The Causes of Distress in Paediatric Outpatients Receiving Dilating Drops
24
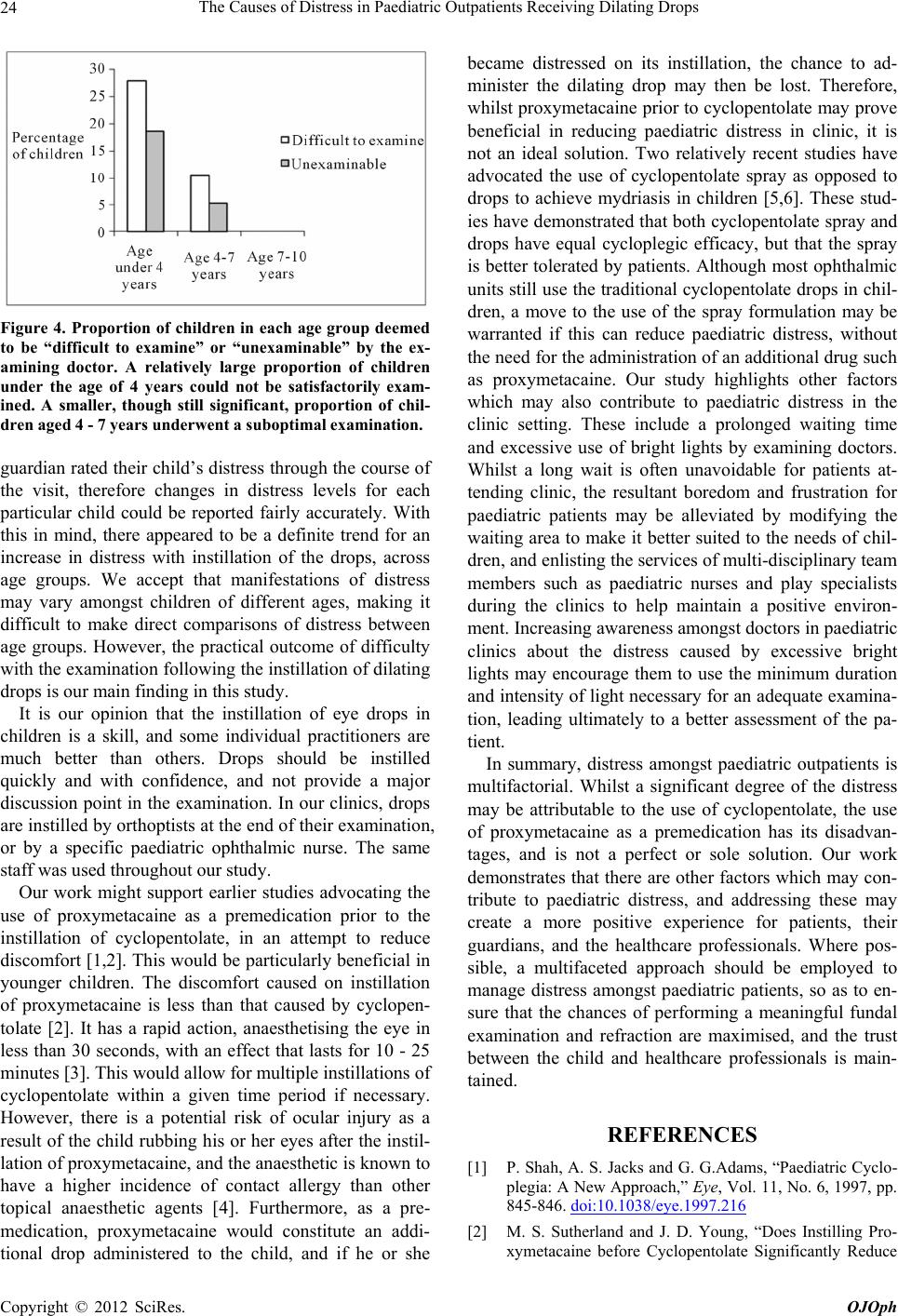
Figure 4. Proportion of children in each age group deemed
to be “difficult to examine” or “unexaminable” by the ex-
amining doctor. A relatively large proportion of children
under the age of 4 years could not be satisfactorily exam-
ined. A smaller, though still significant, proportion of chil-
dren aged 4 - 7 years underwent a suboptimal examination.
guardian rated their child’s distress through the course of
the visit, therefore changes in distress levels for each
particular child could be reported fairly accurately. With
this in mind, there appeared to be a definite trend for an
increase in distress with instillation of the drops, across
age groups. We accept that manifestations of distress
may vary amongst children of different ages, making it
difficult to make direct comparisons of distress between
age groups. However, the practical outcome of difficulty
with the examination followin g the instillation of dilating
drops is our main finding in this study.
It is our opinion that the instillation of eye drops in
children is a skill, and some individual practitioners are
much better than others. Drops should be instilled
quickly and with confidence, and not provide a major
discussion point in the examination. In our clinics, drops
are instilled by orthoptists at th e end of their examination,
or by a specific paediatric ophthalmic nurse. The same
staff was used throughout our study.
Our work might support earlier studies advocating the
use of proxymetacaine as a premedication prior to the
instillation of cyclopentolate, in an attempt to reduce
discomfort [1,2]. This would be particularly beneficial in
younger children. The discomfort caused on instillation
of proxymetacaine is less than that caused by cyclopen-
tolate [2]. It has a rapid action, anaesthetising the eye in
less than 30 seconds, with an effect that lasts for 10 - 25
minutes [3]. This would allow for multiple instillatio ns of
cyclopentolate within a given time period if necessary.
However, there is a potential risk of ocular injury as a
result of the child rubbing h is or her eyes after the instil-
lation of proxymetacaine, and the anaesthetic is known to
have a higher incidence of contact allergy than other
topical anaesthetic agents [4]. Furthermore, as a pre-
medication, proxymetacaine would constitute an addi-
tional drop administered to the child, and if he or she
became distressed on its instillation, the chance to ad-
minister the dilating drop may then be lost. Therefore,
whilst proxymetacaine prior to cyclopentolate may prove
beneficial in reducing paediatric distress in clinic, it is
not an ideal solution. Two relatively recent studies have
advocated the use of cyclopentolate spray as opposed to
drops to achieve mydriasis in children [5,6]. These stud-
ies have demonstrated that both cyclopentolate spray and
drops have equal cycloplegic efficacy, but that the spray
is better tolerated by patients. Although most oph thalmic
units still use th e traditional cyclopentolate drops in ch il-
dren, a move to the use of the spray formulation may be
warranted if this can reduce paediatric distress, without
the need for the administration of an additional drug such
as proxymetacaine. Our study highlights other factors
which may also contribute to paediatric distress in the
clinic setting. These include a prolonged waiting time
and excessive use of bright lights by examining doctors.
Whilst a long wait is often unavoidable for patients at-
tending clinic, the resultant boredom and frustration for
paediatric patients may be alleviated by modifying the
waiting area to make it better suited to the needs of chil-
dren, and en listin g th e services of multi-disciplinary team
members such as paediatric nurses and play specialists
during the clinics to help maintain a positive environ-
ment. Increasing awareness amongst doctors in paediatric
clinics about the distress caused by excessive bright
lights may encourage them to use the minimum duration
and intensity of light necessary fo r an adequate examina-
tion, leading ultimately to a better assessment of the pa-
tient.
In summary, distress amongst paediatric outpatients is
multifactorial. Whilst a significant degree of the distress
may be attributable to the use of cyclopentolate, the use
of proxymetacaine as a premedication has its disadvan-
tages, and is not a perfect or sole solution. Our work
demonstrates that there are other factors which may con-
tribute to paediatric distress, and addressing these may
create a more positive experience for patients, their
guardians, and the healthcare professionals. Where pos-
sible, a multifaceted approach should be employed to
manage distress amongst paediatric patients, so as to en-
sure that the chances of performing a meaningful fundal
examination and refraction are maximised, and the trust
between the child and healthcare professionals is main-
tained.
REFERENCES
[1] P. Shah, A. S. Jacks and G. G.Adams, “Paediatric Cyclo-
plegia: A New Approach,” Eye, Vol. 11, No. 6, 1997, pp.
845-846. doi:10.1038/eye.1997.216
[2] M. S. Sutherland and J. D. Young, “Does Instilling Pro-
xymetacaine before Cyclopentolate Significantly Reduce
Copyright © 2012 SciRes. OJOph