Pain Studies and Treatment
Vol.04 No.01(2016), Article ID:62836,8 pages
10.4236/pst.2016.41002
Prolonged Opioid-Sparing Pain Control after Hemorrhoidectomy with Liposome Bupivacaine: Results from a Cohort of 95 Patients
Allen B. Jetmore1,2*, Douglas Hagen3
1Department of Surgery, Overland Park Surgery Center, Overland Park, KS, USA
2Shawnee Mission Medical Center, Shawnee Mission, KS, USA
3Department of Anesthesia, Anesthesia Associates of Kansas City, Overland Park, KS, USA

Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 25 September 2015; accepted 16 January 2016; published 19 January 2016
ABSTRACT
The objective of this retrospective study was to examine the effects of an intraoperative injection of liposome bupivacaine on the quality and duration of postsurgical pain control, patient satisfaction, and opioid use in a cohort of patients undergoing hemorrhoidectomy in an outpatient setting. Patients underwent ambulatory hemorrhoidectomy conducted by a single surgeon. Liposome bupivacaine 266 mg/20 mL was administered via infiltration at the end of surgery. After discharge, pain-related outcomes were assessed via telephone interviews. Outcomes of interest included first onset of pain after surgery, patient-reported pain intensity (0 = no pain; 10 = worst pain imaginable), time to first use of orally administered opioids after surgery, number of opioid tablets consumed postsurgery, and patient’s satisfaction with postsurgical pain control. A total of 95 patients were included; the average number of hemorrhoids excised was 3.0 (median, 2.7) per patient. Mean time to first onset of pain after surgery was 36 hours; mean time to first consumption of postsurgical opioids was 38 hours. Mean pain intensity scores remained <5 through 72 hours after surgery. The average number of opioid analgesic tablets consumed after surgery was 12.4; 13% (12/95) of patients required no postsurgical opioids. Seventy-five percent of patients reported being “very satisfied” or “perfectly satisfied” with their overall pain control. No liposome bupivacaine-related adverse events were observed. A single intraoperative injection of liposome bupivacaine safely facilitated ambulatory hemorrhoidectomy, eliminated the need for intravenous opioids, minimized opioid use, and was associated with high levels of patient satisfaction.
Keywords:
Postoperative Pain, Hemorrhoidectomy, Liposome Bupivacaine, Postoperative Analgesia

1. Introduction
According to practice parameters for the management of hemorrhoids published in 2011, more than 10 million patients in the United States experience hemorrhoidal symptoms [1] . Because operative hemorrhoidectomy is perceived to be an extremely painful procedure, many patients whose hemorrhoids do not respond to conservative office treatments may avoid surgery that would be helpful to them.
A prolonged-release liposomal formulation of bupivacaine (EXPAREL®; bupivacaine liposome injectable suspension, Pacira Pharmaceuticals, Inc., Parsippany, NJ, USA) [2] has been shown to provide prolonged postsurgical analgesia after hemorrhoidectomy [3] and to significantly reduce cumulative post-hemorrhoidectomy pain scores and rescue opioid consumption compared with standard bupivacaine HCl 0.25% injection [4] . Clinical studies conducted to date involving surgical site administration of liposome bupivacaine have revealed no signs of cardiac toxicity [5] [6] .
In an effort to explore the potential benefits of liposome bupivacaine in a high-volume anorectal surgical practice, we examined the effect of intraoperative administration of liposome bupivacaine on the quality and duration of postsurgical pain control, patient satisfaction, and opioid use in a consecutive cohort of patients undergoing hemorrhoidectomy.
2. Methods
This was a nonblinded, retrospective evaluation of liposome bupivacaine use in a cohort of consecutive hem- orrhoidectomy patients operated on by a single surgeon (ABJ) at Overland Park Surgery Center, Overland Park, KS, USA, and Shawnee Mission Medical Center, Shawnee Mission, KS, USA, from September 2012 to October 2013. The patient cohort included male and female adults undergoing hemorrhoidectomy in an outpatient setting under general anesthesia during the study period.
The hemorrhoidectomy procedures were performed using either the Milligan-Morgan [7] (open) or Ferguson [8] (closed) technique. A standardized protocol was used to inject 5 mL of either lidocaine 2% with epinephrine or 5 mL of bupivacaine HCl 0.25% with epinephrine at the base of the hemorrhoids to be removed before making an incision. Surgical dissection was achieved using needle-tip cauterization; a LigaSure™ small-jaw vessel-sealing device (Covidien, Dublin, Ireland) was used adjunctively in some cases. At the conclusion of the hemorrhoidectomy, a total of 266 mg/20 mL of undiluted liposome bupivacaine was injected using a standard- ized technique in each patient; 15 mL was equally infiltrated into 4 quadrants of the deep subcutaneous adipose tissue just outside the sphincter (ischiorectal space) using a 10-mL syringe with a 1.5-inch, 25-gauge needle. The remaining 5 mL of liposome bupivacaine was injected superficially beneath the incision lines, but not into the anal canal or sphincter. In cases where lidocaine was used prior to the incision, 20 minutes were allowed to elapse before liposome bupivacaine was administered. After surgery, all patients had access to orally administered opioid analgesic medications for rescue analgesia; no intravenous opioids were used. Some patients received ketorolac 30 mg intravenously perioperatively. Patients were discharged on the day of surgery. After discharge, the attending surgeon (ABJ) collected data on pain-related outcomes from interviews with patients via telephone or at the first postoperative visit, which was 2 to 6 weeks after surgery. Patients were asked to provide answers as accurately as possible and responded without guidance or leading. Overall, the time between the surgery and interview ranged from 2 weeks to 6 months.
Postsurgical outcome measures included time to first onset of pain after surgery, patient-reported pain intensity based on an 11-point numeric rating scale (NRS; 0 = no pain, 10 = worst pain imaginable) at 12, 24, 48, and 72 hours after surgery, time to first use of orally administered opioids after surgery, number of opioid tablets consumed postsurgery, patient satisfaction with postsurgical pain control based on a 5-point Likert-type scale (0 = not satisfied at all; 4 = perfectly satisfied), and adverse events.
3. Results
A total of 146 adult patients underwent anorectal surgery with liposome bupivacaine injection during the study period. Of these, 95 underwent hemorrhoidectomy, completed the post surgery telephone interviews, and were included in the analysis. The demographic and clinical characteristics of these patients are summarized in Table 1. Fifty-one patients were excluded from the analysis as summarized in Table 2.
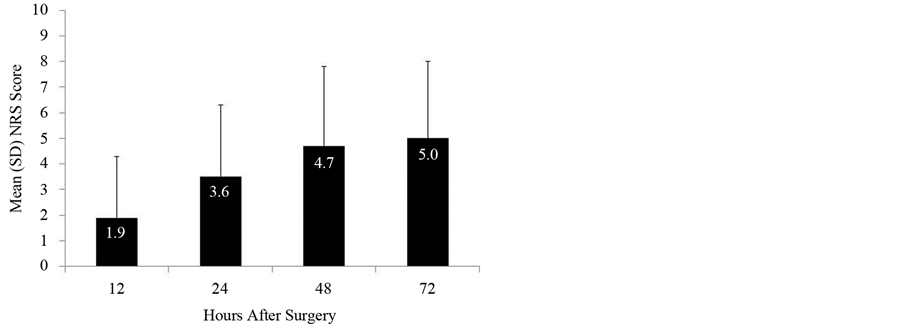
The reported mean time to first onset of pain after surgery was 36 hours and mean time to first consumption of postsurgical opioids was 38 hours. The median times to first onset of postsurgical pain and first consumption of opioids were 24 hours and 30 hours, respectively. Mean pain intensity scores remained ≤5.0 through 72 hours after surgery (Figure 1). The proportion of patients who rated their pain intensity in the 0 - 3 range on the NRS was 79% (75/95) at 12 hours, 51% (48/95) at 24 hours, 35% (33/95) at 48 hours, and 35% (33/95) at 72 hours after surgery.
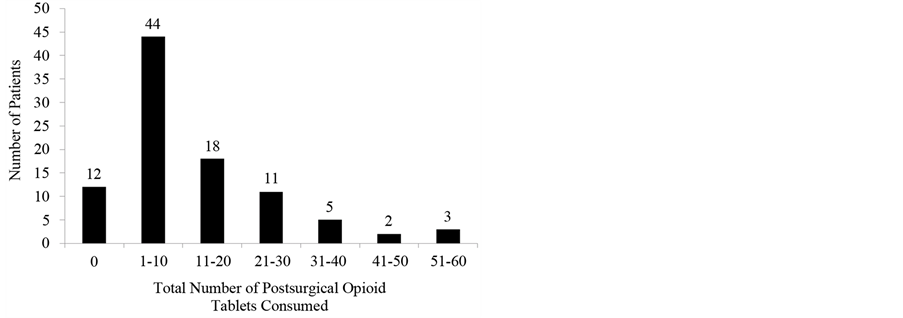
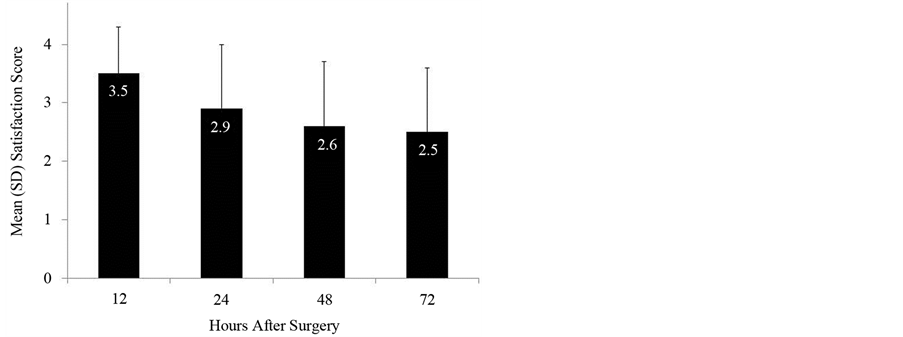
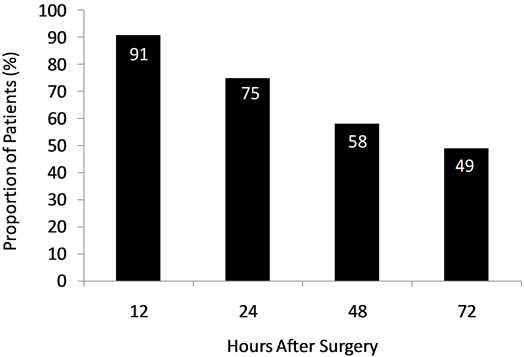
Overall, the mean number of opioid analgesic tablets consumed after surgery was 12.4 (median, 8.0). On average, the emergent surgery subgroup consumed more opioid tablets after surgery (16.7) than the overall study population, and the elective surgery subgroup consumed fewer tablets (11.0). Thirteen percent (12/95) of patients consumed no opioids after surgery; 37% (35/95) consumed ≤3 opioid tablets after surgery (Figure 2). The majority of patients (88%; 84/95) did not require a refill of the prescription for opioid analgesics provided at the time of discharge. Mean patient rating scores for satisfaction with the pain control experience over time are shown in Figure 3. The proportion of patients reporting they were “very satisfied” (satisfaction score = 3) or “perfectly satisfied” (satisfaction score = 4) remained above 70% through 24 hours after surgery (Figure 4). Regarding the entire postsurgical period, 75% of patients reported being “very satisfied” or “perfectly satisfied” with their overall pain control.
There were no liposome bupivacaine-related adverse events and no incidences of urinary retention or cardiac
Table 1. Demographic and clinical characteristics of patients included for analysis.
aOverland Park Surgery Center, Overland Park, KS; bShawnee Mission Medical Center, Shawnee Mission, KS; cHemorrhoidectomies performed for painful, thrombosed, or 4th-degree hemorrhoids.
Table 2. Reasons for patient exclusion.
Abbreviation: IV, intravenous. aOperations included pilonidal cyst excision (n = 6), excision of condyloma acuminata (n = 4), anal sphincterotomy with fissurectomy (n = 2), abscess drainage/fistula surgery (n = 2), fissur- ectomy (n = 1), excision of rectal tumor (n = 1), excision of sebaceous cyst (n = 1); bReasons for overnight hospital admission included late-night surgery, advanced age, medical comorbidities, and extensive hemorrhoid- ectomy.
Figure 1. Mean pain intensity scores through 72 hours after surgery. Abbreviations: NRS, numeric rating scale; SD, standard deviation.
Figure 2. Total number of postsurgical opioid tablets consumed.
Figure 3. Mean patient satisfaction scores through 72 hours after surgery. Abbreviation: SD, standard deviation.
toxicity were observed. One patient who underwent elective hemorrhoidectomy required reoperation for postsurgical bleeding and 1 patient who underwent emergency hemorrhoidectomy required reoperation for fecal impaction. One other patient who underwent emergency hemorrhoidectomy was admitted to the hospital 1 week after surgery due to postsurgical constipation and pain following surgery, but additional surgery was not required.
Figure 4. Proportion of patients reporting “very satisfied” or “perfectly satisfied” scores for postsurgical pain control.
4. Discussion
The anal canal and margin are a pain-sensitive area of the body. The surgical wounds caused by hemorrhoid- ectomy are at the body’s axis with running, walking, and sitting. Further, the anus is difficult to “put at rest” and, by necessity, remains a highly functional zone that must expand with defecation and contract for continence. Because advanced hemorrhoidal disease may only effectively respond to a surgical approach, the painless hem- orrhoidectomy has long been the “Holy Grail” of anorectal surgery.
A plethora of surgical techniques have been devised with the aim of limiting the pain of hemorrhoid surgery. This long list of surgical strategies, including open vs. closed hemorrhoidectomy [9] [10] , lasers [11] [12] , Harmonic® scalpel [13] [14] , LigaSure™ [15] , stapled hemorrhoidopexy [16] , and Doppler-guided hemorrhoid dearterialization [17] , is testament that no one technique has been fully satisfactory in solving the pain problem. In the present series, hemorrhoidectomy was done by either the Milligan-Morgan [7] (open) or Ferguson [8] (closed) method, using a needle-tip electrocautery device and, in some cases, a LigaSure™ small-jaw vessel- sealing device.
Likewise, multiple pharmacologic means have been employed to combat post-hemorrhoidectomy pain, including bupivacaine injection alone [18] [19] , topical glyceryl trinitrate [20] [21] , nifedipine [22] , diltiazem [23] , metronidazole [24] [25] , or sucralfate [26] , as well as botulinum toxin injection [27] , methylene blue injection [28] , and intramuscular ketorolac [29] . Systems to deliver analgesic medication over time, such as patient-con- trolled analgesia pumps and elastomeric infusion pumps [30] , have been used, as have transcutaneous electrical nerve stimulation [31] and both epidural [32] and spinal blocks [33] . Historically, anal stretch was proposed by Goligher [34] to reduce post-hemorrhoidectomy pain and lateral internal anal sphincterotomy also has been proposed as an adjunctive pain-relieving measure [35] . The implicit common goal of these strategies was to reduce postoperative pain and to limit narcotic usage with its attendant risks of constipation and other potentially serious opioid-induced side effects.
In previous studies, intraoperative infiltration of liposome bupivacaine has been shown to be associated with lower cumulative pain scores after hemorrhoidectomy compared with placebo [3] or bupivacaine HCl [4] and to have an acceptable tolerability profile. Clinical pharmacology studies conducted to date have revealed no prolongation of QT interval, electrocardiogram abnormalities, or other cardiac concerns [5] [6] with subcutaneous injection of liposome bupivacaine, and the overall adverse event rate following administration is estimated to be less than 1%, based on aggregated safety data from approximately 600,000 patient exposures [36] . The findings from the present patient series are consistent with those previous reports. We found that liposome bupivacaine injection safely and consistently provided extended postsurgical pain control for hemorrhoidectomy patients and eliminated the need for intravenous narcotics, allowing hemorrhoidectomy to be performed on an ambulatory basis in most cases. Overall, this patient cohort reported high levels of satisfaction with their pain control and the use of oral narcotics was curtailed. We found that liposome bupivacaine injection was transformative for our post-hemorrhoidectomy patients, dramatically changing the overall experience after surgery into one far less painful and more tolerable than we were able to achieve historically in our patients. Even patients with acute painful hemorrhoidal crises were converted to a relatively pain-free state in the immediate postsurgical period and could be discharged home after surgery. Although the use of liposome bupivacaine will not compensate for poor surgical technique, its use should be applicable to any method of hemorrhoidectomy the surgeon prefers.
There were no liposome bupivacaine-related adverse drug events observed in this series. The incidence of complications was low and no patient required readmission due to uncontrolled pain during the first 72 hours after surgery. The goal of reducing opioid use was met; no intravenous narcotics were required before discharge and the overall number of narcotic tablets taken was low (average, 12.4); 13% of patients in the series required no postsurgical narcotics whatsoever. Also, the average time to onset of pain after surgery was 36 hours, and the average patient did not take a narcotic tablet until evening on the day following hemorrhoidectomy (38 hours postsurgery). The observed trends in average pain and patient satisfaction scores appear to indicate that the beneficial analgesic effect of liposome bupivacaine diminished over time during the first 72 hours after surgery. By ameliorating pain on the first night after surgery and inducing a more gradual transition to an awareness of postsurgical pain, the vicious cycle of acute severe pain, anal spasm, reactive narcotic overuse, ileus, constipation, painful defecation and, therefore, increased pain, was interrupted. Because pain was well controlled, patient satisfaction was high.
The ability to perform a hemorrhoidectomy with the expectation on the part of the surgeon and the patient that postsurgical pain will be well controlled is an important advance. Furthermore, physicians may be more willing to recommend surgery as an option for advanced hemorrhoidal disease when postoperative pain is expected to be less. Although more difficult to demonstrate, a reduced need for narcotics in the postoperative period should translate into less opioid-related adverse events, less constipation, and a speedier functional recovery. Without the need for intravenous narcotic analgesics, an overnight hospital stay may be avoided in most cases, sparing valuable hospital resources and reducing costs. Based on its observed potential to provide prolonged postsurgi- cal pain control with an opioid-sparing effect and high patient satisfaction in this patient cohort, liposome bupivacaine may be an effective component of a multimodal pain control strategy for hemorrhoidectomy patients.
This study was limited by its retrospective nature and absence of a control group. The time interval between the hemorrhoidectomy and the interview to collect data on pain-related outcomes was not standardized and ranged from 2 weeks to 6 months. Accurate memory regarding pain may have been variable among patients. In the authors’ experience, however, it is unusual for patients to forget episodes of severe pain. Finally, because the surgeon also conducted the interviews, a form of investigator bias cannot be excluded due to the surgeon-patient relationship.
5. Conclusion
In patients who underwent hemorrhoidectomy in an ambulatory care setting, single-dose infiltration with liposome bupivacaine had the effect of curtailing opioid use and consistently provided prolonged management of postsurgical pain. Even 3-column hemorrhoidectomy and emergent hemorrhoidectomy for painful thrombosis and 4th-degree prolapse were achieved in an ambulatory setting without the need for intravenous narcotics. The majority of patients reported high levels of satisfaction with their postoperative pain control. Liposome bupivacaine was well tolerated and not associated with any adverse events or readmissions due to uncontrolled pain during the first 72 hours after surgery. The use of liposome bupivacaine as part of a multimodal pain protocol represents a potentially important advance in the management of acute postsurgical pain following hemorrhoid- ectomy.
Acknowledgements
Editorial assistance was provided by Peloton Advantage, LLC, supported by Pacira Pharmaceuticals, Inc. The authors were fully responsible for the content, editorial decisions, and opinions expressed in the current article.
Disclosure
Dr. Allen B. Jetmore received grant support from Pacira Pharmaceuticals, Inc. for the development of this man- uscript.
Dr. Douglas Hagen has no conflicts of interest to report.
Cite this paper
Allen B.Jetmore,11,DouglasHagen, (2016) Prolonged Opioid-Sparing Pain Control after Hemorrhoidectomy with Liposome Bupivacaine: Results from a Cohort of 95 Patients. Pain Studies and Treatment,04,5-12. doi: 10.4236/pst.2016.41002
References
- 1. Rivadeneira, D.E., Steele, S.R., Ternent, C., Chalasani, S., Buie, W.D. and Rafferty, J.L. (2011) Practice Parameters for the Management of Hemorrhoids (Revised 2010). Diseases of the Colon & Rectum, 54, 1059-1064. http://dx.doi.org/10.1097/DCR.0b013e318225513d
- 2. Pacira Pharmaceuticals, Inc. (2014) Exparel [Prescribing Information]. Pacira Pharmaceuticals, Inc., Parsippany, NJ.
- 3. Gorfine, S.R., Onel, E., Patou, G. and Krivokapic, Z.V. (2011) Bupivacaine Extended-Release Liposome Injection for Prolonged Postsurgical Analgesia in Patients Undergoing Hemorrhoidectomy: A Multicenter, Randomized, Double- Blind, Placebo-Controlled Trial. Diseases of the Colon & Rectum, 54, 1552-1559. http://dx.doi.org/10.1097/DCR.0b013e318232d4c1
- 4. Haas, E., Onel, E., Miller, H., Ragupathi, M. and White, P.F. (2012) A Double-Blind, Randomized, Active-Controlled Study for Post-Hemorrhoidectomy Pain Management with Liposome Bupivacaine, a Novel Local Analgesic Formulation. The American Surgeon, 78, 574-581.
- 5. Naseem, A., Harada, T., Wang, D., et al. (2012) Bupivacaine Extended Release Liposome Injection Does Not Prolong QTc Interval in a Thorough QT/QTc Study in Healthy Volunteers. Journal of Clinical Pharmacology, 52, 1441-1447. http://dx.doi.org/10.1177/0091270011419853
- 6. Bergese, S.D., Onel, E., Morren, M. and Morganroth, J. (2012) Bupivacaine Extended-Release Liposome Injection Exhibits a Favorable Cardiac Safety Profile. Regional Anesthesia and Pain Medicine, 37, 145-151. http://dx.doi.org/10.1097/AAP.0b013e31823d0a80
- 7. Milligan, E.T.C. and Morgan, C.N. (1937) Surgical Anatomy of the Anal Canal and Operative Treatment of Haemorrhoids. Lancet, 2, 1119-1124. http://dx.doi.org/10.1016/S0140-6736(00)88465-2
- 8. Ferguson, J.A. and Heaton, J.R. (1959) Closed Hemorrhoidectomy. Diseases of the Colon & Rectum, 2, 176-179. http://dx.doi.org/10.1007/BF02616713
- 9. Ho, Y.H., Seow-Choen, F., Tan, M. and Leong, A.F. (1997) Randomized Controlled Trial of Open and Closed Haemorrhoidectomy. British Journal of Surgery, 84, 1729-1730. http://dx.doi.org/10.1002/bjs.1800841223
- 10. Arbman, G., Krook, H. and Haapaniemi, S. (2000) Closed Vs. Open Hemorrhoidectomy—Is There Any Difference? Diseases of the Colon & Rectum, 43, 31-34. http://dx.doi.org/10.1007/BF02237240
- 11. Salfi, R. (2009) A New Technique for Ambulatory Hemorrhoidal Treatment. Coloproctology, 31, 99-103. http://dx.doi.org/10.1007/s00053-009-0009-7
- 12. Wang, J.Y., Chang-Chien, C.R., Chen, J.S., Lai, C.R. and Tang, R.P. (1991) The Role of Lasers in Hemorrhoidectomy. Diseases of the Colon & Rectum, 34, 78-82. http://dx.doi.org/10.1007/BF02050213
- 13. Armstrong, D.N., Frankum, C., Schertzer, M.E., Ambroze, W.L. and Orangio, G.R. (2002) Harmonic Scalpel Hemorrhoidectomy: Five Hundred Consecutive Cases. Diseases of the Colon & Rectum, 45, 354-359. http://dx.doi.org/10.1007/s10350-004-6182-4
- 14. Chung, C.C., Ha, J.P., Tai, Y.P., Tsang, W.W. and Li, M.K. (2002) Double-Blind, Randomized Trial Comparing Harmonic Scalpel Hemorrhoidectomy, Bipolar Scissors Hemorrhoidectomy, and Scissors Excision: Ligation Technique. Diseases of the Colon & Rectum, 45, 789-794. http://dx.doi.org/10.1007/s10350-004-6299-5
- 15. Thorbeck, C.V. and Montes, M.F. (2002) Haemorrhoidectomy: Randomised Controlled Clinical Trial of Ligasure Compared with Milligan-Morgan Operation. European Journal of Surgery, 168, 482-484. http://dx.doi.org/10.1080/110241502321116497
- 16. Senagore, A.J., Singer, M., Abcarian, H., et al. (2004) A Prospective, Randomized, Controlled Multicenter Trial Comparing Stapled Hemorrhoidopexy and Ferguson Hemorrhoidectomy: Perioperative and One-Year Results. Diseases of the Colon & Rectum, 47, 1824-1836. http://dx.doi.org/10.1007/s10350-004-0694-9
- 17. De Nardi, P., Capretti, G., Corsaro, A. and Staudacher, C. (2014) A Prospective, Randomized Trial Comparing the Short- and Long-Term Results of Doppler-Guided Transanal Hemorrhoid Dearterialization with Mucopexy versus Excision Hemorrhoidectomy for Grade III Hemorrhoids. Diseases of the Colon & Rectum, 57, 348-353. http://dx.doi.org/10.1097/DCR.0000000000000085
- 18. Chester, J.F., Stanford, B.J. and Gazet, J.C. (1990) Analgesic Benefit of Locally Injected Bupivacaine after Hemorrhoidectomy. Diseases of the Colon & Rectum, 33, 487-489. http://dx.doi.org/10.1007/BF02052143
- 19. Jirasiritham, S., Tantivitayatan, K. and Jirasiritham, S. (2004) Perianal Blockage with 0.5% Bupivacaine for Postoperative Pain Relief in Hemorrhoidectomy. Journal of the Medical Association of Thailand, 87, 660-664.
- 20. Karanlik, H., Akturk, R., Camlica, H. and Asoglu, O. (2009) The Effect of Glyceryl Trinitrate Ointment on Posthemorrhoidectomy Pain and Wound Healing: Results of a Randomized, Double-Blind, Placebo-Controlled Study. Diseases of the Colon & Rectum, 52, 280-285. http://dx.doi.org/10.1007/DCR.0b013e31819c98a7
- 21. Wasvary, H.J., Hain, J., Mosed-Vogel, M., Bendick, P., Barkel, D.C. and Klein, S.N. (2001) Randomized, Prospective, Double-Blind, Placebo-Controlled Trial of Effect of Nitroglycerin Ointment on Pain after Hemorrhoidectomy. Diseases of the Colon & Rectum, 44, 1069-1073. http://dx.doi.org/10.1007/BF02234622
- 22. Perrotti, P., Dominici, P., Grossi, E., Cerutti, R. and Antropoli, C. (2010) Topical Nifedipine with Lidocaine Ointment versus Active Control for Pain after Hemorrhoidectomy: Results of a Multicentre, Prospective, Randomized, Double- Blind Study. Canadian Journal of Surgery, 53, 17-24.
- 23. Silverman, R., Bendick, P.J. and Wasvary, H.J. (2005) A Randomized, Prospective, Double-Blind, Placebo-Controlled Trial of the Effect of a Calcium Channel Blocker Ointment on Pain after Hemorrhoidectomy. Diseases of the Colon & Rectum, 48, 1913-1916. http://dx.doi.org/10.1007/s10350-005-0135-4
- 24. Nicholson, T.J. and Armstrong, D. (2004) Topical Metronidazole (10 Percent) Decreases Posthemorrhoidectomy Pain and Improves Healing. Diseases of the Colon & Rectum, 47, 711-716. http://dx.doi.org/10.1007/s10350-003-0129-z
- 25. Ala, S., Saeedi, M., Eshghi, F. and Mirzabeygi, P. (2008) Topical Metronidazole Can Reduce Pain after Surgery and Pain on Defecation in Postoperative Hemorrhoidectomy. Diseases of the Colon & Rectum, 51, 235-238. http://dx.doi.org/10.1007/s10350-007-9174-3
- 26. Gupta, P.J., Heda, P.S., Kalaskar, S. and Tamaskar, V.P. (2008) Topical Sucralfate Decreases Pain after Hemorrhoidectomy and Improves Healing: A Randomized, Blinded, Controlled Study. Diseases of the Colon & Rectum, 51, 231- 234. http://dx.doi.org/10.1007/s10350-007-9092-4
- 27. Davies, J., Duffy, D., Boyt, N., Aghahoseini, A., Alexander, D. and Leveson, S. (2003) Botulinum Toxin (Botox) Reduces Pain after Hemorrhoidectomy: Results of a Double-Blind, Randomized Study. Diseases of the Colon & Rectum, 46, 1097-1102. http://dx.doi.org/10.1007/s10350-004-7286-6
- 28. Sim, H.L. and Tan, K.Y. (2014) Randomized Single-Blind Clinical Trial of Intradermal Methylene Blue on Pain Reduction after Open Diathermy Haemorrhoidectomy. Colorectal Disease, 16, O283-O287. http://dx.doi.org/10.1111/codi.12587
- 29. O’Donovan, S., Ferrara, A., Larach, S. and Williamson, P. (1994) Intraoperative Use of Toradol Facilitates Outpatient Hemorrhoidectomy. Diseases of the Colon & Rectum, 37, 793-799. http://dx.doi.org/10.1007/BF02050144
- 30. Ilfeld, B.M., Morey, T.E. and Enneking, F.K. (2003) Portable Infusion Pumps Used for Continuous Regional Analgesia: Delivery Rate Accuracy and Consistency. Regional Anesthesia and Pain Medicine, 28, 424-432. http://dx.doi.org/10.1097/00115550-200301000-00004
- 31. Chiu, J.H., Chen, W.S., Chen, C.H., et al. (1999) Effect of Transcutaneous Electrical Nerve Stimulation for Pain Relief on Patients Undergoing Hemorrhoidectomy: Prospective, Randomized, Controlled Trial. Diseases of the Colon & Rectum, 42, 180-185. http://dx.doi.org/10.1007/BF02237124
- 32. Baptista, J.F., Gomez, R.S., Paulo, D.N., Carraretto, A.R., Brocco, M.C. and Silva, J.J. (2014) Epidural Anesthesia with Ropivacaine with or without Clonidine and Postoperative Pain in Hemorrhoidectomies. Acta Cirurgica Brasileira, 29, 201-208. http://dx.doi.org/10.1590/S0102-86502014000300009
- 33. Moreira Jr., H., Moreira, J.P., Isaac, R.R., et al. (2014) Morphine Spinal Block Anesthesia in Patients Who Undergo an Open Hemorrhoidectomy: A Prospective Analysis of Pain Control and Postoperative Complications. Annals of Coloproctology, 30, 135-140. http://dx.doi.org/10.3393/ac.2014.30.3.135
- 34. Goligher, J.C., Graham, N.G., Clark, C.G., De Dombal, F.T. and Giles, G. (1969) The Value of Stretching the Anal Sphincters in the Relief of Post-Haemorrhoidectomy Pain. British Journal of Surgery, 56, 859-861. http://dx.doi.org/10.1002/bjs.1800561117
- 35. Kanellos, I., Zacharakis, E., Christoforidis, E., et al. (2005) Usefulness of Lateral Internal Sphincterotomy in Reducing Postoperative Pain after Open Hemorrhoidectomy. World Journal of Surgery, 29, 464-468. http://dx.doi.org/10.1007/s00268-004-7432-2
- 36. Data on File (2014) Unpublished Results. Pacira Pharmaceuticals, Inc., Parsippany, NJ.
NOTES
*Corresponding author.