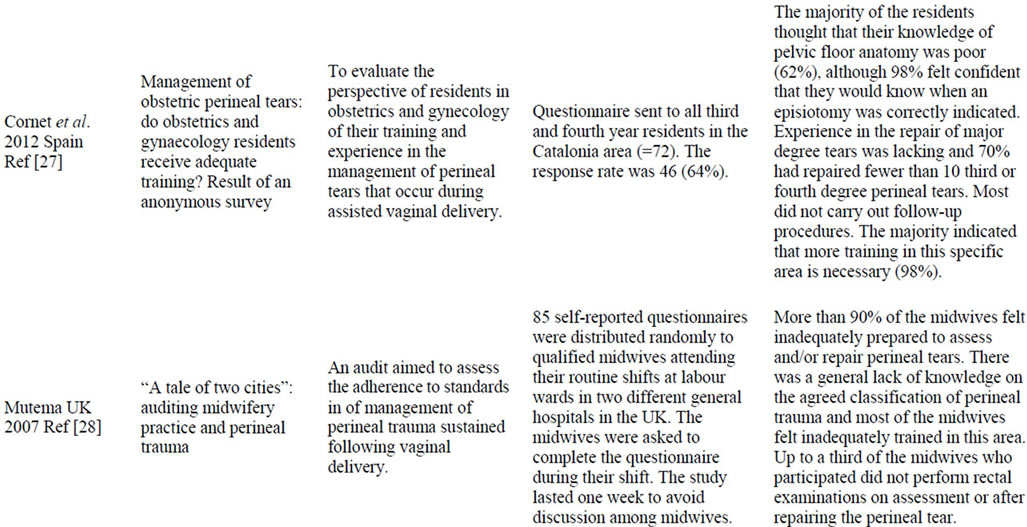
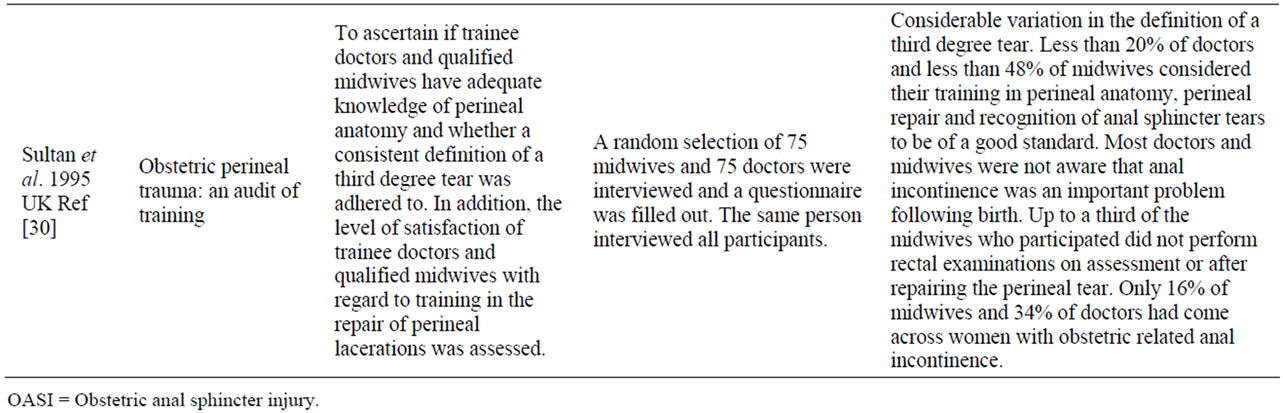
Table 2. Description of included studies.
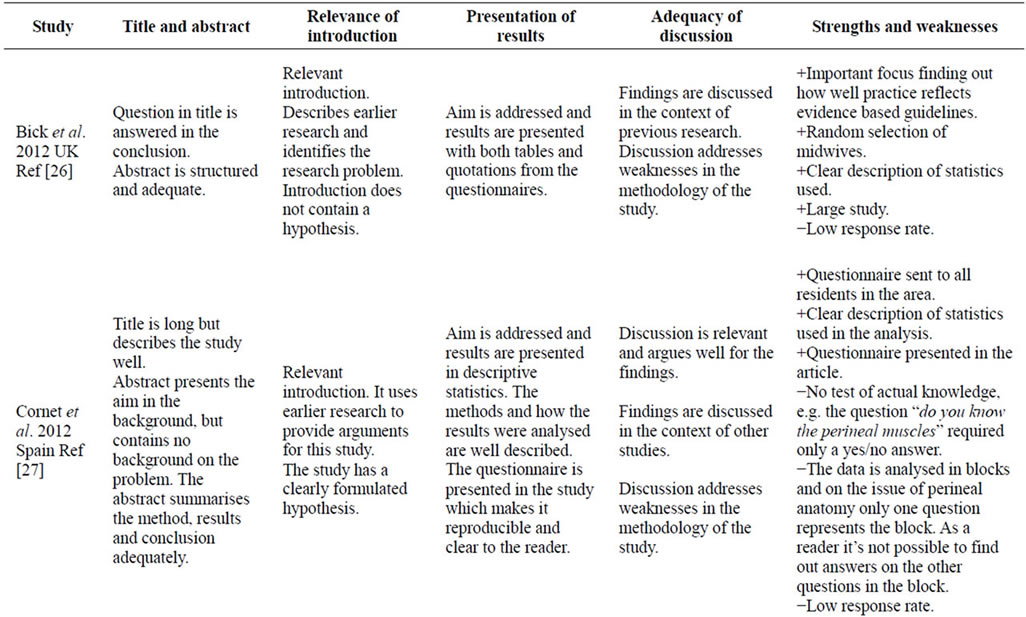
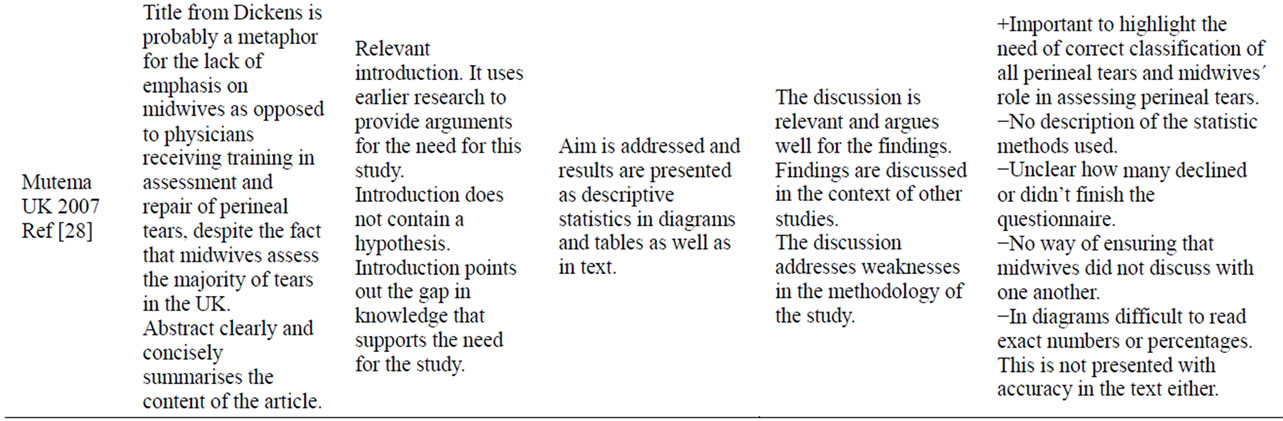
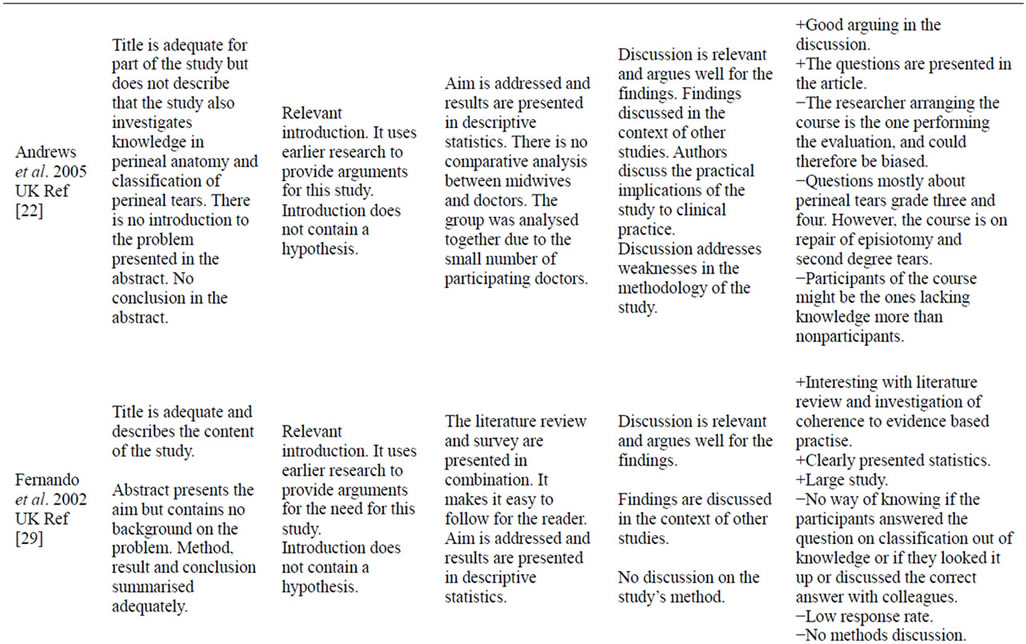
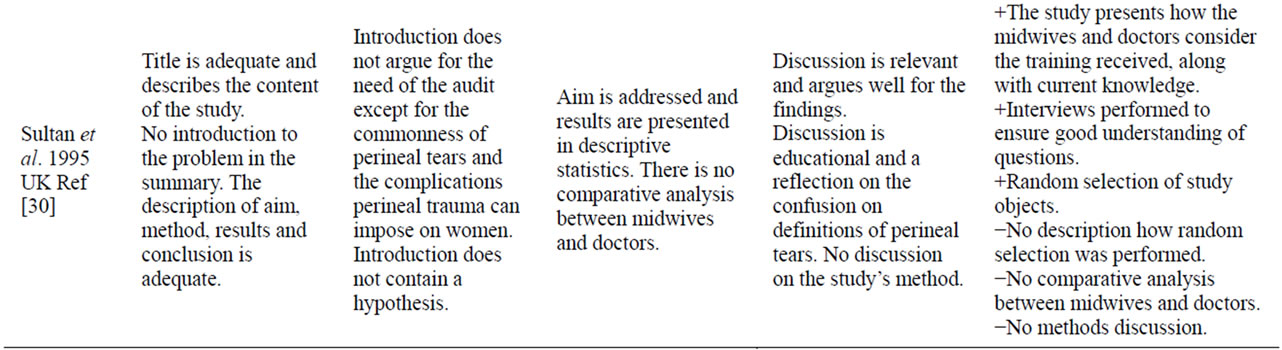
Table 3. Quality judgment of included studies.
between the number of years as a qualified midwife and higher band (more senior clinical post) and confidence in assessing perineal trauma. There was no correlation between level of confidence and model of maternity care or location of care. When midwives were asked whether they always performed rectal examination as routine when assessing perineal trauma less than half of the midwives (42.4%) did this “all” the time, 13.1% “most” of the time, 27.2% “some” of the time and 17.3% “never” performed a rectal examination when assessing perineal trauma. Higher band was associated with a higher number of midwives performing rectal examination “all” the time. There was no association between years as qualified midwife, model of care or location of practice and rectal examinations.
The Spanish study by Cornet et al. [27] found that 91% of the residents thought it was necessary to receive more theoretical training and 98% thought there was a need for a theoretical-practical course on pelvic floor anatomy and on the repair of perineal injuries. Mutema [28] found that 90% of the midwives in the study felt inadequately prepared to assess or repair perineal tears in both units. All of the midwives would have liked to attend a course in assessment and repair of perineal tears if the trusts facilitated it. Andrews et al. [22] found that 24% of the midwives and doctors thought their training was poor when performing their first unsupervised perineal repair; another 40% thought it could have been better. Fernando et al. [29] did not find any research in the literature review on studies comparing different methods of training. The survey disclosed that 64% of consultants and trainees reported either lack of or unsatisfactory training in the management of perineal tears grade three or four. Finally, Sultan et al. [30] revealed that only 39% of the midwives and 16% of doctors thought their training in recognising a third degree perineal tear was of good quality when performing their first unsupervised perineal repair.
3.4. Synthesis of the Research Findings
These findings point out a lack of knowledge in perineal anatomy among both doctors and midwives. This deficiency in anatomic understanding leads to impaired assessment of perineal tears grade 1 - 4 following vaginal birth. This adversely affects the ability to classify correctly and a large proportion of both doctors and midwives make errors in the classification of the injuries. Both professions perceive they have inadequate knowledge in the topic of perineal assessment after childbirth, experience that they lack training in the assessment of perineal injuries and consider their clinical training under the supervision of experienced tutors to be insufficient. This insecurity among professionals highlights a need for a more in-depth theoretical knowledge as well as improved clinical training for both professions. There is also a strong focus in the literature on the less frequent perineal tears, grade three and four, and little scientific or health care focus on the most common perineal injuries grade one and two that a majority of postnatal women suffer from after childbirth.
4. DISCUSSION
Considered individually, all of the studies included in this review have methodological flaws (Table 3). When considered together, the flaws do not outweigh the evidence produced to support the need for better training in perineal anatomy, and assessment and classification of perineal tears. None of the studies were of very high quality due to different methodological problems, lack of validated questionnaires, no control of whether the responders discussed or looked for the correct answer and small study populations. The fact that the healthcare professionals themselves perceive that their knowledge and training is inadequate is enough to conclude that training needs to be better. Studies with the aim of finding out the true prevalence of occult third and fourth degree tears strengthen the validity of the findings in this review. In these studies an expert re-examined the perineal tears that had been assessed and classified by the midwife or doctor that assisted the birth and found that a large part of the so called occult third and fourth degree tears were in fact overt [1,2].
It is a concern that midwives and doctors do not know the correct names of the muscles involved when performing an episiotomy, the most common surgical procedure in obstetrics [30]. It can be argued that it is less important that healthcare professionals know the correct names as long as they assess and suture the perineal tears correctly. On the contrary it can also be argued that it is essential to have a precise language that enables professionals to communicate knowledge, perform research and develop skills. In order to evaluate the effectiveness of different methods and to improve the standard of knowledge it is important to establish good procedures in how the evaluation process can be validated.
Many questions remain unanswered because of weak descriptions in the methods. In most studies it was not possible to control whether healthcare professionals communicated or searched for correct answers before filling out the study questionnaire [22,28,29]. A strong point is that in all studies the midwife or doctor was asked about their own perception of their training and knowledge in perineal assessment. Five studies were from the UK and one from Spain. This makes it difficult to evaluate the generalizability of the studies since education and practices vary between different countries [30].
It is important that more research on the topic of knowledge in assessment and classification of perineal tears is carried out. The Description of Essential Competencies for Midwives from the International Confederation of Midwives (ICM) [31] includes principles for prevention of pelvic floor damage and perineal tears, indications for performing an episiotomy, principles underpinning the technique for repair of perineal tears and episiotomy, skills to perform an episiotomy when needed and to repair first and second degree perineal or vaginal lacerations as well as an episiotomy if needed. These skills are listed as basic and essential for midwives. However, knowledge of perineal anatomy, rectal palpation and ability to classify perineal tears are not mentioned [31]. McLennan et al. [23] revealed that a majority of fouryear residents received no formal training in pelvic floor anatomy or episiotomy repair and had insufficient supervision when engaged in such activities. Furthermore, Nielsen et al. [32] who performed a study on Objective Structured Assessment for Technical Skills for episiotomy repair found that 60% of residents who failed because of technical skill did so because they did not fully evaluate the injury either before or after repair.
An alarming finding in this review is that a majority of midwives and doctors felt inadequately trained in perineal anatomy and assessment of perineal trauma. This shows the importance of conducting research on the best methods for training in assessment of perineal tears. There is also a need for research on assessment and classification of perineal tears grade one and two, which are the most common tears [4] and to determine the golden standard for assessing perineal tears. It would improve the credibility if a validated questionnaire was created to be used as a measuring tool before and after interventions so that studies can be reproduced in different countries. In Norway a randomised controlled trial is currently being carried out with the aim to investigate consistency between midwives’ classification and estimation of the size of the perineal tear, with and without a tool to assist the assessment of the tear (Clintrials.gov ID. NCT01278979).
Methodological Considerations
Searches in databases is a common and efficient way to find publications, but there are recognised limitations associated with inconsistent search terminology and indexing problems which may yield only about 50% of the eligible studies [24,33]. The searches on knowledge in assessment and classification of perineal tears proved to have an inconsistent search terminology which made the database searches alone an unreliable source to use for finding articles on the topic requiring that a large number of titles and abstracts had to be read through. Therefore, reference lists in relevant studies found were scrutinised and the search was extended with new search terms. One problem with the topic of perineal tears is that many studies in obstetrics have perineal tears as a secondary outcome measure, but the primary outcome may be on birth positions, augmentation or instrumental deliveries. It proved to be hard to keep these studies out despite using combinations of search terms aimed at narrowing the search to the specific topic of knowledge in assessment and classification of perineal tears. Another problem that occurred was that almost all research done on the topic assessment/diagnosing and classifying of perineal tears focuses only on perineal tears grade three and four. Even though congruence of the incidence of these tears remains uncertain they represent a small proportion of all tears diagnosed clinically [18]. On the topic of the current knowledge among healthcare professionals when assessing perineal tears it was not possible to find randomised controlled trials.
To evaluate the quality of the studies a guide of overall critique from Polit and Beck was being used [25]. Peer-reviewed studies were not used as a limitation for the search in CINAHL because by including all studies, even those of poor quality, it is possible to map out what is good and bad with earlier research [33]. Quality scoring in observational studies is as controversial as it is in randomised controlled trials and may lack demonstrated validity and therefore affect the validity of the results [24]. In this review the quality of the studies is discussed but there is no attempt to follow a quality scoring. Due to the non-experimental design in the studies found on the topic of assessment of perineal tears this review is presented as an integrative review.
5. CONCLUSIONS
The findings in this review provide evidence that healthcare providers lack adequate training in assessment and classification of perineal tears and in perineal anatomy. The training of healthcare professionals in assessment and correct classification of perineal tears is urgent. Midwives are often the first, and many times the only, to assess and classify perineal tears. Therefore, they are in a unique position to improve the standard of care in this field.
The consequences for the women who suffer from incorrectly assessed and classified tears, and as a result receive wrong treatment, may be both personal suffering and increased health care costs due to need of re-suturing or incontinence treatment. There are also legal aspects where incorrect treatment may lead to litigation issues.
REFERENCES
- Andrews, V., Sultan, A.H., Thakar, R. and Jones, P.W. (2006) Occult anal sphincter injuries—Myth or reality? BJOG: An International Journal of Obstetrics & Gynaecology, 113, 195-200. doi:10.1111/j.1471-0528.2006.00799.x
- Groom, K.M. and Paterson-Brown, S. (2002) Can we improve on the diagnosis of third degree tears? European Journal of Obstetrics & Gynecology and Reproductive Biology, 10, 19-21. doi:10.1016/S0301-2115(01)00495-X
- Hordnes, K. and Bergsjo, P. (1993) Severe lacerations after childbirth. Acta Obstetricia et Gynecologica Scandinavica, 72, 413-422. doi:10.3109/00016349309021127
- Albers, L., Garcia, J., Renfrew, M., McCandlish, R. and Elbourne, D. (1999) Distribution of genital tract trauma in childbirth and related postnatal pain. Birth, 26, 11-17. doi:10.1046/j.1523-536x.1999.00011.x
- Renfrew, M.J., Hannah, W., Albers, L. and Floyd, E. (1998) Practices that minimize trauma to the genital tract in childbirth: A systematic review of the literature. Birth, 25, 143-160. doi:10.1111/j.1523-536X.1998.t01-2-.x
- Williams, F.L., du V Florey, C., Mires, G.J. and Ogston, S.A. (1998) Episiotomy and perineal tears in low-risk UK primigravidae. Journal of Public Health, 20, 422-427. doi:10.1093/oxfordjournals.pubmed.a024797
- Macarthur, A.J. and Macarthur, C. (2004) Incidence, severity, and determinants of perineal pain after vaginal delivery: A prospective cohort study. American Journal of Obstetrics & Gynecology, 191, 1199-1204. doi:10.1016/j.ajog.2004.02.064
- Andrews, V., Thakar, R., Sultan, A.H. and Jones, P.W. (2008) Evaluation of postpartum perineal pain and dyspareunia—A prospective study. European Journal of Obstetrics & Gynecology and Reproductive Biology, 137, 152-156. doi:10.1016/j.ejogrb.2007.06.005
- Brown, S. and Lumley, J. (1998) Maternal health after childbirth: Results of an Australian population based survey. BJOG: An International Journal of Obstetrics & Gynaecology, 105, 156-161. doi:10.1111/j.1471-0528.1998.tb10045.x
- Glazener, C.M., Abdalla, M., Stroud, P., Naji, S., Templeton, A. and Russell, I.T. (1995) Postnatal maternal morbidity: Extent, causes, prevention and treatment. BJOG: An International Journal of Obstetrics & Gynaecology, 102, 282-287. doi:10.1111/j.1471-0528.1995.tb09132.x
- Steen, M. (2005) “I can’t sit down”—Easing genital tract trauma. British Journal of Midwifery, 13, 311-314.
- Signorello, L.B., Harlow, B.L., Chekos, A.K. and Repke, J.T. (2001) Postpartum sexual functioning and its relationship to perineal trauma: A retrospective cohort study of primiparous women. American Journal of Obstetrics & Gynecology, 184, 881-890. doi:10.1067/mob.2001.113855
- Rådestad, I., Olsson, A., Nissen, E. and Rubertsson, C. (2008) Tears in the vagina, perineum, sphincter ani, and rectum and first sexual intercourse after childbirth: A nationwide follow-up. Birth, 35, 98-106. doi:10.1111/j.1523-536X.2008.00222.x
- Johanson, J.F. and Lafferty, J. (1996) Epidemiology of fecal incontinence: The silent affliction. The American Journal of Gastroenterology, 91, 33-36.
- Den norske legeforening, (2008) Norsk gynekologisk forening. Veileder i fødselshjelp. http://legeforeningen.no/Fagmed/Norsk-gynekologisk-forening/Veiledere/veileder-i-fodselshjelp-2008/kapittel-38-perinealruptur/
- Jaiyesimi, R.A.K. (2007) Pitfalls in the management of perineal trauma. Clinical Risk, 13, 89-91. doi:10.1258/135626207780559950
- Dudding, T.C., Vaizey, C.J. and Kamm, M.A. (2008) Obstetric anal sphincter injury: Incidence, risk factors, and management. Annals of Surgery, 247, 224-237. doi:10.1097/SLA.0b013e318142cdf4
- Sultan, A.H., Kamm, M.A., Hudson, C.N., Thomas, J.M. and Bartram, C.I. (1993) Anal-sphincter disruption during vaginal delivery. The New England Journal of Medicine, 329, 1905-1911. doi:10.1056/NEJM199312233292601
- Sultan, A.H. and Thakar, R. (2005) Diagnosis of anal sphincter tears to prevent fecal incontinence: A randomized controlled trial. Obstetrics & Gynecology, 106, 1108- 1109. doi:10.1097/01.AOG.0000186051.88740.7f
- Pretlove, S.J., Thompson, P.J., Guest, P., Toozs-Hobson, P. and Radley, S. (2003) Detecting anal sphincter injury: Acceptability and feasibility of endoanal ultrasound immediately postpartum. Ultrasound in Obstetrics & Gynecology, 22, 215-217. doi:10.1002/uog.136
- Andrews, V., Sultan, A.H., Thakar, R. and Jones, P.W. (2006) Risk factors for obstetric anal sphincter injury: A prospective study. Birth, 33, 117-122. doi:10.1111/j.0730-7659.2006.00088.x
- Andrews, V., Thakar, R., Sultan, A. and Kettle, C. (2005) Can hands-on perineal repair courses affect clinical practice? British Journal of Midwifery, 13, 562-565.
- McLennan, M.T., Melick, C.F., Clancy, S.L. and Artal, R. (2002) Episiotomy and perineal repair. An evaluation of resident education and experience. The Journal of Reproductive Medicine, 47, 1025-1030.
- Whittemore, R. and Knafl, K. (2005) The integrative review: Updated methodology. Journal of Advanced Nursing, 52, 546-553. doi:10.1111/j.1365-2648.2005.03621.x
- Polit, D.F. and Beck, C.T. (2012) Nursing research: Generating and assessing evidence for nursing practice. 9th Edition, Wolters Kluwer Health, Philadelphia.
- Bick, D.E., Ismail, K.M., MacDonald, S., Thomas, P., Tohill, S. and Kettle, C. (2012) How good are we at implementing evidence to support the management of birth related perineal trauma? A UK wide survey of midwifery practice. BMC Pregnancy and Childbirth, 12, 57. doi:10.1186/1471-2393-12-57
- Cornet, A., Porta, O., Pineiro, L., Ferriols, E., Gich, I. and Calaf, J. (2012) Management of obstetric perineal tears: Do obstetrics and gynaecology residents receive adequate training? Results of an anonymous survey. Obstetrics and Gynecology International, 2012.
- Mutema, E.K. (2007) “A tale of two cities”: Auditing midwifery practice and perineal trauma. British Journal of Midwifery, 15, 511-513.
- Fernando, R.J., Sultan, A.H., Radley, S., Jones, P.W. and Johanson, R.B. (2002) Management of obstetric anal sphincter injury: a systematic review & national practice survey. BMC Health Services Research, 2, 9. doi:10.1186/1472-6963-2-9
- Sultan, A.H., Kamm, M.A. and Hudson, C.N. (1995) Obstetric perineal trauma: An audit of training. Journal of Obstetrics & Gynaecology, 15, 19-23.
- International Confederation of Midwives, (2010) Essential competencies for basic midwifery practice. http://www.internationalmidwives.org/assets/uploads/documents/CoreDocuments/ICM%20Essential%20Competencies%20for%20Basic%20Midwifery%20Practice%202010,%20revised%202013.pdf
- Nielsen, P.E., Foglia, L.M., Mandel, L.S. and Chow, G.E. (2003) Objective structured assessment of technical skills for episiotomy repair. American Journal of Obstetrics & Gynecology, 189, 1257-1260. doi:10.1067/S0002-9378(03)00812-3
- Stroup, D.F., Berlin, J.A., Morton, S.C., Olkin, I., Williamson, G.D., Rennie, D., et al. (2000) Meta-analysis of observational studies in epidemiology: A proposal for reporting. The Journal of the American Medical Association, 283, 2008-2012. doi:10.1001/jama.283.15.2008

