R. S. ELUMALAI ET AL.
6
(a)
(b)
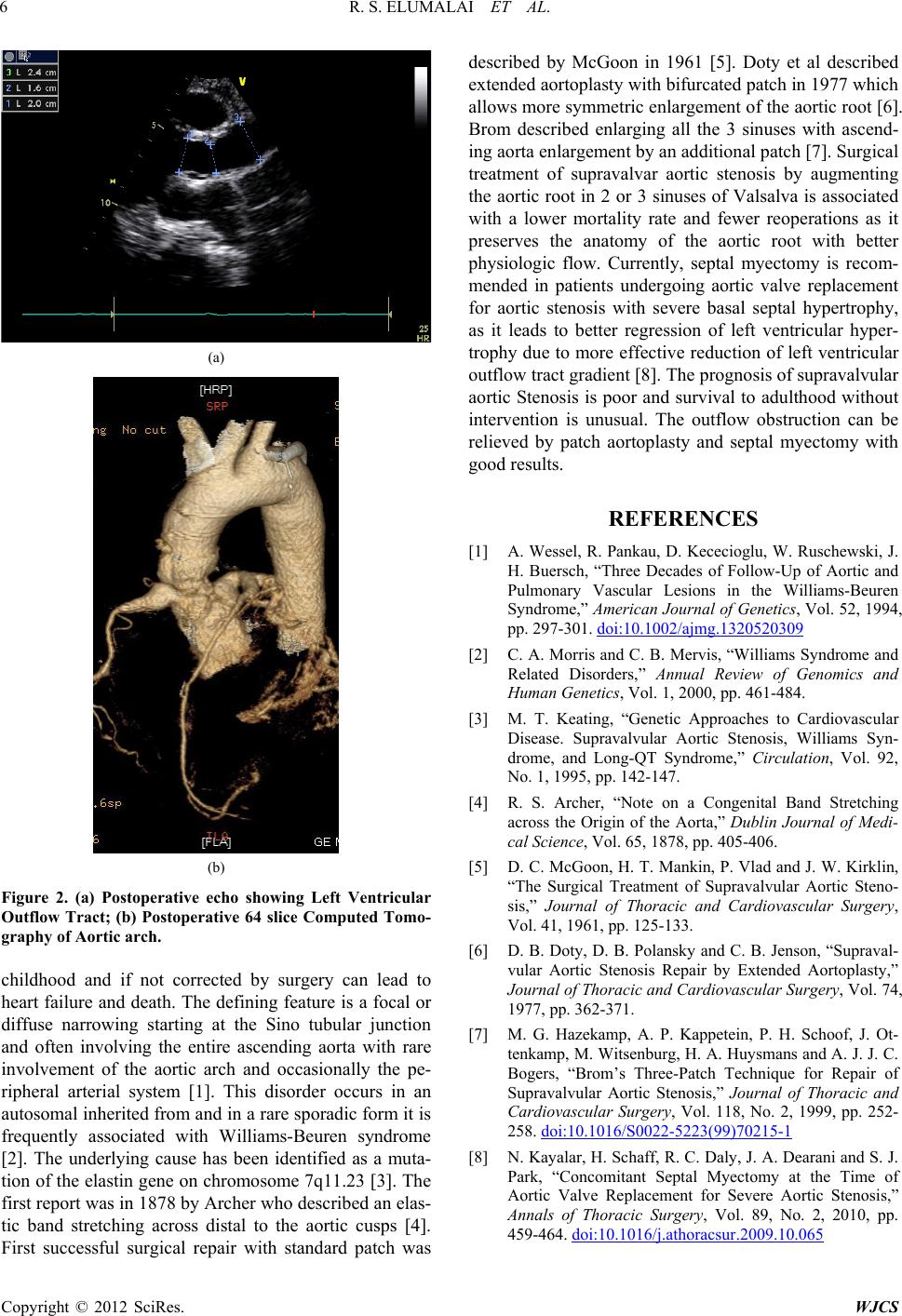
Figure 2. (a) Postoperative echo showing Left Ventricular
Outflow Tract; (b) Postoperative 64 slice Computed Tomo-
graphy of Aortic arch.
childhood and if not corrected by surgery can lead to
heart failure and death. The defining feature is a focal or
diffuse narrowing starting at the Sino tubular junction
and often involving the entire ascending aorta with rare
involvement of the aortic arch and occasionally the pe-
ripheral arterial system [1]. This disorder occurs in an
autosomal inherited from and in a rare sporadic form it is
frequently associated with Williams-Beuren syndrome
[2]. The underlying cause has been identified as a muta-
tion of the elastin gene on chromosome 7q11.23 [3]. The
first repor t was in 187 8 b y Arch er w ho d e scribe d an elas-
tic band stretching across distal to the aortic cusps [4].
irst successful surgical repair with standard patch was
described by McGoon in 1961 [5]. Doty et al described
extended aortoplasty w ith bifur cated patch in 1977 which
allows more symmetric enlargement of the ao rtic root [6].
Brom described enlarging all the 3 sinuses with ascend-
ing aorta enlarg ement by an additional patch [7]. Surgical
treatment of supravalvar aortic stenosis by augmenting
the aortic root in 2 or 3 sinuses of Valsalva is associated
with a lower mortality rate and fewer reoperations as it
preserves the anatomy of the aortic root with better
physiologic flow. Currently, septal myectomy is recom-
mended in patients undergoing aortic valve replacement
for aortic stenosis with severe basal septal hypertrophy,
as it leads to better regression of left ventricular hyper-
trophy due to more effective reduction of left ventricular
outflow tract gradien t [8]. The p rogno sis of suprav alvular
aortic Stenosis is poor and survival to adulthood without
intervention is unusual. The outflow obstruction can be
relieved by patch aortoplasty and septal myectomy with
good results.
F
REFERENCES
[1] A. Wessel, R. Pankau, D. Kececioglu, W. Ruschewski, J.
H. Buersch, “Three Decades of Follow-Up of Aortic and
Pulmonary Vascular Lesions in the Williams-Beuren
Syndrome,” American Journal of Genetics, Vol. 52, 1994,
pp. 297-301. doi:10.1002/ajmg.1320520309
[2] C. A. Morris and C. B. Mervis, “Williams Syndrome and
Related Disorders,” Annual Review of Genomics and
Human Genetics, Vol. 1, 2000, pp. 461-484.
[3] M. T. Keating, “Genetic Approaches to Cardiovascular
Disease. Supravalvular Aortic Stenosis, Williams Syn-
drome, and Long-QT Syndrome,” Circulation, Vol. 92,
No. 1, 1995, pp. 142-147.
[4] R. S. Archer, “Note on a Congenital Band Stretching
across the Origin of the Aorta,” Dublin Journal of Medi-
cal Science, Vol. 65, 1878, pp. 405-406.
[5] D. C. McGoon, H. T. Mankin, P. Vlad and J. W. Kirklin,
“The Surgical Treatment of Supravalvular Aortic Steno-
sis,” Journal of Thoracic and Cardiovascular Surgery,
Vol. 41, 1961, pp. 125-133.
[6] D. B. Doty, D. B. Polansky and C. B. Jenson, “Supraval-
vular Aortic Stenosis Repair by Extended Aortoplasty,”
Journal of Thoracic and Cardiovascular Surgery, Vol. 74,
1977, pp. 362-371.
[7] M. G. Hazekamp, A. P. Kappetein, P. H. Schoof, J. Ot-
tenkamp, M. Witsenburg, H. A. Huysmans and A. J. J. C.
Bogers, “Brom’s Three-Patch Technique for Repair of
Supravalvular Aortic Stenosis,” Journal of Thoracic and
Cardiovascular Surgery, Vol. 118, No. 2, 1999, pp. 252-
258. doi:10.1016/S0022-5223(99)70215-1
[8] N. Kayalar, H. Schaff, R. C. Daly, J. A. Dearani and S. J.
Park, “Concomitant Septal Myectomy at the Time of
Aortic Valve Replacement for Severe Aortic Stenosis,”
Annals of Thoracic Surgery, Vol. 89, No. 2, 2010, pp.
459-464. doi:10.1016/j.athoracsur.2009.10.065
Copyright © 2012 SciRes. WJCS