Open Journal of Preventive Medicine
Vol.2 No.2(2012), Article ID:19543,9 pages DOI:10.4236/ojpm.2012.22035
Self-reported ischemic heart disease: Prevalence, sociodemographics, health behavior, health-care utilization, and quality of life
![]()
1National Institute of Public Health, University of Southern Denmark, Copenhagen, Denmark; *Corresponding Author: shan.alphin@hotmail.com
2Institute of Food and Resource Economics, Faculty of Life Sciences, University of Copenhagen, Copenhagen, Denmark
3Department of Cardiology, Copenhagen University Hospital, Copenhagen, Denmark
Received 9 January 2012; revised 18 February 2012; accepted 22 March 2012
Keywords: Ischemic Heart Disease; Lifestyle; Health-Care Utilization; Risk Factors; Health-Related Quality of Life; SF-36
ABSTRACT
The aim of this study was to present the prevalence of self-reported Ischemic Heart Disease (IHD) based on a national population-based survey and to characterize people with self-reported IHD with respect to health behavior, risk factors, health-care services utilization and health-related HRQoL; further to compare people with self-reported IHD to those with other chronic illness and people without chronic illness. Based on the Danish Health Interview Survey 2005 (SUSY), a sample of 10,983 persons aged 35 years or older was examined. Data was collected through personal interviews (response rate = 66.7%) and self-administered questionnaires (51.5%). The sample was divided into three mutual exclusive groups: IHD; other chronic illnesses; and no chronic illness. The prevalence of IHD was 5.6% (5.2 - 6.0). The disease was more common in men than women, and the average age was 67.5 years. People with self-reported IHD were characterized as having poorer health behaviors; more risk factors: 40% smokers, 21% sedentary lifestyle, 26% obese; higher utilization of the health-care services; and poorer HRQoL. When compared to people with other chronic diseases, people with IHD continued to show the same characteristics. The IHD group had more problems affecting their daily lives than the other two groups. The issues that affected the people with IHD have also been shown to increase the load on the health-care system. Therefore, it is important to the patients, health-care, and society that the prevalence of IHD is reduced and the burden of disease is made a priority.
1. INTRODUCTION
In 2005, the World Health Organization projected that 60% of the deaths worldwide would be caused by chronic diseases [1]. The top four chronic diseases are: cardiovascular disease, cancer, chronic respiratory disease, and diabetes [1]. Cardiovascular disease is the leading cause of death, responsible for 30% of all deaths worldwide [1,2]. However, mortality from cardiovascular disease has declined over the past decade in many Western countries [1], including Denmark [3].
As the mortality rates have declined in Denmark, there has been a documented increase in the rate of hospitalization due to ischemic heart disease (IHD) [3]. This reflects changes in morbidity, risk factor modification, and the treatment of IHD within the healthcare system [3]. Thus, the improved survival rate implies that more people are living with the disease and IHD appears to be transforming from a fatal to a chronic disease.
The impact of chronic disease is both a major cost and economic burden to individuals, health systems, and societies [1]. Furthermore, chronic diseases are slow to develop and can lead to compounding medical complications, premature death, and lower health-related quality of life (HRQoL) [2]. In Denmark it has been reported that individuals with heart disease cost the healthcare system on average 3196 more per person than individuals without heart disease [4].
Previous research conducted with people living with IHD has mainly been based on data from national or regional hospital registries [3-5], however this data only reflects the number of people with chronic IHD in contact with the healthcare system. From a public health perspective, it is important to know how many people are living in society with chronic IHD and how their everyday life is affected.
In cross-sectional surveys among people aged > 50 years, Oldridge and Stump found a significantly greater likelihood of limitation of activity and poor or fair selfrated health among respondents with heart disease compared to people with other kinds of chronic illness [5]. No similar studies have given a broader description of how health behavior, HRQoL, and use of health services are affected among people living with IHD. Health behavior, or prevalence of risk factors for heart diseases, are well-known in relation to the general population [5] and cardiac patients [6-8]. Most of the information on HRQoL among people with IHD is based on follow-up studies of hospitalized patients [9,10], while information is lacking on the HRQoL of people living with chronic IHD outside of the healthcare setting.
The aim of this study is to present the prevalence of self-reported IHD based on a national population-based survey and to characterize people with self-reported IHD with respect to health behavior, risk factors, health-care services utilization and health-related HRQoL; further to compare people with self-reported IHD to those with other chronic illness and people without chronic illness.
2. METHODS
2.1. Sample
The Danish Health Interview Survey 2005 (SUSY) was conducted by the National Institute of Public Health [5]. The purpose of the survey was to describe the status and trends in health and morbidity in the adult population and the factors that influence health status, including health behavior and health habits, lifestyles, environmental and occupational health risks and health resources [5]. The study was based on a representative sample of 21,183 Danes aged 16 or older. The data was collected by personal interview in the respondent’s home followed by a self-administered questionnaire distributed after the interview [5]. The questions for both the interview [11] and the self-administered questionnaire [12] can be found elsewhere. There were 14,566 interviews conducted at a response rate of 66.7% and 11,238 self-administered questionnaires were returned at a response rate of 51.5% [5]. Using the SUSY 2005 data, a sample of 10,983 respondents aged 35 years or older was obtained; 17 were excluded because of missing data.
2.2. Clinical and Demographic Measures
During the interview participants were asked two key questions, with subsequent follow-up questions. First they were asked, “Do you have any chronic disease, disorder or illness, chronic effects of injury, any functional impairment or any other chronic health problem?” If the answer was “yes”, then the participant was asked two follow-up questions: “What kind of disease?” and “Where in your body is the disease located?” The second key question asked them specifically, “Do you now or have you previously had a heart attack (myocardial infarction) or angina pectoris?”
Based on the interview responses the study sample was divided into three mutually exclusive groups:
• Participants with IHD: respondents giving a “yes” answer to one or both questions (n = 630);
• Participants with other chronic illnesses (e.g. musculoskeletal disease, respiratory disease, diseases of the nervous system) (n = 4353);
• Participants with no chronic illness (n = 5983).
All reported chronic illnesses were subsequently coded according to the International Classification of Diseases, 10th revision (ICD-10). The chronic illness breakdown is illustrated for both the IHD group and other chronic illness group in Table 1.
The other data collected can be categorized into seven major areas: sociodemographic, health behaviors, risk factors, healthcare system utilization, medication use, social relations and HRQoL. Standard socio-demographic data was collected during the interview including: gender, age, cohabitation status and educational level. The questions concerning health behaviors and risk factors included smoking pattern, level of physical activity, dietary intake, prevalence of hypertension and diabetes, use of preventive check-ups, self-efficacy [13] and height/ weight for BMI calculations.
Six questions in the interview addressed the use of physician services within the past three months and four questions asked about the use of other health-care providers within the same time period. Participants were also asked if they were regularly taking medication. Questions concerning quality of life included social relations, self-rated health, chronic activity limitations and self-rated HRQoL. There were three questions regarding social relations during the interview. Self-rated HRQoL measurement were collected from the self-administered questionnaire and based on the SF-36 [14,15]. Questions on sexual activity were also included in the self-administered questionnaire.
2.3. Data Analysis and Statisitics
Raw prevalence and 95% confidence intervals are presented for the IHD group only. When comparing the three groups prevalences are adjusted for both age and gender and presented with 95% confidence intervals. To test for equal prevalences in the groups, a test for conditional independence [16] was used which takes into account the discrete nature of risk factors. All analyses were performed in SAS, version 9.1.
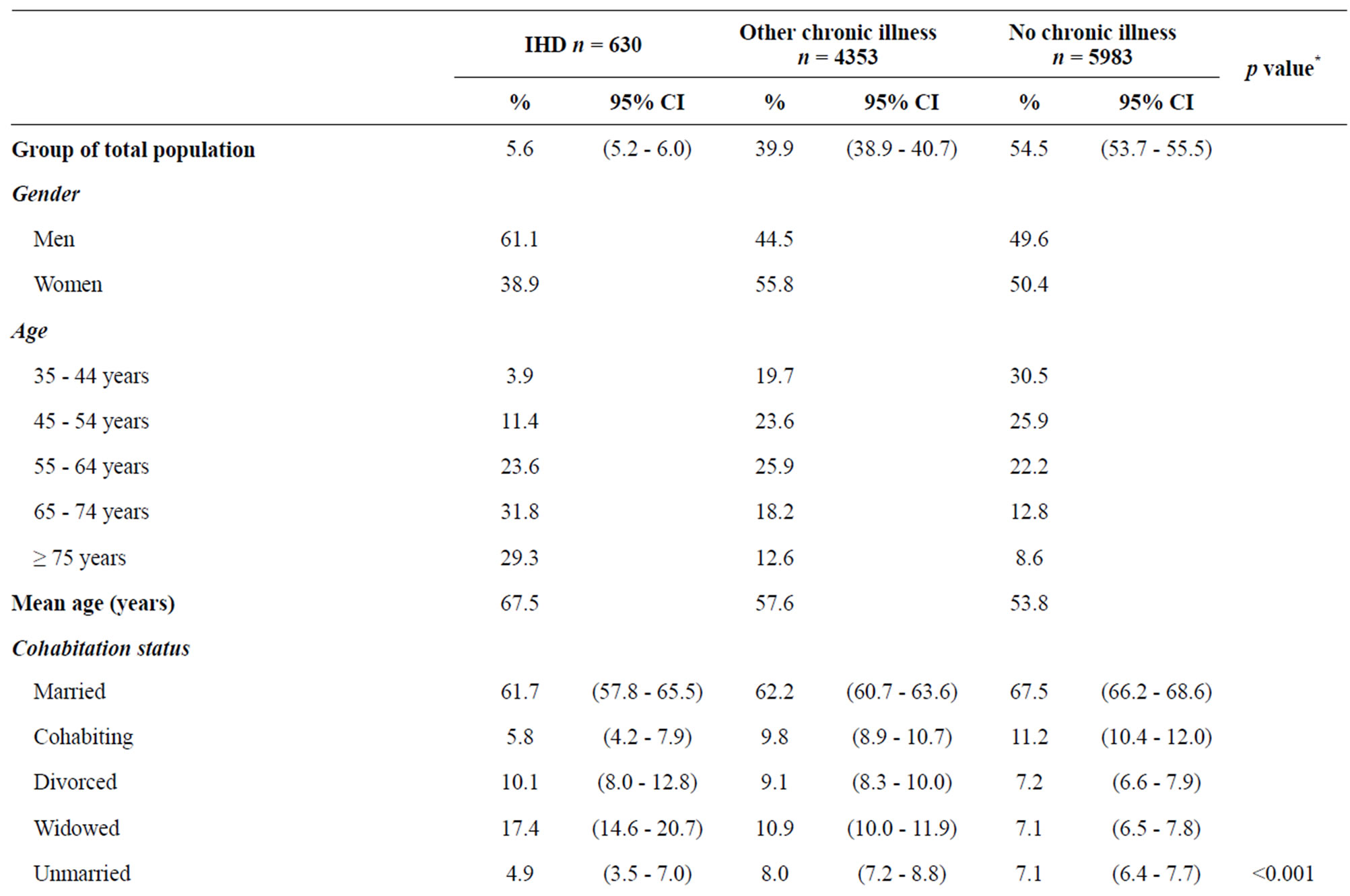
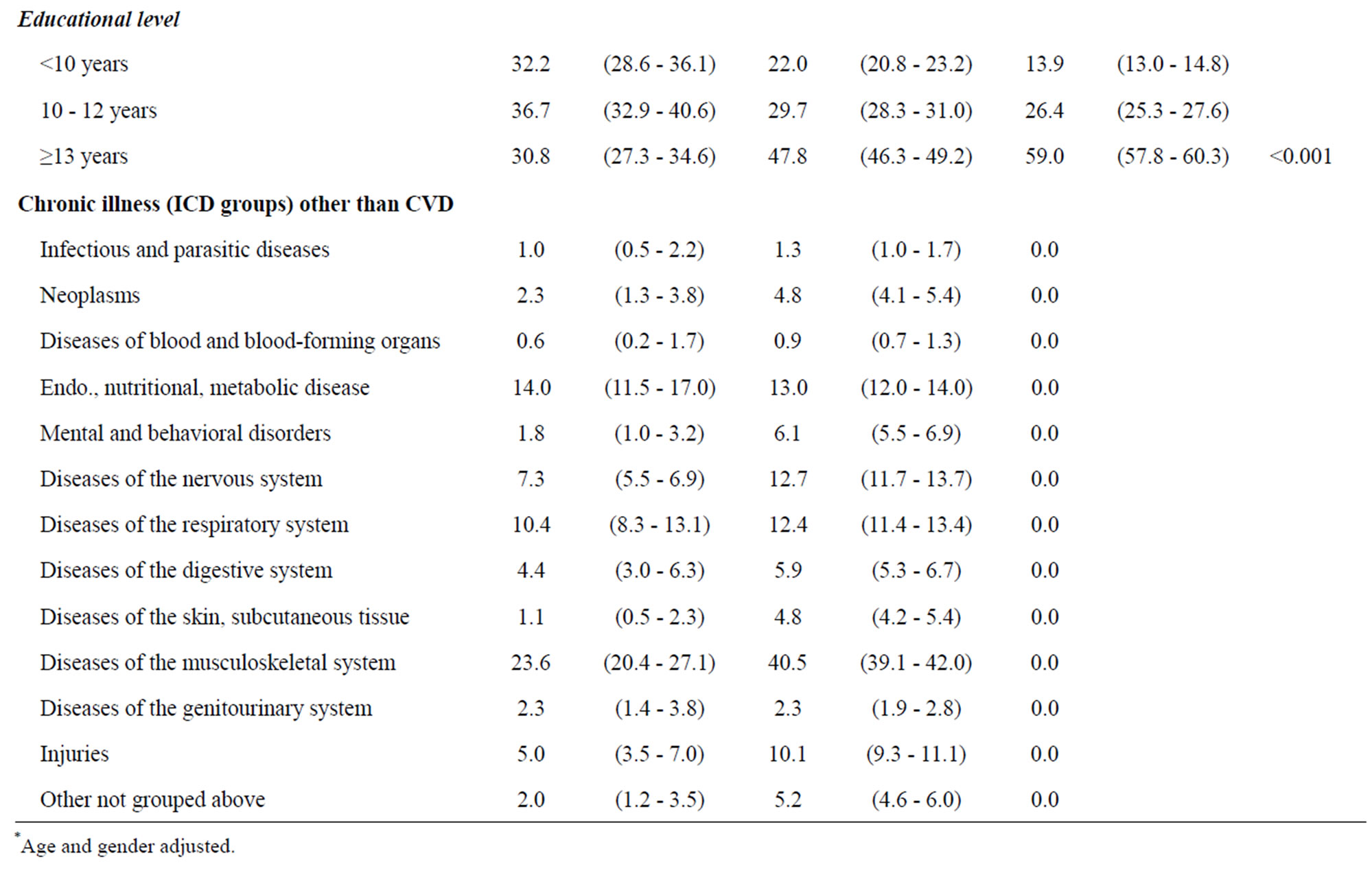
Table 1. Sociodemographic characteristics and chronic illness of people with self-reported ischemic heart disease (IHD), other chronic illness and no chronic illness.
3. RESULTS
A total of 630 respondents reported having IHD, corresponding to 5.6% (95% CI 5.2% - 6.0%) of adult Danes aged 35 years or older. Table 1 shows the sociodemographic characteristics. There were more men than women in the IHD group, and people with IHD were an average of 10 years older than those with other chronic illness and almost 14 years older than those without illness. Corresponding to the age differences, the IHD group included more widowers than the other groups, even after age and gender were controlled. Educational level was clearly lower in the IHD group.
3.1. Cormorbidity
The comorbidities for the IHD group and the other chronic illness group are shown in Table 1. Some of the respondents in the IHD group reported other chronic illnesses in addition IHD. The IHD group’s most reported diseases included: musculoskeletal disease (23.6%); endocrine/metabolic disease (14.0%); respiratory disease (10.4%); nervous system disease (7.3%); and other injuries (5.0%). The other chronic illness group’s major chronic diseases are as follows: musculoskeletal disease (40.5%), endocrine/metabolic disease (13.0%), nervous system disease (12.7%), respiratory disease (12.4%) and other injuries (10.1%).
3.2. Health Behavior and Risk Factors
Health behavior and risk factors among people with IHD differed significantly from the two other groups (Table 2). The IHD group had fewer “never smokers” but more “smokers” and “former smokers” compared to the other two groups (p < 0.001). The IHD group is more sedentary and participating in less in heavy physical activity, however there is little difference between the three groups in regards to self-reported moderate physical activity. Dietary behavior also did not differ between the groups. Obesity, as represented by BMI, was significantly more prevalent in the IHD group (26.0%; (95% CI: 20.5% - 31.5%)) than in the group with other chronic illness (15.8%; (95% CI: 14.7% - 16.9%)) and the group without illness (9.6%; (95% CI: 8.8% - 10.4%)) (p < 0.001). Furthermore, people with IHD had lower selfefficacy (confidence that their own effort is important in staying healthy [12]). Attendance for preventive health check-ups was significantly more frequent in the IHD group (87.8%); (95% CI: 84.1% - 91.5%) than in the group with other illness (70.6%); (95% CI: 69.2% - 71.9%) and in the group with no illness (54.2%); (95% CI: 53.0% - 55.5%) (p < 0.001). Similar patterns were seen for blood pressure and cholesterol preventive visits. Hypertension and diabetes, which are well-known risk factors for IHD, were significantly more prevalent in the IHD group compared to the other two groups.
3.3. Use of Health-Care Services
Health-care utilization varied considerably between the two disease groups and the group without disease (Table 3). Use of general practitioners, outpatient clinics and hospitalization was significantly more frequent in the IHD group than in the group with other chronic illness. A total of 84.4% of the IHD group stated that they regularly or continually took medicine and this proportion was significantly higher than the chronic illness group (69.7%) and the group without illnesses (26.7%).
3.4. Quality of Life
Table 4 shows various indicators of HRQoL including social relations, self-rated health, chronic activity limitations, self-rated HRQoL and sexual activity. Both the IHD group and the group with other illnesses had significantly poorer social relations than people without illness. The IHD group also rated their own health as significantly poorer than the two other groups and the groups with illness reported more activity limitations than the group without illness.
Figure 1 presents the SF-36 profiles for the three groups. The IHD group and the group with other illnesses had significantly poorer HRQoL on all subscales than the group without illness. The difference was most pronounced in the scales measuring physical health (Figure 1). The SF-12 physical component for the IHD group (41.8%); (95% CI: 33.6% - 50%) was significantly lower than the chronic illness group (45.3%); (95% CI 43.5% - 47.1%)) and the no disease group (54.0%); (95% CI: 2.4% - 55.5%) (p < 0.001) (Table 4). The mean SF- 12 mental component scores were also lower in the IHD group (49.0%); (95% CI 40.8 - 57.8)) compared to the chronic illness group (51.5%); (95% CI 49.7% - 53.3%) and other disease group (53.6%); (95% CI 52% - 55.1%) (p < 0.001). Figure 1 clearly shows that the HRQoL of people with IHD is lower than that of people with other illnesses.
Another indicator of HRQoL is sexual activity (Table 4). More people in the two illness groups reported reduced or unsatisfactory sexual activity, with the IHD group reporting the most reduced sexual function. Stratified analyses showed no differences between men and women.
4. DISCUSSION
A total of 5.6% (95% CI 5.2% - 6.0%) of the adult population in Denmark is living with IHD. People with self-reported IHD can be characterized as having poorer
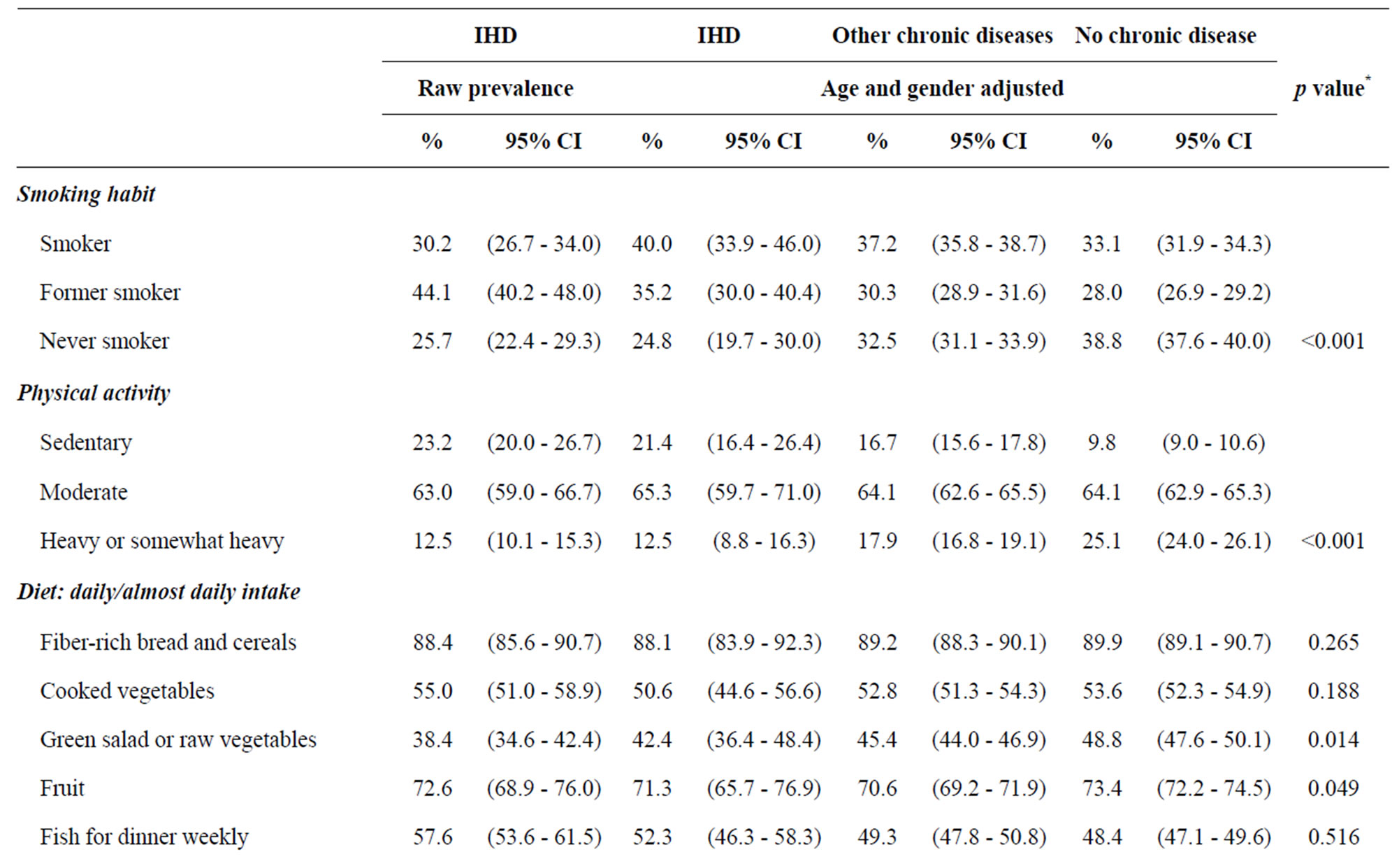
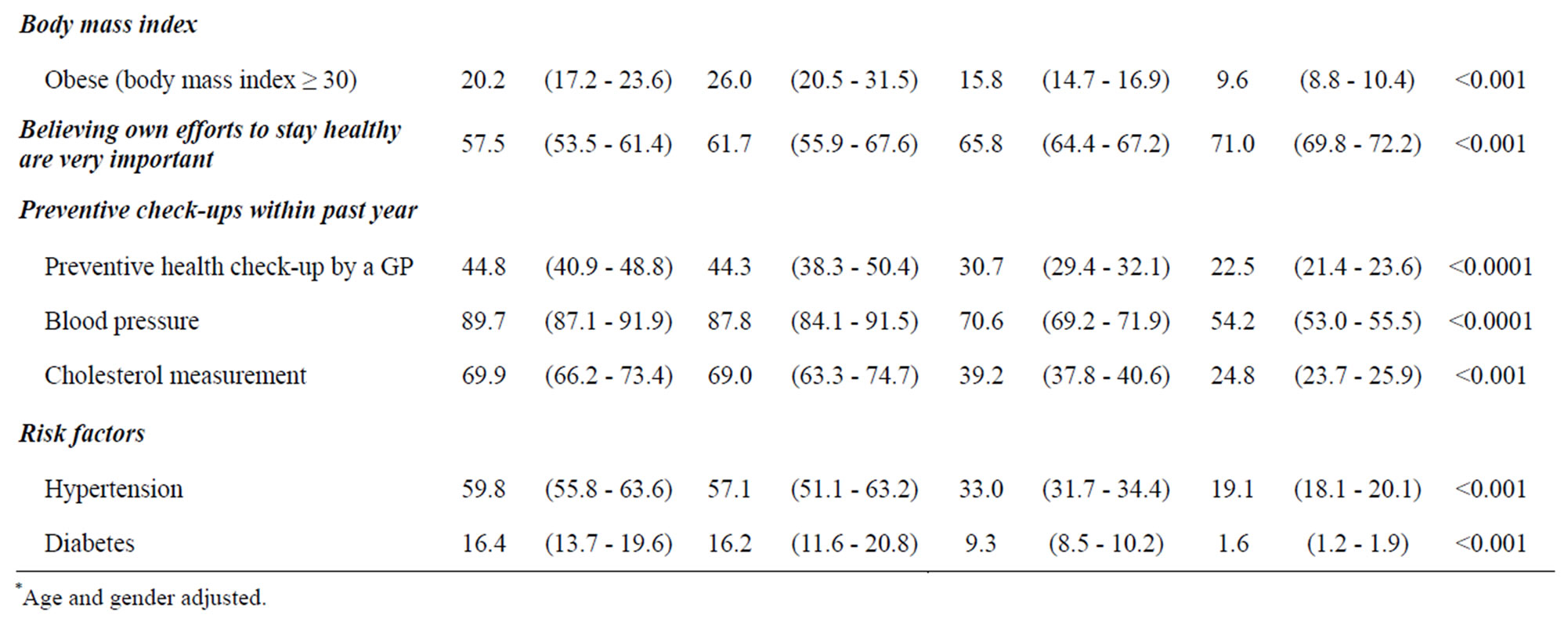
Table 2. Health behavior and risk factors among people with self-reported IHD, other chronic illness, and no chronic illness.
health behaviors, more risk factors, higher utilization of the health-care services, and poorer HRQoL. When compared to people with other chronic diseases, people with IHD continue to show the same characteristics.
4.1. Strengths and Weaknesses
The study is based on a representative survey of the adult Danish population aged 35 years or older. It is a large sample with an acceptable response rate of 67%, which minimizes non-respondent basis [17]. The survey includes a wealth of information on health and morbidity, making it possible to describe the health behaviors, lifestyle, HRQoL and health-care system utilization associated with people with IHD. This was a unique opportunity to investigate this population regardless of their use of the health-care system. Furthermore, the survey made it possible to compare the IHD group to a group with other chronic diseases.
The SUSY survey did rely on self-reported information that was collected during the interview and selfadministered questionnaire. In some cases lifestyle can
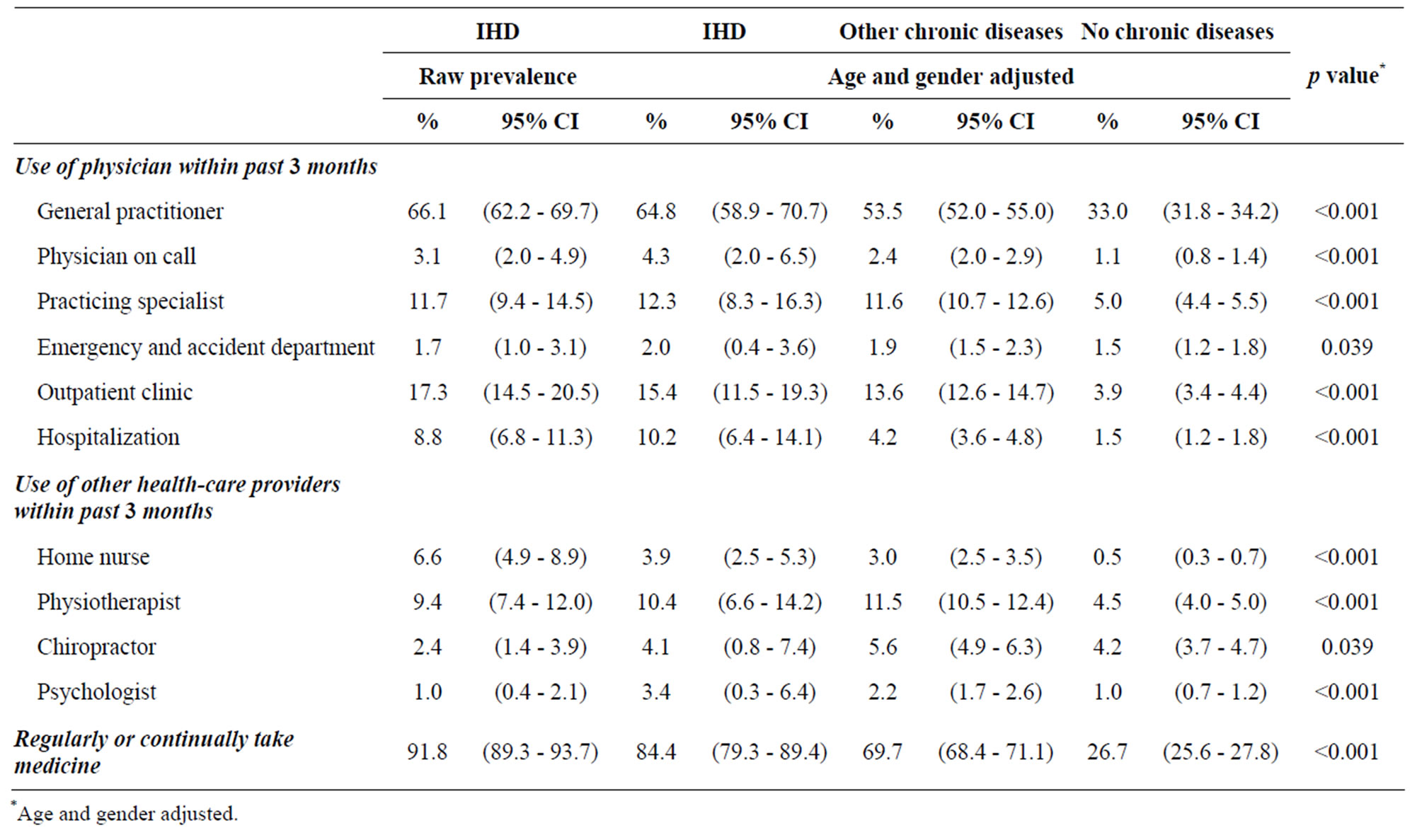
Table 3. Use of health-care services by people with self-reported ischemic heart disease, other chronic illness and no chronic illness.
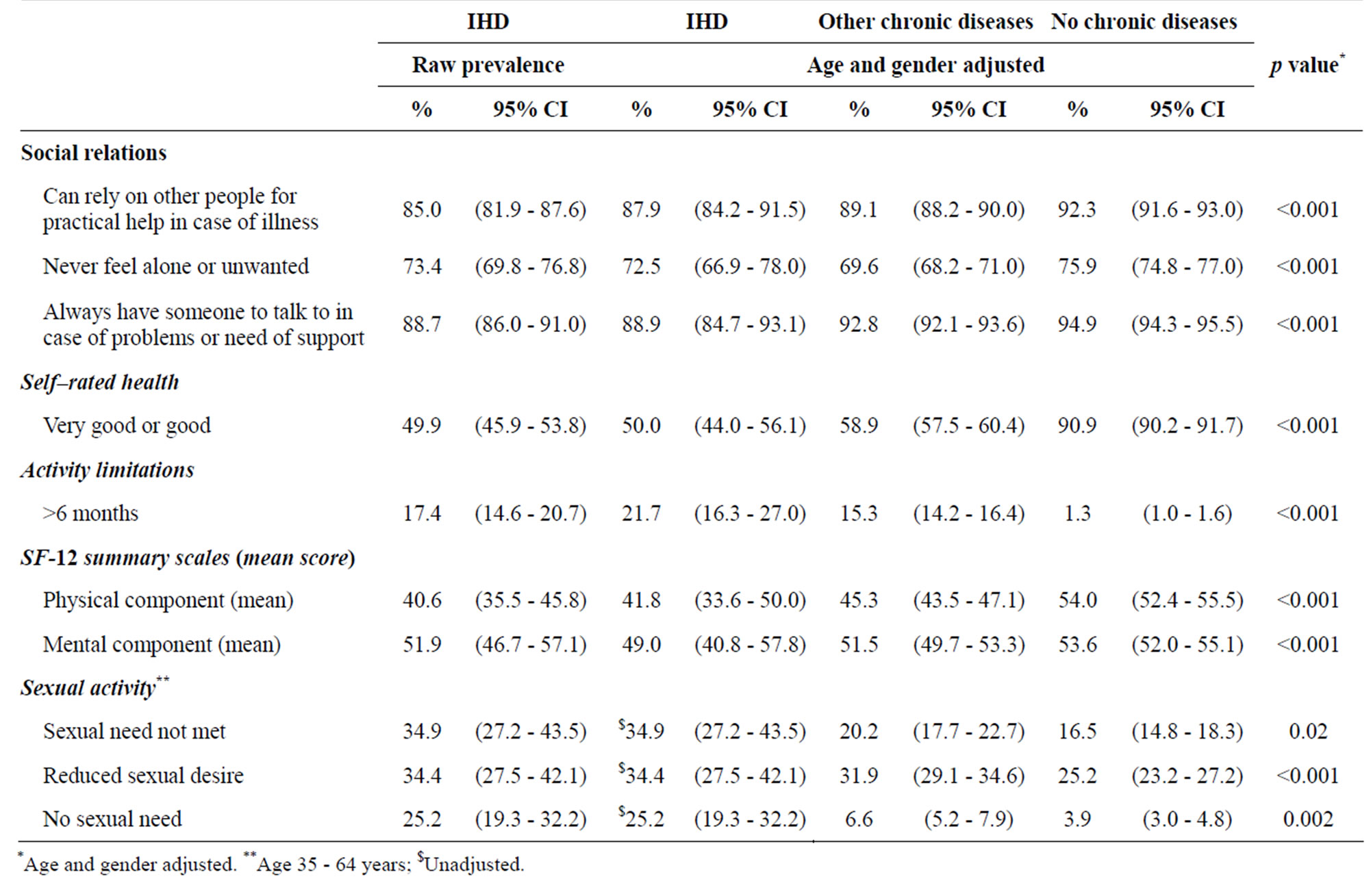
Table 4. Social relations and quality of life among people with self–reported ischemic heart disease, other chronic illnesses, and no chronic illness.
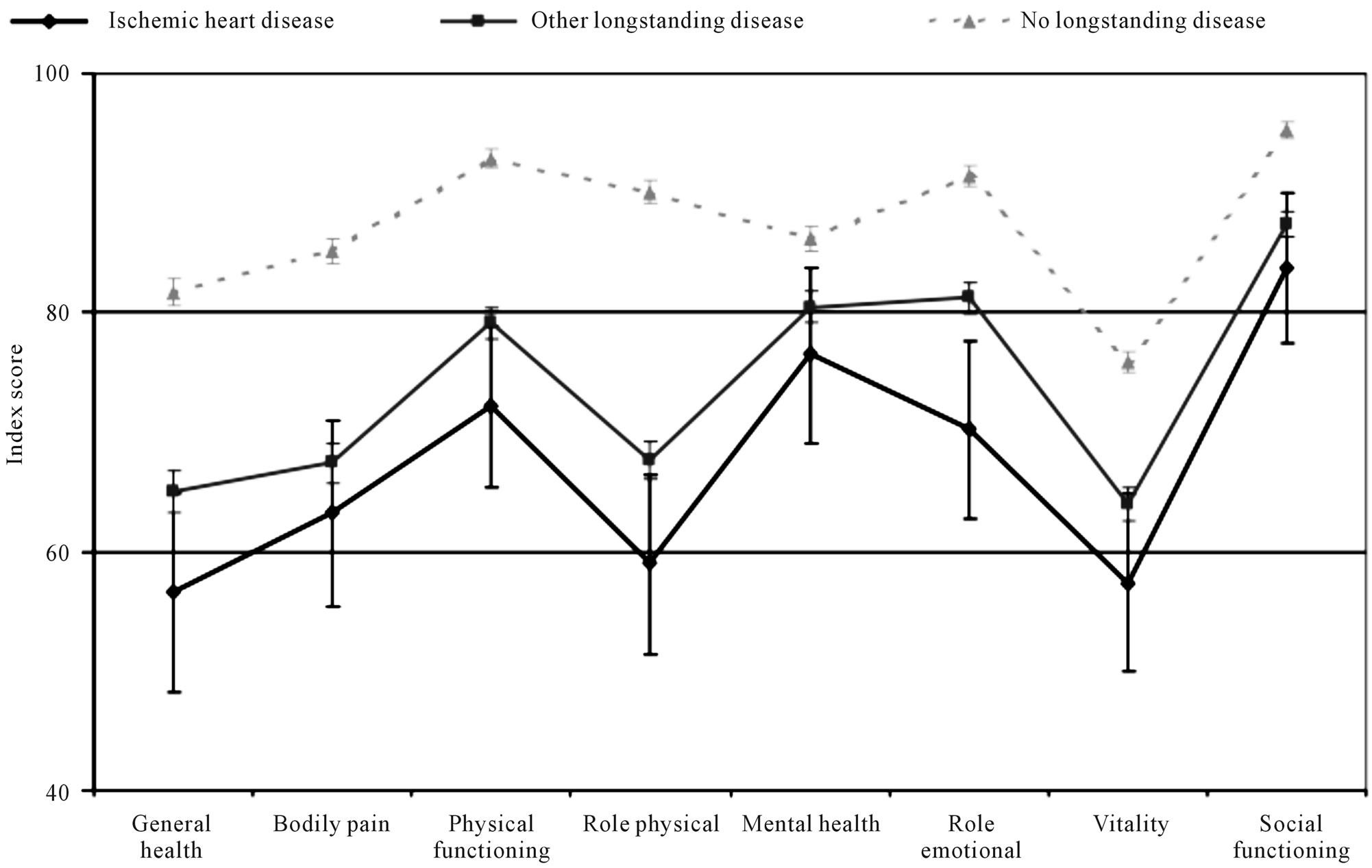
Figure 1. Health status measures by SF-36 score among people with ischemic heart disease, other chronic illness, and no chronic illness. Age and gender adjusted scores and 95% CI.
be underreported because respondents try to paint a positive picture [19]; however, self-reporting is the only way to collect subjective information about experiences, how people feel about their own health status and health knowledge level [17]. This kind of information makes important contributions to the overall description of the daily life of people with IHD because functionality and disability [17] related to IHD can be investigated. It also must be noted that the questions used for the survey were developed with a minimum manageable data set [17], therefore some health behaviors were measured using shorten validated tools. For example, the SF-36 [15] was used to measure HRQoL and a single question [13] was used to measure self-efficacy.
Another potential weakness is the misclassification of the IHD group. However, 96% of respondents reporting chronic illness also reported that a doctor established the diagnosis [6]. Following the respondents in the National Hospital Register, 36% of the IHD group, 1% of the other illness group and 2% of the group without illness had been hospitalized during a 5-year period. Therefore, if misclassification existed, it is estimated as minimal.
This study was also not able to account for the effect of multiple chronic conditions. It has been established that many older individuals have a combination of chronic diseases and that clinical research often overlooks individuals with multiple chronic illnesses [18]. This is an area of current research and understanding how chronic illnesses work in combination [18] can greatly impact the healthcare-system.
4.2. Clinical and Health-Care System Implications
From a health promotion and rehabilitation perspective it is important to note that the IHD group had more problems affecting their daily lives than the other two groups. The IHD group exhibited poorer health behaviors and more risk factors including: smoking, sedentary lifestyle, obesity, hypertension and diabetes. These cardiovascular disease risk factors have also been identified by previous research as modifiable risk factors, which means they can be controlled or even prevented [20].
The IHD group also had lower self-efficacy compared to the other two groups. Self-efficacy is an important prerequisite for changing health behavior and coping with chronic illness [14,21], including IHD [14]. Low cardiac self-efficacy has been linked to higher hospitalizations [14] and higher self-efficacy has been associated with better health status [12] and lifestyle modification compliance [14,22].
Higher utilization of the health-care system was also found in the IHD group. They attended more preventive health check-ups and had more contact with general practitioners and other health professionals than the other two groups. Furthermore, the IHD group reported taking significantly more regular medication, which required contact with health-care system. Higher utilization of the healthcare system can lead to higher economic cost for the health-care system and society. Previous research in Denmark estimated that people with heart disease cost 3,195 times more per person than people without heart disease [5]. It has also been reported that the cost of living an unhealthy lifestyle contributes 11% - 16% of the attributable cost of heart disease [5].
Likewise, there were a number of indicators for poorer HRQoL for the IHD group: poorer social relations, lower self-rated health, more physical limitations, lower selfrated HRQoL and reduced sexual function. Lower selfrated health [23] and poorer social relations [24,25] have been associated with higher morbidity and mortality for chronic disease. Chronic physical limitations also have a negative impact on people with IHD [7,8]. Lower selfrated HRQoL has been linked to mortality from IHD [26] . Reduced sexual frequency and satisfaction is commonly found in patients with IHD and it is an important factor of HRQoL for many patients [27,28].
All these issues contribute to the high burden that patients with IHD cost the health-care system and society [1,3,17]. The burden of disease includes the substantial loss of HRQoL, disability and lifelong dependence on the healthcare system and medications [17]. Additionally, the societal costs are not only related to health-care and social services, but are linked to illness benefits and retirement, impact on families and caregivers and loss of years of productive life [17].
To reduce the burden of IHD it has been recommended that timely and accurate diagnosis is made a high priority [29] and that investment is needed to strengthen health promotion and prevention interventions [1,3,17]. For patients already diagnosed with IHD, costeffective disease management is needed [30]. Outpatient exercise-based cardiac rehabilitation has been shown to reduce modifiable risk factors [7-9,30], increase physical function [9], improve psychological and social functioning [9] and enhance HRQoL [8,30]. Previous research also indicates that cardiac rehabilitation reduces hospitalizations [30]; all-cause mortality [8,30], and recurrent MI [30]. Thus, cardiac rehabilitation could be developed and promoted to meet the challenges of chronic IHD in the adult population.
5. ACKNOWLEDGEMENTS
This study was partly financed by Helsefonden. The authors would like to thank Mette Madsen who contributed to the protocol and data definitions.
REFERENCES
- Tunstall-Pedoe, H. (2005) Preventing chronic diseases. A vital investment: WHO global report. World Health Organization, Geneva, 200 p. http://www.who.int/chp/chronic_disease_report/en/
- Meetoo, D. (2008) Chronic diseases: The silent global epidemic. British Journal of Nursing, 17, 1320-1325.
- Abildstrom, S.Z., Rasmussen, S. and Madsen, M. (2002) Significant decline in case fatality after acute myocardial infarction in Denmark—A population-based study from 1994 to 2001. Scandinavian Cardiovascular Journal, 36, 287-291. doi:10.1080/140174302320774492
- Kruse, M., Davidsen, M., Madsen, M., Gyrd-Hansen, D. and Sorensen, J. (2008) Costs of heart disease and risk behavior: Implications for expenditure on prevention. Scandinavian Cardiovascular Journal, 36, 850-856. doi:10.1177/1403494808095955
- Ekholm, O., Hesse, U., Davidsen, M. and Kjøller, M. (2009) The study design and characteristics of the Danish national health interview surveys. Scandinavian Journal of Public Health, 37, 758-765. doi:10.1177/1403494809341095
- Oldridge, N.B. and Stump, T.E. (2004) Heart disease, comorbidity, and activity limitation in community-dwelling elderly. European Journal of Preventive Cardiology, 11, 427-434.
- Taylor, R.S., Brown, A., Ebrahim, S., Jolliffe, J., Noorani, H., Rees, K., et al. (2004) Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. The American Journal of Medicine, 116, 682-692. doi:10.1016/j.amjmed.2004.01.009
- Leon, A.S., Franklin, B.A., Costa, F., Balady, G.J., Berr, K.A., Stewart, K.J., et al. (2005) Cardiac rehabilitation and secondary prevention of coronary heart disease. Circulation, 111, 369-376. doi:10.1161/01.CIR.0000151788.08740.5C
- Dempster, M. and Donnelly, M. (2000) Measuring the health related quality of life of people with ischemic heart disease. Heart, 83, 641-644. doi:10.1136/heart.83.6.641
- Brown, N., Melville, M., Gray, D., Young, T., Munro, J., Skene, A.M., et al. (1999) Quality of life four years after acute myocardial infarction: Short form 36 scores compared with a normal population. Heart, 81, 352-358.
- National Institute of Public Health (2006) Danish health interview survey 2005: Questionnaire for personal interviews with response frequencies. National Institute of Public Health, University of Southern Denmark, Copenhagen. http://www.niph.dk/upload/2005_questionnaire_for_personal_interviews_with_response_frequencies.pdf
- National Institute of Public Health (2006) Danish health interview survey 2005: Self administered questionnaire 1. National Institute of Public Health, University of Southern Denmark, Copenhagen. http://www.niph.dk/upload/2005_self-administrated_questionnaire_i.pdf
- Sarkar, U., Ali, S. and Whooley, M.A. (2009) Self-efficacy as a marker of cardiac function and predictor of heart failure hospitalization and mortality in patients with stable coronary heart disease: Findings from the Heart and Soul Study. Health Psychology, 28, 166-173. doi:10.1037/a0013146
- Bjorner, J.B., Thunedborg, K., Kristensen, T.S., Modvig, J. and Bech, P. (1998) The Danish SF-36 health survey: Translation and preliminary validity studies. Journal of Clinical Epidemiology, 51, 991-999. doi:10.1016/S0895-4356(98)00091-2
- McHorney, C.A., Ware, J.E. Jr., Lu, J.F. and Sherbourne, C.D. (1994) The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care, 32, 40-66. doi:10.1097/00005650-199401000-00004
- Whittaker, J. (2008) Graphical models in applied multivariate statistics. John Wiley and Sons Ltd., West Sussex,
- Primatesta, P., Allender, S., Ciccarelli, P., Doring, A., GraffIversen, S., Holub, J., et al. (2007) Cardiovascular surveys: Manual of operations. European Journal of Preventive Cardiology, 14, S43-S61. doi:10.1097/01.hjr.0000277988.18096.3b
- Vogeli, C., Shields, A.E., Lee, T.A., Gibson, T.B., Marder, W.D., Weiss, K.B., et al. (2007) Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. Journal of General Internal Medicine, 22, 391-395. doi:10.1007/s11606-007-0322-1
- Rasmussen, L.B., Matthiessen, J., Biltoft-Jensen, A. and Tetens, I. (2007) Characteristics of misreporters of dietary intake and physical activity. Public Health Nutrition, 10, 230-237. doi:10.1017/S136898000724666X
- Yusuf, S., Hawken, S., Ounpuu, S., Dans, T., Avezum, A., Lanas. F., et al. (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet, 364, 937-952. doi:10.1016/S0140-6736(04)17018-9
- Lorig, K.R. and Holman, H. (2003) Self-management education: history, definition, outcomes, and mechanisms. Annals of Behavioral Medicine, 26, 1-7. doi:10.1207/S15324796ABM2601_01
- Lau-Walker, M. (2007) Importance of illness beliefs and self-efficacy for patients with coronary heart disease. Journal of Advanced Nursing, 60, 187-198. doi:10.1111/j.1365-2648.2007.04398.x
- Idler, E.L. and Benyamini, Y. (1997) Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21-37. doi:10.2307/2955359
- Due, P., Holstein, B., Lund, R., Modvig, J. and Avlund, K. (1999) Social relations: Network, support and relational strain. Social Science & Medicine, 48, 661-673. doi:10.1016/S0277-9536(98)00381-5
- Berkman, L.F. (1995) The role of social relations in health promotion. Psychosomatic Medicine, 57, 245-254.
- Alonso, J., Ferrer, M., Gandek, B., Ware, J.E. Jr., Aaronson, N.K., Mosconi, P., et al. (2004) Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Quality of Life Research, 13, 283-298. doi:10.1023/B:QURE.0000018472.46236.05
- Klein, R., Baron, E., Klein, J. and Benbenishty, R. (2007) The impact of sexual therapy on patients after cardiac events participating in a cardiac rehabilitation program. European Journal of Cardiovascular Prevention & Rehabilitation, 14, 672-678. doi:10.1097/HJR.0b013e3282eea52d
- Drory, Y., Kravetz, S. and Weingarten, M. (2000) Comparison of sexual activity of women and men after a first acute myocardial infarction. American Journal of Cardiology, 85, 1283-1287. doi:10.1016/S0002-9149(00)00756-6
- Cassar, A., Holmes, D.R. Jr., Rihal, C.S. and Gersh, B.J. (2009) Chronic coronary artery disease: diagnosis and management. Mayo Clinic Proceedings, 84, 1130-1146. doi:10.4065/mcp.2009.0391
- Wenger, N.K. (2008) Current status of cardiac rehabilitation. Journal of the American College of Cardiology, 51, 1619-1631. doi:10.1016/j.jacc.2008.01.030

