Iris Repair after Long-Term Complications of Angle-Supported Phakic Intraocular Lenses
42
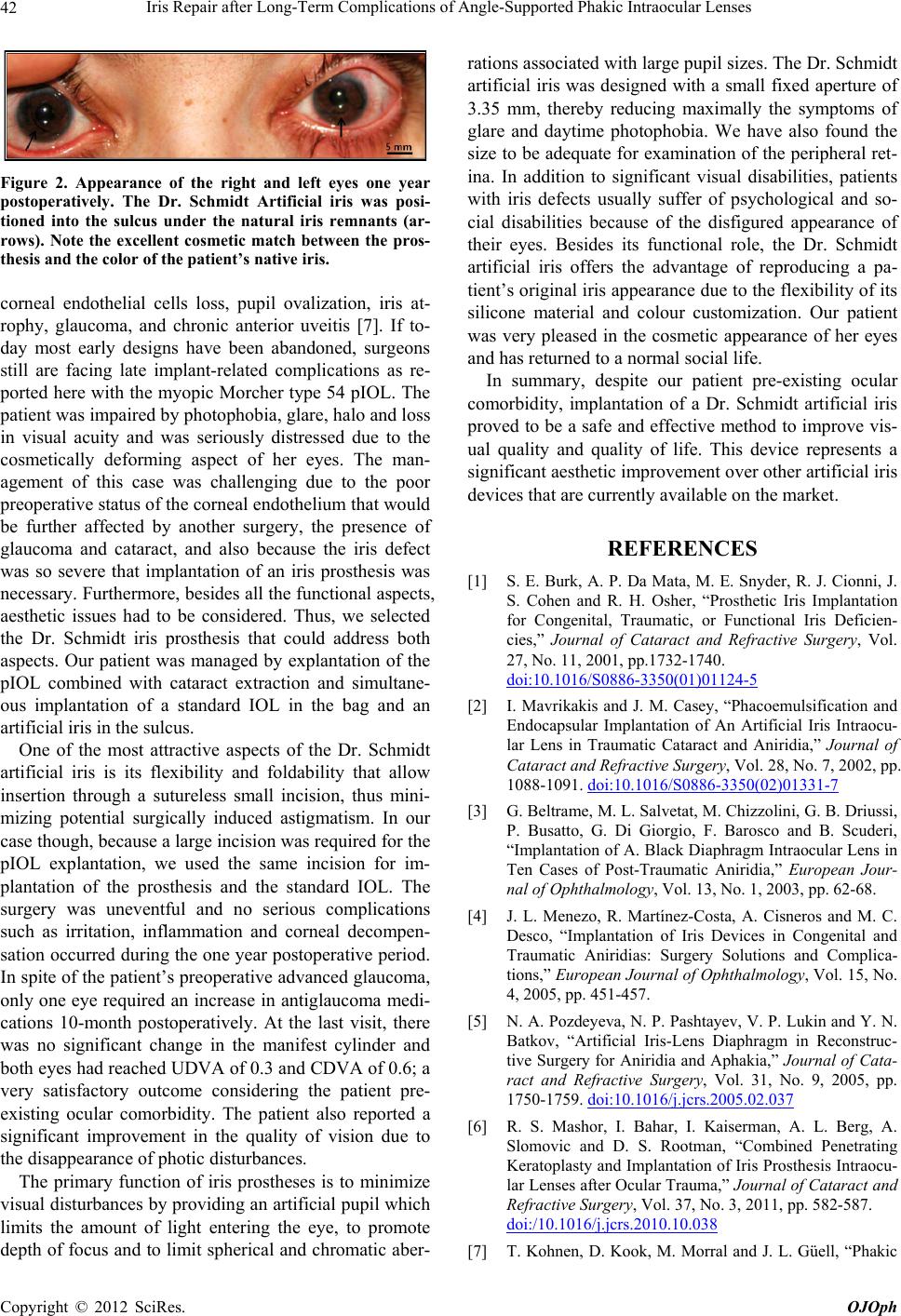
Figure 2. Appearance of the right and left eyes one year
postoperatively. The Dr. Schmidt Artificial iris was posi-
tioned into the sulcus under the natural iris remnants (ar-
rows). Note the excellent cosmetic match between the pros-
thesis and the color of the patient’s native iris.
corneal endothelial cells loss, pupil ovalization, iris at-
rophy, glaucoma, and chronic anterior uveitis [7]. If to-
day most early designs have been abandoned, surgeons
still are facing late implant-related complications as re-
ported here with the myopic Morcher type 54 pIOL. The
patient was impaired by photophobia, glare, halo and loss
in visual acuity and was seriously distressed due to the
cosmetically deforming aspect of her eyes. The man-
agement of this case was challenging due to the poor
preoperative status of the corneal endothelium that would
be further affected by another surgery, the presence of
glaucoma and cataract, and also because the iris defect
was so severe that implantation of an iris prosthesis was
necessary. Furthermore, besides all the functional aspects,
aesthetic issues had to be considered. Thus, we selected
the Dr. Schmidt iris prosthesis that could address both
aspects. Our patient was managed by explantation of the
pIOL combined with cataract extraction and simultane-
ous implantation of a standard IOL in the bag and an
artificial iris in the sulcus.
One of the most attractive aspects of the Dr. Schmidt
artificial iris is its flexibility and foldability that allow
insertion through a sutureless small incision, thus mini-
mizing potential surgically induced astigmatism. In our
case though, because a large incision was required for the
pIOL explantation, we used the same incision for im-
plantation of the prosthesis and the standard IOL. The
surgery was uneventful and no serious complications
such as irritation, inflammation and corneal decompen-
sation occurred during the one year postoperative period.
In spite of the patient’s preoperative advanced glaucoma,
only one eye required an increase in antiglaucoma medi-
cations 10-month postoperatively. At the last visit, there
was no significant change in the manifest cylinder and
both eyes had reached UDVA of 0.3 and CDVA of 0.6; a
very satisfactory outcome considering the patient pre-
existing ocular comorbidity. The patient also reported a
significant improvement in the quality of vision due to
the disappearance of photic disturbances.
The primary function of iris prostheses is to minimize
visual disturbances by providing an artificial pupil which
limits the amount of light entering the eye, to promote
depth of focus and to limit spherical and chromatic aber-
rations associated with large pupil sizes. The Dr. Schmidt
artificial iris was designed with a small fixed aperture of
3.35 mm, thereby reducing maximally the symptoms of
glare and daytime photophobia. We have also found the
size to be adequate for examination of the peripheral ret-
ina. In addition to significant visual disabilities, patients
with iris defects usually suffer of psychological and so-
cial disabilities because of the disfigured appearance of
their eyes. Besides its functional role, the Dr. Schmidt
artificial iris offers the advantage of reproducing a pa-
tient’s original iris appearance due to the flexibility of its
silicone material and colour customization. Our patient
was very pleased in the cosmetic appearance of her eyes
and has returned to a normal social life.
In summary, despite our patient pre-existing ocular
comorbidity, implantation of a Dr. Schmidt artificial iris
proved to be a safe and effective method to improve vis-
ual quality and quality of life. This device represents a
significant aesthetic improvement over other artificial iris
devices that are currently available on the market.
REFERENCES
[1] S. E. Burk, A. P. Da Mata, M. E. Snyder, R. J. Cionni, J.
S. Cohen and R. H. Osher, “Prosthetic Iris Implantation
for Congenital, Traumatic, or Functional Iris Deficien-
cies,” Journal of Cataract and Refractive Surgery, Vol.
27, No. 11, 2001, pp.1732-1740.
doi:10.1016/S0886-3350(01)01124-5
[2] I. Mavrikakis and J. M. Casey, “Phacoemulsification and
Endocapsular Implantation of An Artificial Iris Intraocu-
lar Lens in Traumatic Cataract and Aniridia,” Journal of
Cataract and Refractive Surgery, Vol. 28, No. 7, 2002, pp.
1088-1091. doi:10.1016/S0886-3350(02)01331-7
[3] G. Beltrame, M. L. Salvetat, M. Chizzolini, G. B. Driussi,
P. Busatto, G. Di Giorgio, F. Barosco and B. Scuderi,
“Implantation of A. Black Diaphragm Intraocular Lens in
Ten Cases of Post-Traumatic Aniridia,” European Jour-
nal of Ophthalmology, Vol. 13, No. 1, 2003, pp. 62-68.
[4] J. L. Menezo, R. Martínez-Costa, A. Cisneros and M. C.
Desco, “Implantation of Iris Devices in Congenital and
Traumatic Aniridias: Surgery Solutions and Complica-
tions,” European Journal of Ophthalmology, Vol. 15, No.
4, 2005, pp. 451-457.
[5] N. A. Pozdeyeva, N. P. Pashtayev, V. P. Lukin and Y. N.
Batkov, “Artificial Iris-Lens Diaphragm in Reconstruc-
tive Surgery for Aniridia and Aphakia,” Journal of Cata-
ract and Refractive Surgery, Vol. 31, No. 9, 2005, pp.
1750-1759. doi:10.1016/j.jcrs.2005.02.037
[6] R. S. Mashor, I. Bahar, I. Kaiserman, A. L. Berg, A.
Slomovic and D. S. Rootman, “Combined Penetrating
Keratoplasty and Implantation of Iris Prosthesis Intraocu-
lar Lenses after Ocular Trauma,” Journal of Cataract and
Refractive Surgery, Vol. 37, No. 3, 2011, pp. 582-587.
doi:/10.1016/j.jcrs.2010.10.038
[7] T. Kohnen, D. Kook, M. Morral and J. L. Güell, “Phakic
Copyright © 2012 SciRes. OJOph