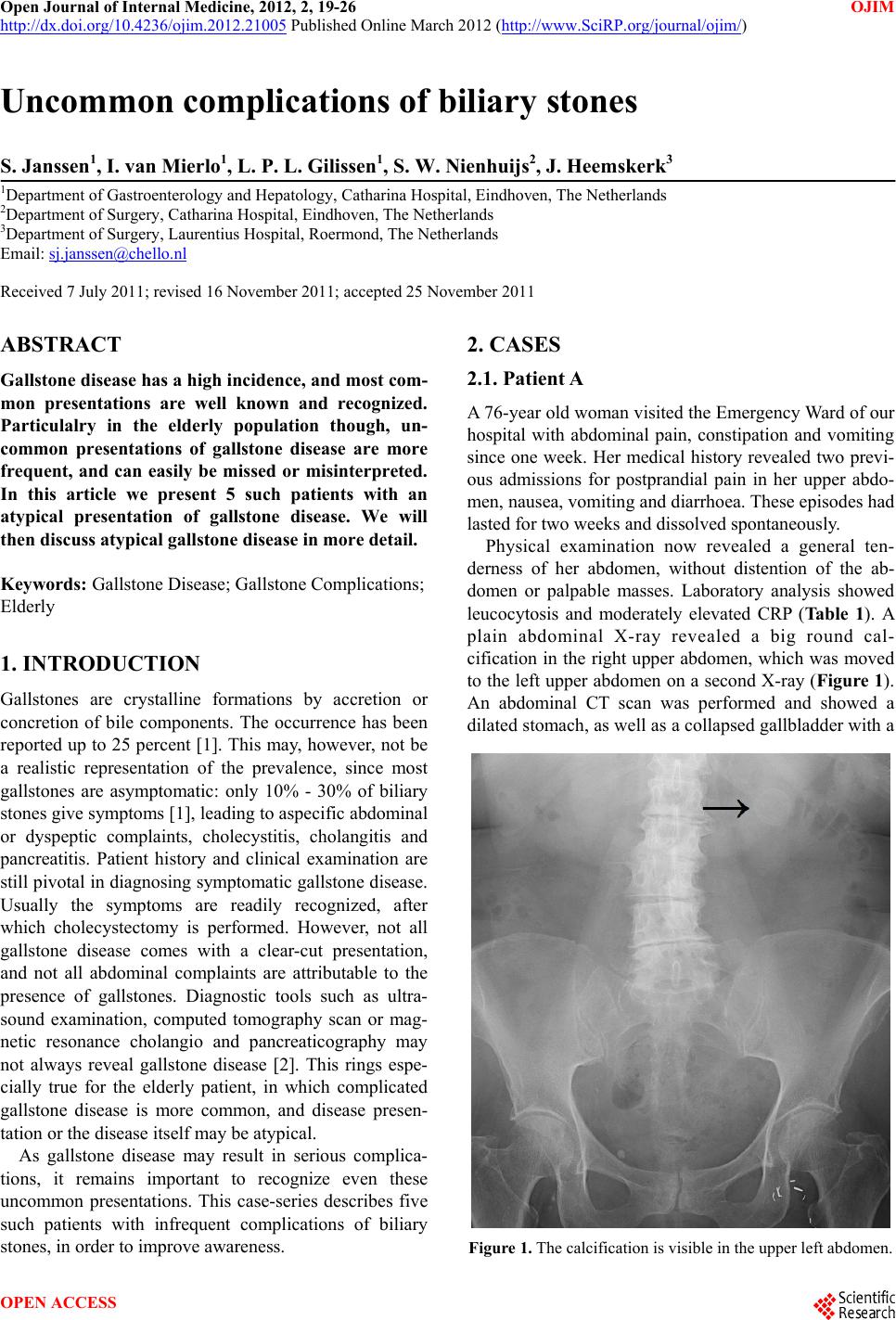
 Open Journal of Internal Medicine, 2012, 2, 19-26 OJIM http://dx.doi.org/10.4236/ojim.2012.21005 Published Online March 2012 (http://www.SciRP.org/journal/ojim/) Uncommon complications of biliary stones S. Janssen1, I. van Mierlo1, L. P. L. Gilissen1, S. W. Nienhuijs2, J. Heemskerk3 1Department of Gastroenterology and Hepatology, Catharina Hospital, Eindhoven, The Netherlands 2Department of Surgery, Catharina Hospital, Eindhoven, The Netherlands 3Department of Surgery, Laurentius Hospital, Roermond, The Netherlands Email: sj.janssen@chello.nl Received 7 July 2011; revised 16 November 2011; accepted 25 November 2011 ABSTRACT Gallstone disease has a high incidence, and most com- mon presentations are well known and recognized. Particulalry in the elderly population though, un- common presentations of gallstone disease are more frequent, and can easily be missed or misinterpreted. In this article we present 5 such patients with an atypical presentation of gallstone disease. We will then discuss atypical gallstone disease in more detail. Keywords: Gallstone Disease; Gallstone Complications; Elderly 1. INTRODUCTION Gallstones are crystalline formations by accretion or concretion of bile components. The occurrence has been reported up to 25 percent [1]. This may, however, not be a realistic representation of the prevalence, since most gallstones are asymptomatic: only 10% - 30% of biliary stones give symptoms [1], leading to aspecific abdominal or dyspeptic complaints, cholecystitis, cholangitis and pancreatitis. Patient history and clinical examination are still pivotal in diagnosing symptomatic gallsto ne disease. Usually the symptoms are readily recognized, after which cholecystectomy is performed. However, not all gallstone disease comes with a clear-cut presentation, and not all abdominal complaints are attributable to the presence of gallstones. Diagnostic tools such as ultra- sound examination, computed tomography scan or mag- netic resonance cholangio and pancreaticography may not always reveal gallstone disease [2]. This rings espe- cially true for the elderly patient, in which complicated gallstone disease is more common, and disease presen- tation or the disease itself may be atypical. As gallstone disease may result in serious complica- tions, it remains important to recognize even these uncommon presentations. This case-series describes five such patients with infrequent complications of biliary stones, in order to improve awareness. 2. CASES 2.1. Patient A A 76-year old woman visited the Emergency Ward of our hospital with abdominal pain, constipation and vomiting since one week. Her medical history revealed two previ- ous admissions for postprandial pain in her upper abdo- men, nause a, vomiting and diarrho ea. These ep isodes had lasted for two weeks and dissolved spontaneously. Physical examination now revealed a general ten- derness of her abdomen, without distention of the ab- domen or palpable masses. Laboratory analysis showed leucocytosis and moderately elevated CRP (Ta bl e 1). A plain abdominal X-ray revealed a big round cal- cification in the right upper abdomen, which was moved to the left upper ab domen on a second X-ray (Figure 1). An abdominal CT scan was performed and showed a dilated stomach, as well as a collaps ed gallblad der with a Figure 1. The calcif icati on i s visibl e in the upp er left abdom en. OPEN ACCESS 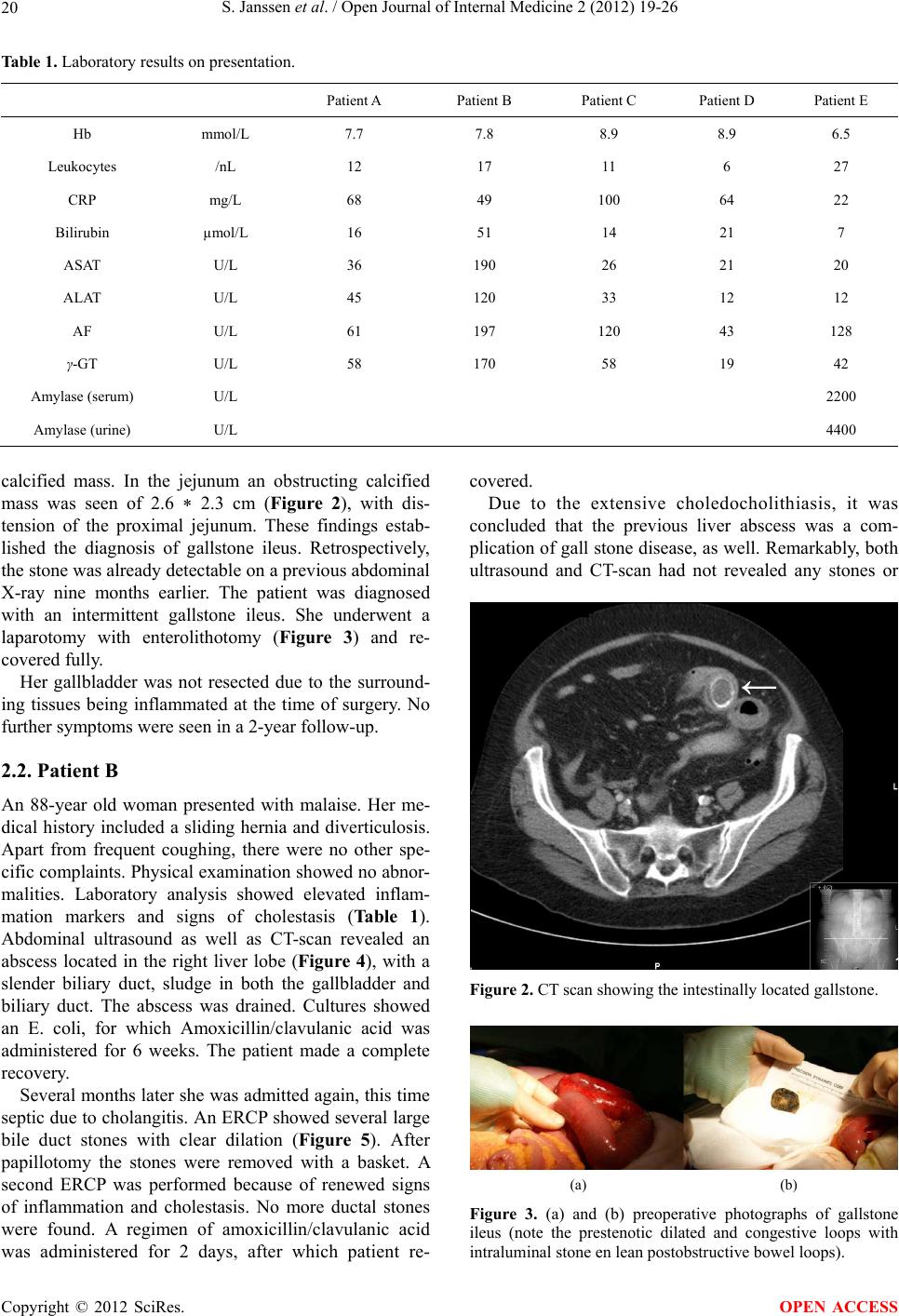 S. Janssen et al. / Open Journal of Internal Medicine 2 (2012) 19-26 20 Table 1. Laboratory results on presentation. Patient A Patient B Patient C Patient D Patient E Hb mmol/L 7.7 7.8 8.9 8.9 6.5 Leukocytes /nL 12 17 11 6 27 CRP mg/L 68 49 100 64 22 Bilirubin µmol/L 16 51 14 21 7 ASAT U/L 36 190 26 21 20 ALAT U/L 45 120 33 12 12 AF U/L 61 197 120 43 128 γ-GT U/L 58 170 58 19 42 Amylase (serum) U/L 2200 Amylase (urine) U/L 4400 calcified mass. In the jejunum an obstructing calcified mass was seen of 2.6 * 2.3 cm (Figure 2), with dis- tension of the proximal jejunum. These findings estab- lished the diagnosis of gallstone ileus. Retrospectively, the stone was already detectable on a previous abdominal X-ray nine months earlier. The patient was diagnosed with an intermittent gallstone ileus. She underwent a laparotomy with enterolithotomy (Figure 3) and re- covered fully. Her gallbladder was not resected due to the surround- ing tissues being inflammated at the time of surgery. No further symptoms were seen in a 2-year follow-up. 2.2. Patient B An 88-year old woman presented with malaise. Her me- dical history included a sliding hernia and diverticulosis. Apart from frequent coughing, there were no other spe- cific complaints. Physical examin ation showed no abnor- malities. Laboratory analysis showed elevated inflam- mation markers and signs of cholestasis (Table 1). Abdominal ultrasound as well as CT-scan revealed an abscess located in the right liver lobe (Figure 4), with a slender biliary duct, sludge in both the gallbladder and biliary duct. The abscess was drained. Cultures showed an E. coli, for which Amoxicillin/clavulanic acid was administered for 6 weeks. The patient made a complete recovery. Several months later she was admitted again, this time septic due to cholang itis. An ERCP showed several large bile duct stones with clear dilation (Figure 5). After papillotomy the stones were removed with a basket. A second ERCP was performed because of renewed signs of inflammation and cholestasis. No more ductal stones were found. A regimen of amoxicillin/clavulanic acid was administered for 2 days, after which patient re- covered. Due to the extensive choledocholithiasis, it was concluded that the previous liver abscess was a com- plication of gall stone disease, as well. Remarkably, both ultrasound and CT-scan had not revealed any stones or Figure 2. CT scan showing the intestinally located gallstone. (a) (b) Figure 3. (a) and (b) preoperative photographs of gallstone ileus (note the prestenotic dilated and congestive loops with intraluminal stone en lean postobstructive bowel loops). Copyright © 2012 SciRes. OPEN ACCESS 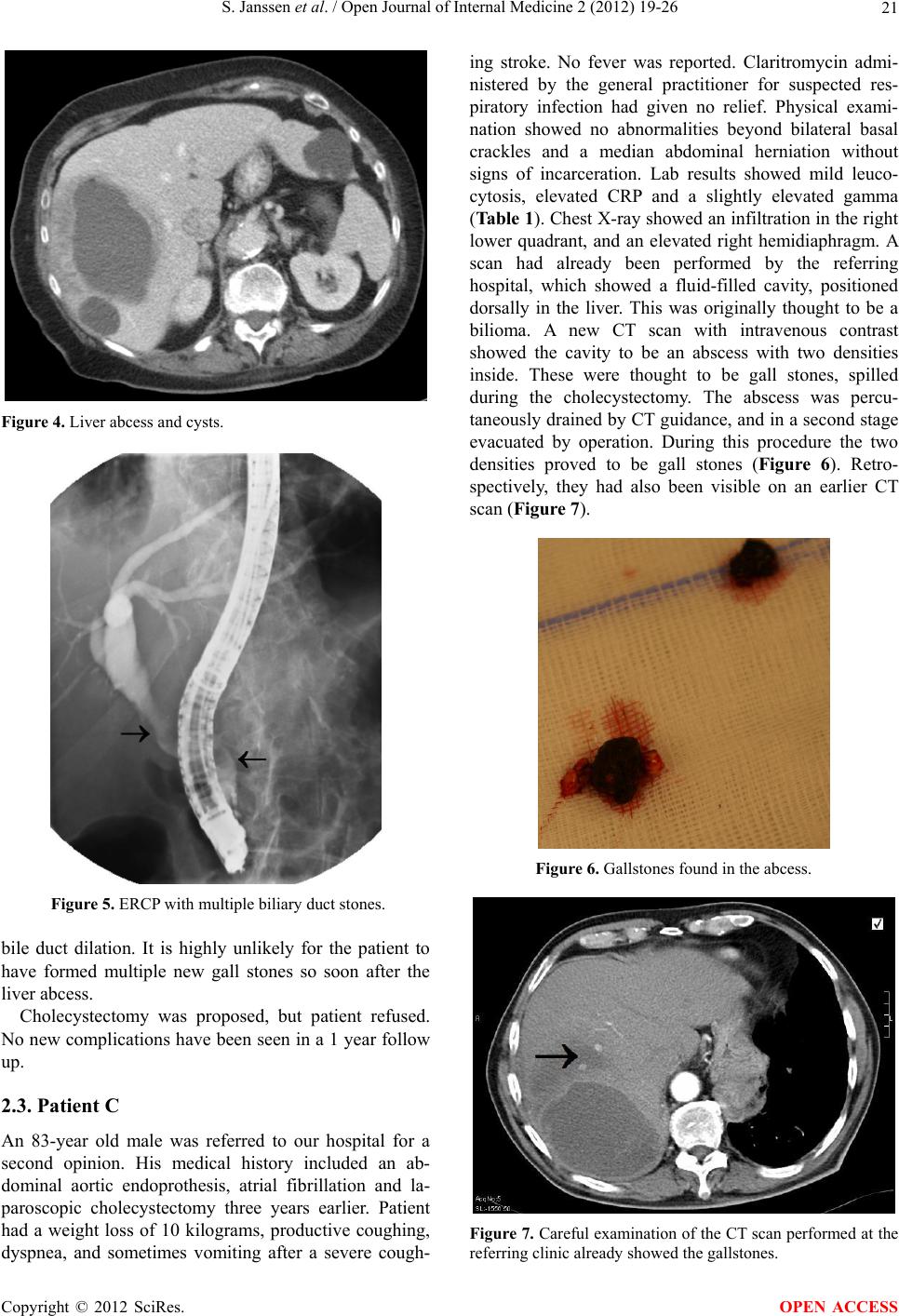 S. Janssen et al. / Open Journal of Internal Medicine 2 (2012) 19-26 21 Figure 4. Liver abcess and cysts. Figure 5. ERCP with multiple biliary duct stones. bile duct dilation. It is highly unlikely for the patient to have formed multiple new gall stones so soon after the liver abcess. Cholecystectomy was proposed, but patient refused. No new complications have been seen in a 1 year follow up. 2.3. Patient C An 83-year old male was referred to our hospital for a second opinion. His medical history included an ab- dominal aortic endoprothesis, atrial fibrillation and la- paroscopic cholecystectomy three years earlier. Patient had a weight loss of 10 kilograms, productive coughing, dyspnea, and sometimes vomiting after a severe cough- ing stroke. No fever was reported. Claritromycin admi- nistered by the general practitioner for suspected res- piratory infection had given no relief. Physical exami- nation showed no abnormalities beyond bilateral basal crackles and a median abdominal herniation without signs of incarceration. Lab results showed mild leuco- cytosis, elevated CRP and a slightly elevated gamma (Table 1). Chest X-ray sh owed an infiltration in the right lower quadrant, and an elevated right hemidiaphragm. A scan had already been performed by the referring hospital, which showed a fluid-filled cavity, positioned dorsally in the liver. This was originally thought to be a bilioma. A new CT scan with intravenous contrast showed the cavity to be an abscess with two densities inside. These were thought to be gall stones, spilled during the cholecystectomy. The abscess was percu- taneously drained by CT guidance, and in a second stage evacuated by operation. During this procedure the two densities proved to be gall stones (Figure 6). Retro- spectively, they had also been visible on an earlier CT scan (Figure 7). Figure 6. Gallstones found in the abcess. Figure 7. Careful examination of the CT scan performed at the referring clinic already showed the gallstones. Copyright © 2012 SciRes. OPEN ACCESS 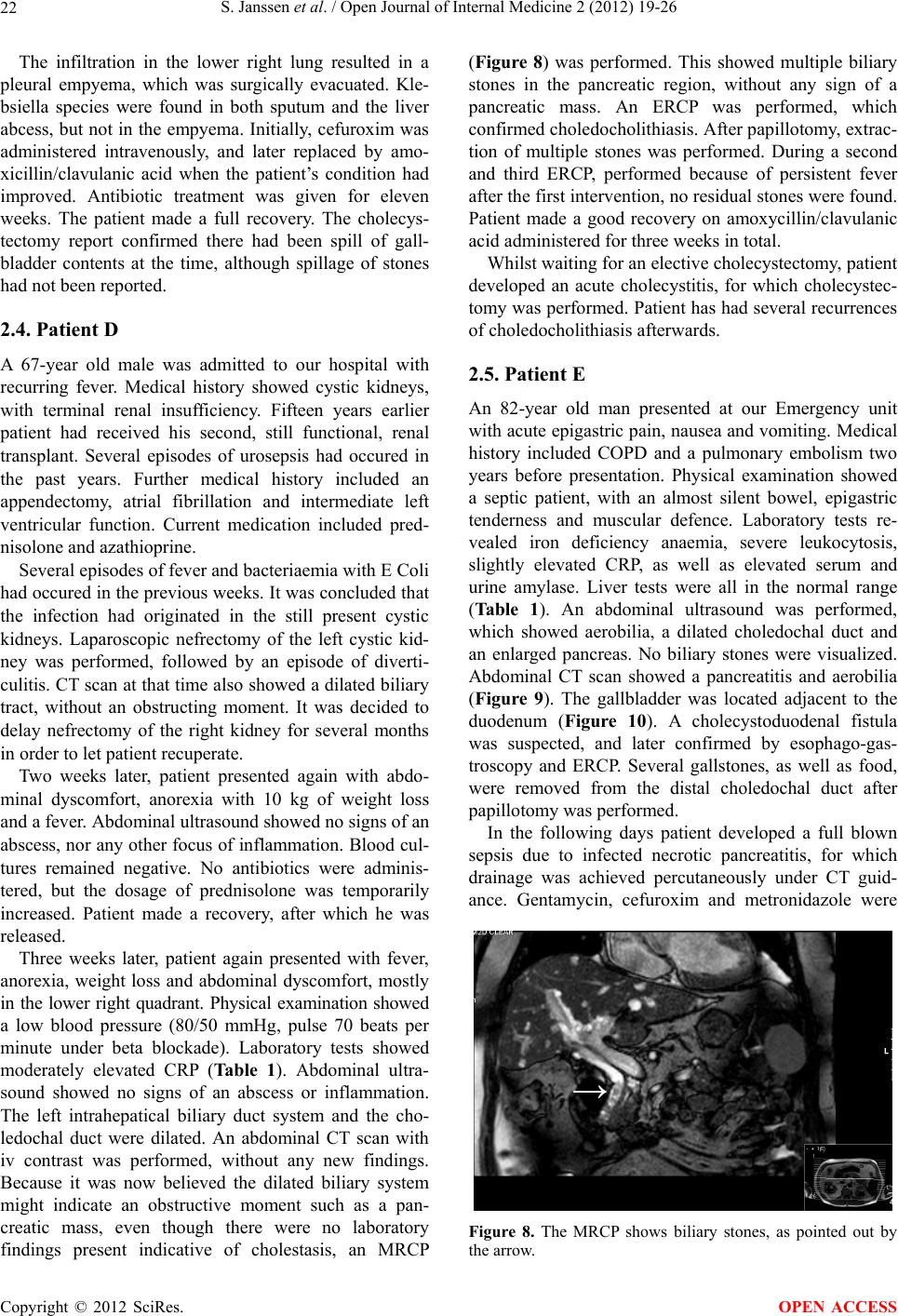 S. Janssen et al. / Open Journal of Internal Medicine 2 (2012) 19-26 22 The infiltration in the lower right lung resulted in a pleural empyema, which was surgically evacuated. Kle- bsiella species were found in both sputum and the liver abcess, but not in the empyema. Initially, cefuroxim was administered intravenously, and later replaced by amo- xicillin/clavulanic acid when the patient’s condition had improved. Antibiotic treatment was given for eleven weeks. The patient made a full recovery. The cholecys- tectomy report confirmed there had been spill of gall- bladder contents at the time, although spillage of stones had not been reported. 2.4. Patient D A 67-year old male was admitted to our hospital with recurring fever. Medical history showed cystic kidneys, with terminal renal insufficiency. Fifteen years earlier patient had received his second, still functional, renal transplant. Several episodes of urosepsis had occured in the past years. Further medical history included an appendectomy, atrial fibrillation and intermediate left ventricular function. Current medication included pred- nisolone and azathioprine. Several episodes of fever and bacteriaemia with E Coli had occured in the previous weeks. It was concluded that the infection had originated in the still present cystic kidneys. Laparoscopic nefrectomy of the left cystic kid- ney was performed, followed by an episode of diverti- culitis. CT scan at that time also showed a dilated biliary tract, without an obstructing moment. It was decided to delay nefrectomy of the right kidney for several months in order to let patient recuperate. Two weeks later, patient presented again with abdo- minal dyscomfort, anorexia with 10 kg of weight loss and a fever. Abdominal ultrasound showed no signs of an abscess, nor any other focu s of inflammation. Blood cul- tures remained negative. No antibiotics were adminis- tered, but the dosage of prednisolone was temporarily increased. Patient made a recovery, after which he was released. Three weeks later, patient again presented with fever, anorexia, weight loss and abdominal dyscomfort, mostly in the lower right quadrant. Physical examination showed a low blood pressure (80/50 mmHg, pulse 70 beats per minute under beta blockade). Laboratory tests showed moderately elevated CRP (Table 1). Abdominal ultra- sound showed no signs of an abscess or inflammation. The left intrahepatical biliary duct system and the cho- ledochal duct were dilated. An abdominal CT scan with iv contrast was performed, without any new findings. Because it was now believed the dilated biliary system might indicate an obstructive moment such as a pan- creatic mass, even though there were no laboratory findings present indicative of cholestasis, an MRCP (Figure 8) was performed. This showed multiple biliary stones in the pancreatic region, without any sign of a pancreatic mass. An ERCP was performed, which confirmed choledocholithiasis. After papillotomy, extrac- tion of multiple stones was performed. During a second and third ERCP, performed because of persistent fever after the first intervention , no residual stones were found. Patient made a good recovery on amoxycillin/clavulanic acid administered for three weeks in total. Whilst waiting for an elective cholecystectomy, patient developed an acute cholecystitis, for which cholecystec- tomy was performed. Patient has had several recurrences of choledocholithiasis afterwards. 2.5. Patient E An 82-year old man presented at our Emergency unit with acute epigastric pain, naus ea and vomiting. Medical history included COPD and a pulmonary embolism two years before presentation. Physical examination showed a septic patient, with an almost silent bowel, epigastric tenderness and muscular defence. Laboratory tests re- vealed iron deficiency anaemia, severe leukocytosis, slightly elevated CRP, as well as elevated serum and urine amylase. Liver tests were all in the normal range (Table 1). An abdominal ultrasound was performed, which showed aerobilia, a dilated choledochal duct and an enlarged pancreas. No biliary stones were visualized. Abdominal CT scan showed a pancreatitis and aerobilia (Figure 9). The gallbladder was located adjacent to the duodenum (Figure 10). A cholecystoduodenal fistula was suspected, and later confirmed by esophago-gas- troscopy and ERCP. Several gallstones, as well as food, were removed from the distal choledochal duct after papillotomy was performed. In the following days patient developed a full blown sepsis due to infected necrotic pancreatitis, for which drainage was achieved percutaneously under CT guid- ance. Gentamycin, cefuroxim and metronidazole were Figure 8. The MRCP shows biliary stones, as pointed out by the arrow. Copyright © 2012 SciRes. OPEN ACCESS  S. Janssen et al. / Open Journal of Internal Medicine 2 (2012) 19-26 23 Figure 9. CT scan showing aerobilia. Figure 10. Same CT scan, showing the close relation between gallbladder and duodenum, respectively on the left and right side of the circle, within an inflamed region. administered. Cultures of the drain fluids showed mul- tiple enteric bacteriae. Blood cultures showed Strepto- coccus anginosus. Antibiotic treatment was then swit- ched to tazobactam/piperacillin. In the following weeks, the patient’s condition fluc- tuated. Via endoscopic ultrasound an enteral drainage of the abscess was achieved several times. In spite of this, his condition eventually deteriorated, and the patient died. 3. DISCUSSION With a prevalence of 5% - 25%, and in some groups even up to 75%, gallston e disease is a common illness [1,3-5]. A wide variety of risk factors is currently known (Table 2), amongst which are obesity, female gender, in- creasing age, pregnancy and age. Despite their high Table 2. Risk factors for biliary disease [1,3-5]. Increased age Hormonal effects Female gender Pregnancy Exogenous estrogens Metabolic disorders Obesity Diabetes mellitus Insulin resistance Dyslipidemia Dietary factors High calorie diet High cholesterol diet High carbohydrate diet Low-fiber diet Loss of bile salts Crohn’s disease Rapid weight loss (>1.5 kg/wk) Liver disease Liver cirrhosis, Hepatitis C virus infection Gallbladder stasis Medication: Octreotide, Fibrates, Ceftriaxon Autonomic neuropathy Spinal cord injury Prolonged fasting Long-term total parenteral nutrition Low physical activity Genetic factors Family history Ethnicity Lithogenic gene mutation/polymorphism Miscellaneous Hyperparathyroidism Hemolytic diseases Down’s syndrome Cystic Fibrosis prevalence, only 10% - 30% of gallstones are sym- ptomatic [1,5]. Cholesterol stones account for 80% - 90% of all stones in Western countries [3]. The remainder are pigment stones. If symptomatic, the most common presentation is that of biliary colics or epigastric discomfort [1,3]. More complications of gallstone disease are displayed in Table 3. Gallstone disease usually presents itself by either its complications, or by accidental discovery during diag- nostic investigati ons such as an abdomi nal ultrasound [ 1]. In this article we describe several uncommon pre- sentations of gallstone disease. Both patients A and E presented with a cholecystoduodenal fistula due to stone erosion through the gallbladder wall. In patient A this led to a gallstone ileus. Beyond causing iron deficiency Copyright © 2012 SciRes. OPEN ACCESS  S. Janssen et al. / Open Journal of Internal Medicine 2 (2012) 19-26 24 Table 3. Complications of gallstone disease [3]. Common complications: Anual Risk (%) biliary colic acute cholecystitis symptomatic choledocholithiasis cholangitis obstructed neck of the gallbladder mucocele extra-hepatic cholestasis pancreatitis 1 0.3 0.2 0.04 - 1.5 Rare complications: gallbladder carcinoma liver abscess gallstone ileus gallbladder perforation/cholecysto-duodenal fistula anaemia due to blood loss, gall stone disease also led to an eventually fatal pancreatitis in patient E. Patient B showed a liver abcess, most likely as a complication of intermittent cholestasis and cholangitis due to gallstones. Patient C displayed a hepatic abscess due to gallstone spill during laparoscopic cholecystec- tomy several years earlier. Patient D had intermittent bacteraemias and atypical abdominal complaints under immunosuppressive therapy because of a renal transplant. Despite nephrectomy the bacteraemia relapsed. Even- tually cholelithiasis was revealed, for which stone re- moval and cholecystectomy were performed. Despite this, patient suffered recurrent gall stone disease. Below we will elaborate on these presentations. Gallstone ileus results from recurrent attacks of cho- lecystitis with erosion of a gallstone through a fistula through the adjacent duodenal wall into small intestine [4,6,7]. Normally the fistula will be formed between a gangrenous gallbladder and the duodenum (cholecys- toduodenal fistula). Occasionally the fistula forms bet- ween the gallbladder and other parts of the gastroin- testinal tract [6,7]. Patient E presented which aerobilia on initial imaging, which (ap art from secondary to operation or papillotomy) can only be cau sed by such a fistula [7]. Gallstone ileus accounts for 1% - 3% of mechanical small bowel obstruction [6] and causes up to 25% of cases of non-strangulated small bowel obstruction in patients over 65 years of age [6,7]. Mean age at presen- tation is 65 - 75 years and it is 3 times more common in women than men [6,7]. Clinical sy mptoms may be ileus, intermittent obstipation or diarrhoea, melaena, acute upper gastro-intestinal bleeding and aerobilia [4,6,7]. More than one-thi r d of pat ie n t s present with no history of biliary symptoms and 40% - 50% with a history of symptomatic cholelithiasis [6]. Overall mortality rate varies between 12% - 33% [4,7]. This may be attributed to delayed diagnosis, elderly patients, and coexisting concomitant medical disease. An accurate preoperative diagnosis is made in 20% - 73% of patients [6,7]. CT scanning appears most sensitive to reveal gall stone ileus [6]. Although other treatment modalities, such as ERCP, are e mployed, th e treatment of choice is surgery [6,7]. Enterolithotomy alone has been shown to have a lower mortality rate on both the short and long term than enterolithotomy combined with fistula repair [6]. Re-operation rate for secondary fistula repair or recurrence of ileus were low (10% and 5% - 9% respectively) [6]. Liver abscess is the most common type of visceral abcess, accounting for 48% of visceral abscesses, and 13% of all intra-abdominal abscesses [8]. The incidence of liver abscess has been estimated at 2.3 per 100.000 citizens [9]. It is more common among men (3.3 vs 1.3 per 100.000) [9]. Biliary tract obstruction, due to either malignancy or gallstones, accounts for 40% - 60% of pyogenic liver abscesses [8-10]. Most abscesses are polymicrobial, mostly due to facultative or anaerobic species from the intestinal tract [8,9]. Presentation of liver abscess usually includes fever and abdominal pain, as well as nausea, vomiting, malaise, weight loss and anorexia [9]. Depending on the size and location of the abcess there may be hepatomegaly or jaundice. Imaging should be performed by 4 phase CT scan or ultrasound [8]. The best treatment for hepatic abscess is still uncertain [8,10,11]. Current convention is that treatment should include both drainage, either operatively or radiologically, and long-term antibiotics. The main guide in this is the clinical condition of the patient. Despite optimal treat- ment, mortality of liver abscess remains high. Although usually around 6%, it can be as high as 53% in elderly patients [12,13]. In the case of patient B, it is remarkable that during her first hospital stay, neither abdominal ultrasound, nor CT scan, showed signs of gallstone disease, even though sensitivity of these combined diagnostic tools exceeds 84% and specificity of ultrasound alone is 99% [2,5]. Laparoscopic cholecystectomy is the treatment of choice for both acute cholecystitis and other presenta- tions of symptomatic gallstone disease [4,14,15]. Reduced cost, decreased hospital stay and increased patient satisfaction are amongst the advantages of this technique [15]. On the other hand laparoscopic cholecystectomy has a higher rate of several complications, such as bile duct injury. Some complications are hardly ever seen in open cholecystectomy, such as visceral laceration or gallstone spillage into the abdominal cavity [6]. The incidence of gall bladder perforation during laparoscopic surgery has been reported to be 20% - 40% [6,16,17]. Gallstone spill occurs in 7% - 16% of all laparosco pically performed cholecystectomies [16,17]. Copyright © 2012 SciRes. OPEN ACCESS  S. Janssen et al. / Open Journal of Internal Medicine 2 (2012) 19-26 25 Not much is known about the n atural history of sp illed gallstones. It is estimated that about 2% of all spilled stones give rise to clinical problems [16]. This can occur days to years after the initial surgery [6]. The usual presentation is in the form of an abscess, either intra- abdominally or in the operation tract [6]. Pseudocysts have also been reported [18]. Predisposing factors for developing complications after ston e spill are reported to be older age, male sex, acute cholecystitis at the time of operation, spillage of pigment stones, number of stones (>15) or size of the stone (diameter > 1.5 cm), and perihepatic localization of lost stones [6,17]. If possible, spill of stones should of course be avoided, and re- trieving spilled stones sho uld be considered [6,17]. The age of the patients presented in this article exceeds 65 years in all cases. All of them showed serious morbidity due to gallstone disease. In general, these cases of relatively uncommon, but otherwise well-known complications of gallstone disease, demonstrate that in elderly patients with atypical abdominal complaints gallstone disease should always be considered. Most of the uncommon complications of gallstone disease are more common in the elderly, as is gallstone disease in general. Fifteen percent of men and 24% of women have gallstones at the age of 70. At 90 years, those numbers rise to 24% and 35% respectively [15]. Typical symptoms such as colics, local peritonitis and fever are often absent in these patients. This also counts for immunocompromised patients (HIV patients, use of immunosuppressives or corticosteroids) and patients on hemodialysis, as case D clearly demonstrates. Although surgeons might be hesitant to operate on elderly patients, we would advocate at least serious consideration on a case-to-case basis. Not only is the average patient getting older, but operating on the elderly has been proven to be safe [14,15,19,20,21]. The main reason for higher morbidity among the elderly is comorbidity [14,19,20]. Careful selection and preopera- tive optimalization can mini mize any risk s. So me authors even state this judicous selection and preparation would only be required in those over 80 years [14]. Furthermore, Riall showed that in those elderly patients in whom cholecystectomy is not performed after a first compli- cation of gallstone disease, readmission rate is 38% in the following two years, most of whom require chole- cystectomy. In those operated the readmission rate is only 4% [15] . As mentioned, comorbidity is one of th e main reasons not to operate on elderly patients. Although comorbidity predicts 2-year mortality, lack of definitive therapy in complicated gallstone disease is an independent predictor of mortality, suggesting increased mortality rate in con- servative treatment [15]. 4. CONCLUSION This case series describes several uncommon, but gene- rally known complications of gallstone disease. It is demonstrated that gallstone disease should always be considered in case of elderly or immunocompromised patients with atypical (abdominal) symptoms or radiolo- gic findings. It also shows that in those patients who present with symptomatic gallstone disease, cholecy- stectom y should not b e d ismi ssed easily. REFERENCES [1] Yoo, E.H. and Lee, S.Y. (2009) The prevalence and risk factors for gallstone disease. Clinical Chemistry and La- boratory Medicine, 47, 795-807. doi:10.1515/CCLM.2009.194 [2] Zakko, S. and Ramsby, G. (1990) Role of computed to- mography in assessing gallstones. Radiology Report, 2, 426. [3] Attasaranya, S., Fogel, E.L. and Lehman, G.A. (2008) Choledocholithiasis, ascending cholangitis, and gallstone pancreatitis. Medical Clinics of North America, 92, 925- 960. doi:10.1016/j.mcna.2008.03.001 [4] Sanders, G. and Kingsnorth, A.N. (2007) Gallstones. British Medical Journal, 335, 295-299. doi:10.1136/bmj.39267.452257.AD [5] Marschall, H.U. and Einarsson, C. (2007) Gallstone dis- ease. Journal of Internal Medicine, 261, 529-542. doi:10.1111/j.1365-2796.2007.01783.x [6] Zaliekas, J. and Munson, J.L. (2008) Complications of gallstones: The Mirizzi syndrome, gallstone ileus, gall- stone pancreatitis, complications of “lost” stones. Surgi- cal Clinics of North America, 88, 1345-1368. doi:10.1016/j.suc.2008.07.011 [7] Abou-Saif, A. and Al-Kawas, F.H. (2002) Complications of gallstone disease: Mirizzi syndrome, cholecystochole- dochal fistula, and gallstone ileus. The American Journal of Gastroenterology, 97, 249-254. doi:10.1111/j.1572-0241.2002.05451.x [8] Mezhir, J.J., Fong, Y. and Jacks, L.M. (2010) Current management of pyoegnic liver abscess: Surgery is now second-line treatment. Journal of the American College of Surgeons, 210, 975-983. doi:10.1016/j.jamcollsurg.2010.03.004 [9] Huang, C.-J., Pitt, H.A., Lipsett, P.A., et al. (1996) Pyo- genic hepatic abscess: Changing trends over 42 years. Annals of Surgery, 223, 600-607. doi:10.1097/00000658-199605000-00016 [10] Lam, Y.-H., Wong, S. K.-H., Lee, D.W.-H, et al. (1999) ERCP and pyogenic liver abscess. Gastrointest Endosc, 50, 340-344. doi:10.1053/ge.1999.v50.98065 [11] Ch-Yu, S., Hg-Lo, R., Kan, P.S. and Metreweli, C. (1997) Pyogenic liver abscess: Treatment with needle aspiration. Clinical Radiology, 52, 912-916. doi:10.1016/S0009-9260(97)80223-1 [12] Lee, K.T., Wong, S.R. and Sheen, P.C. (2001) Pyogenic Copyright © 2012 SciRes. OPEN ACCESS  S. Janssen et al. / Open Journal of Internal Medicine 2 (2012) 19-26 Copyright © 2012 SciRes. 26 OPEN ACCESS liver abscess: An audit of 10 years’ experience and ana- lysis of risk factors. Digestive Surgery, 18, 459-465. doi:10.1159/000050194 [13] Sridharan, G.V., Wilkinson, S.P. and Primrose, W.R. (1990) Pyogenic liver abscess in the elderly. Age Ageing, 19, 199-203. doi:10.1093/ageing/19.3.199 [14] Yetkin, G. and Uludag, M. (2009) Laparoscopic chole- cystectomy in elderly patients. Journal of the Society of Laparoendoscopic Surgeons, 13, 587-591. doi:10.4293/108680809X1258998404604 [15] Riall, T.S. and Zhang, D. (2010) Failure to perform cho- lecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. Journal of the American College of Surgeons, 210, 668- 677. [16] Woodfield, J.C., Rodgers, M. and Windsor, J.A. (2004) Peritoneal gallstones following laparoscopic cholecystec- tomy: Incidence, complications, and management. Sur- gical Endoscopy, 18, 1200-1207. doi:10.1007/s00464-003-8260-4 [17] Brockmann, J.G., Kocher, T., Senninger, N.J. and Schür- mann, G.M. (2002) Complications due to gallstones lost during laparoscopic cholecystectomy . Surgical Endoscopy, 16, 1226-1232. doi:10.1007/s00464-001-9173-8 [18] Arishi, A.R., Rabie, M.E., Khan, M.S., Sumaili, H., Shaabi, H., Michael, N.T. and Shekhawat, B.S. (2008) Spilled gallstones: The source of an enigma. Journal of the Society of Laparoendoscopic Surgeons, 12, 321-325. [19] Osman, Y., Ebru, M., Umit, T., Volkan, O., Melih, K., Belma, K., Betul, B., Omer, C. and Atilla, S. (2008) La- paroscopic cholecystectomy in elderly patients. Brati- slava Medical Journal, 109, 313-316. [20] Mayol, J., Martinez-Sarmiento, J., Tamayo, F.J. and Fer- nández-Represa, J.A. (1997) Complications of laparo- scopic cholecystectomy in the ageing patient. Age Ageing, 26, 77-81. doi:10.1093/ageing/26.2.77 [21] Sánchez-Beorlegui, J., Soriano, P., Monsalve, E., Moreno, N., Cabezali, R. and Navarro, A. (2009) Laparoscopic cholecystectomy in octogenarian patients. A comparative study between two geriatric population groups. Cirugía Española, 85, 246-251.
|