Open Journal of Stomatology
Vol. 2 No. 4 (2012) , Article ID: 25553 , 8 pages DOI:10.4236/ojst.2012.24058
99mTc in the evaluation of microleakage of compositeresin restorations with SonicFillTM. An in vitro experimental model*
![]()
Faculty of Medicine, University of Coimbra, Coimbra, Portugal
Email: eunicecarrilho@netcabo.pt
Received 5 October 2012; revised 5 November 2012; accepted 23 November 2012
Keywords: Posterior resin Composites; Composite Restorations; Polymerization Stress; Polymerization Shrinkage; Microleakage; Thermocycling
ABSTRACT
Introduction: The composite SonicFillTM (Kerr/Kavo) is indicated for posterior restorations, with a single increment up to 5 mm due to reduced polymerization shrinkage, thus reducing working time. Aim: Evaluation of marginal microleakage with SonicFillTM. Method and Materials: There were sectioned sixty noncarious human molars in the occluso-cervical direction. Class V cavities were prepared on each tooth with gingival margin walls in a standardized way. The specimens were divided into 4 groups: group 1—restored with SonicFillTM (Kerr/Kavo), group 2—restored with FiltekTM SupremeXTE (3M ESPE), group 3—the cavities were not restored; group 4—restored with SonicFillTM (Kerr/Kavo). In groups 1, 2 and 4 the enamel was conditioned with 37% orthophosphoric acid and applied the self-etch adhesive system ClearfillTM SE BOND (Kuraray). The specimens were stored in distilled water at 37˚C for 7 days. After, the specimens, were immersed in a solution of 99mTcPertechnetate and the radioactivity was assessed with a gamma camera. The nonparametric Kruskal-Wallis and Mann-Whitney test with Bonferroni correction at a significance level of 5% were used for the statistical analyses. Results: There are significant differences between the positive and negative control groups and between these and experimental groups (p < 0.05). There are no statistically significant differences between the specimens restored with SonicFillTM and FiltekTM SupremeXTE. Conclusion: The new composite SonicFillTM and FiltekTM SupremeXTE showed no difference concerning dye penetration. The SonicFillTM restorative system showed no influence in concerning microleakage.
1. INTRODUCTION
Amalgam was for years the most often used restorative material by dentists. Due to aesthetic reasons, environmental and questionable biocompatibility of alloys that contain mercury, practitioners needed to seek a new material that would satisfy these needs. Resin composites, introduced in the 1960s [1,2], satisfied aesthetic needs, and nowadays they represent a class of materials widely used in restorative dentistry [3].
Resin composites should fulfil a lot of basic requirements: good optical characteristics; the physical properties should correspond to those of dental hard tissue in terms of wear resistance; they should be distinguishable from dental tissue on x-ray; easy to handle and polish; they should be tasteless and biocompatible and should form a sufficient bond with dental tissue or at least with the dental adhesive [4]. However, many clinical and material limitations have restricted the universal use of resin composites as posterior restorative material [1].
Despite having good physical properties, the main shortcomings of composite resin materials are polymerization shrinkage [1-8] and polymerization stress [5]— shrinkage stress resulting in internal microcracks within the bulk of the material [7]; separation of the bonding agent from the cavity wall with resultant gap formation, marginal microleakage and post-operative sensitivity [1, 3,7-9]; enamel microcracks [5,7]; marginal staining [8]; wear [9]; discoloration [9]; lower fracture resistance [1,5, 9]; recurrent caries [1,3,8,9]; and deformation of tooth [5,7].
Microleakage is the clinically undetectable passage of bacteria, fluids, molecules and ions between the cavity wall and the restorative material [1,10,11] and is considered to be a major factor influencing the longevity of dental restorations [1]. The decrease of the polymerization shrinkage and consequent microleakage, can be obtained by an oblique layering technique with increments or design cavities with a low C-factor [1,6]. On the other hand, some changes in restorative materials, made in the past, like improvements in the filler technology and formulation of composite materials, have improved performance of the resins [8,9,12].
A novel resin composite system, SonicFill™ System (Kerr/Kavo), was recently introduced in the market. Is indicated for use as a bulk fill posterior composite restorations and can be bulk filled in layers up to 5 mm in depth due to reduced polymerization shrinkage. SonicFillTM incorporates a highly-filled proprietary resin with special modifiers that react to sonic energy. As sonic energy is applied through the hand piece, the modifier causes the viscosity to drop (up to 87%), increasing the flow ability of the composite enabling quick placement and precise adaptation to the cavity walls. When the sonic energy is stopped, the composite returns to a more viscous, non-slumping state that is perfect for carving and contouring [13].
One of the objective methods for microleakage rating is the use of radioactive isotopes. Technetium is an artificial element, obtained by the radioactive decay molibdenium, which is a radioactive metallic element belonging to the transition metals with an atomic radius of 135.8 pm. It is element 43 of the periodic table, and the radioactive element with the lowest atomic number. This presents a half-life of 2.6 hours. Its decay occurs by the isometric transition and emission and 140.5 keV of gamma radiation [14].
The purpose of the present study is to evaluate the microleakage of the dental restorations with SonicFillTM System (Kerr/Kavo). The null hypothesis is that the type restorative system has no influence concerning microleakage.
2. METHOD AND MATERIALS
Thirty noncarious extracted human molars were hand scaled and stored in normal saline solution 0.9% (B. Braun, 11496403, Queluz de Baixo, Barcarena) at 5˚C no more than 4 months after extraction. The teeth were cut with a Exakt System 300 saw (Exakt System, 22851 Norderstedt, Germany) in two equal halves occluso gingivally. Class V cavities were prepared on the buccal surface of each tooth. The cavity had dimensions of approximately 4 mm mesiodistally, 3 mm occluso gingivally and 3 mm in depth. An internal line angle of 90 degrees was maintained to create occlusal and gingival margins walls of approximately 2 mm. Both margins were located in enamel. A transparent resin mold was performed to design the cavities in each tooth surface (Figure 1). The burs FG 835/010 (Proclinic, 34/09, Nyon, Swiss) were replaced after every 5 preparations.
The specimens were divided randomly in each group. Forty specimens were used for the study group and twenty specimens for each control group.
Group 1: a SonicFillTM System (Kerr/Kavo, 3691651, Bismarckring, Biberach) activated, bulk fill composite shade (A2) was used to restore the class V cavities of 20 specimens. The enamel was conditioned for 30 seconds with 35% phosphoric acid gel Octacid Jumbo (Clarben, T012RD, Lindigo, Sweden), washed immediately after with an air/water jet for 30 seconds. A self-etch bond agent, ClearfilTM SE BOND (Kuraray, 041872, Okayama, Japan) was used according to manufacturer’s instructions. ClearfilTM SE BOND primer was applied to the enamel/- dentin using a scrubbing motion and dried thoroughly with mild air flow before being light cured for 20 seconds using light cure Blue PhaseTM G2 (Ivoclar Vivadent, 5VDC, Liechtenstein, Austria), ClearfilTM SE BOND bond was applied to the enamel/dentin surface using a light brushing motion, dried with gentle air flow and light cured for 10 seconds using light cure BluePhaseTM G2. The Sonic Fill™ was placed in one bulk increment followed by shaping the buccal surface and light curing for 20 seconds using light cure BluePhaseTM G2 (Ivoclar Vivadent, 5VDC, Liechtenstein, Austria). Restorations were polished using Sof-Lex Disk System (Brown/ Orange/Light Orange/Yellow, 3M ESPE, N301289, St. Paul, MN, USA).
Group 2: a FiltekTM SupremeXTE (3M ESPE, N339166, St. Paul, MN, USA) shade A2 was used to restore the class V cavities of 20 specimens. The enamel was conditioned in the same way as described for group 1. A self-etch bond agent, ClearfilTM SE BOND (Kuraray, 041872, Okayama, Japan) was applied following the use pattern in group 1. Restorations were polished using the same disk system.
Group 3: the class V cavities of 10 specimens were not restored.

Figure 1. Cavity preparation to receive the resin composite.
Group 4: a SonicFillTM System (Kerr/Kavo, 3691651, Bismarckring, Biberach) activated, bulk fill composite shade (A2) was used to restore the class V cavities of 10 specimens. The enamel was conditioned in the same way as described for group 1 and 2. A self-etch bond agent, ClearfilTM SE BOND (Kuraray, 041872, Okayama, Japan) was applied following the use pattern in group 1 and group 2. Restorations were polished using the same disk system.
There was only one operator performing all restorative procedures. The specimens were stored in distilled water at 37˚C for one week and then went through thermocycling 500 cycles between 5˚C and 55˚C with a dwell time of 30 seconds, and no further treatment. The specimens of groups 1, 2 and 3 were covered with two layers of red nail varnish (Resist and Shine L’Oréal, 16G901, Paris, France) up to 2 mm from the margins around the restorations. The specimens of group 4 were covered over the entire surface. The specimens of all groups were immersed in 99mTc-Pertechnetate solution for 3 hours. Afterwards the varnish was removed. The radioactivity issued by the specimens was detected by the gamma camera (Figure 2). The statistical analysis was performed using the program SPSS 19. Comparisons were made using the nonparametric Kruskal-Wallis test and multiple comparisons were made using the Mann-Whitney test with Bonferroni correction. A significance level of 5% was considered.
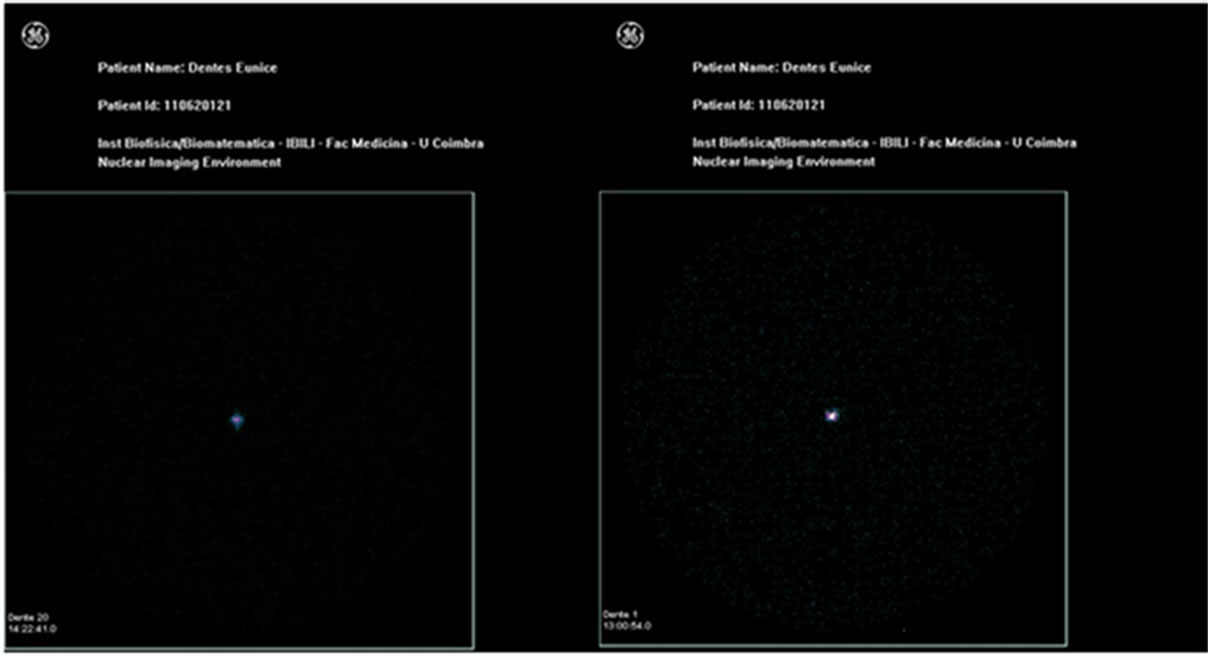
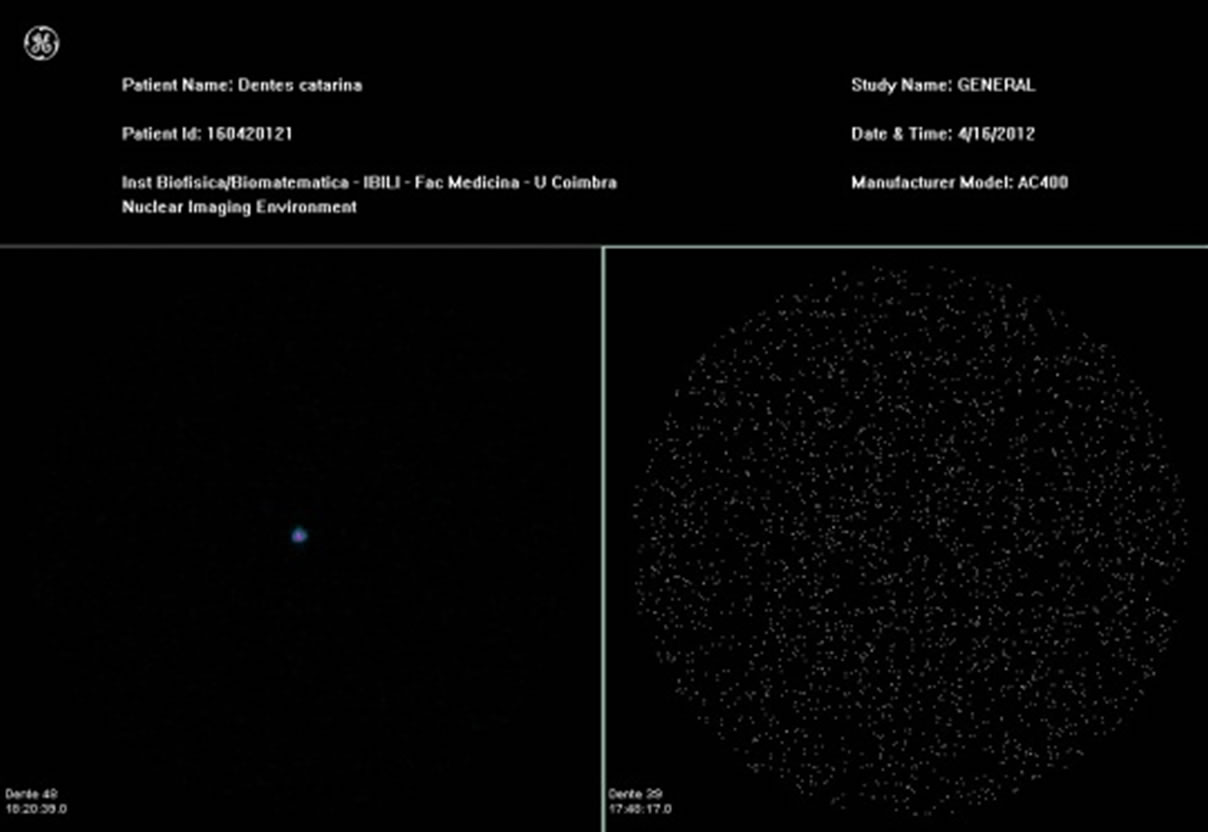
Figure 2. Nuclear medicine static image, obtained in the Gamma-camera GE 400 Ac, 3 hours after teeth infiltration with 99mTc for the groups 1, 2, 3 and 4.
3. RESULTS
In this study, 60 specimens were used, assigned to group 1 (n = 20), group 2 (n = 20) and positive control groups (n = 10) and negative (n = 10). After acquiring the values of the average counts of each tooth, multiple group comparison was performed using the nonparametric Kruskal-Wallis test, since, although there was a normal distribution of the values obtained, there was no homogeneity of variances necessary to apply the ANOVA test. A Mann-Whitney test with Bonferroni correction was used to calculate p value between different test groups. We established the level of Statistical Significance at p < 0.05. If p < 0.05, it indicates significant difference. If p < 0.001, it Indicates highly significant difference among groups.
Data analysis showed that there were statistically significant differences between experimental groups and control groups (p < 0.05) in accordance with that shown in Table 1. Apart from these differences, highly significant difference was observed between negative and positive control groups (p < 0.001), as shown in Table 1. In the positive control group there was a large microleakage, and the negative control group received minimum counts, as shown in Table 2.
Regarding the comparison of scores obtained from groups 1 and 2, according to Table 3, a significant statistical difference was not observed (p < 0.05).
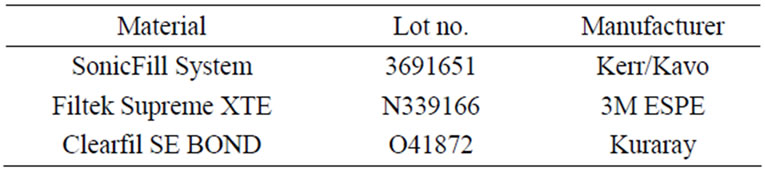
Table 1. Materials used in the study.
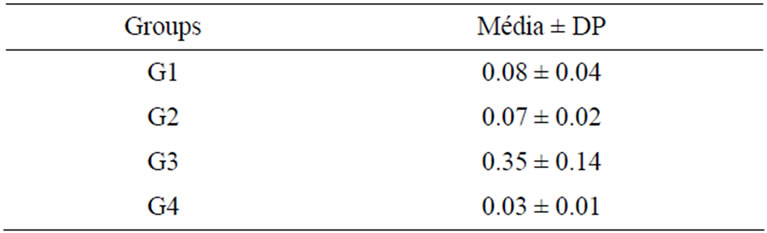
Table 2. Means and standard deviation of the microleakage in the experimental and control groups.
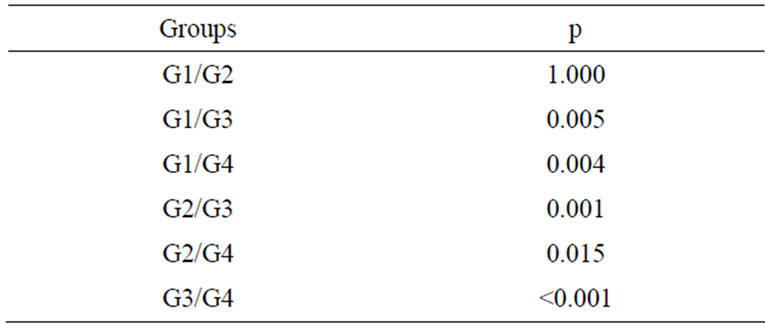
Table 3. Statistical comparison according to the Mann-Whitney test with Bonferroni correction.
4. DISCUSSION
Aesthetic considerations are playing a greater role in the treatment planning of dental care, even in the restoration of posterior teeth, stimulated by the popularity of aesthetics, patient demands for nonmetallic restorations and the controversy about the systemic and environmental effects of dental amalgam. These facts have stimulated the development of adhesive dentistry.
Resin composites can be used for different purposes such as: restoring the function and aesthetics of dental hard tissue lost due to caries or trauma, correct malposition/malocclusion or gaps, repair restorations, building up fractured teeth and creating stump build-ups for prosthetic reconstruction, cement indirect restorations, bond orthodontic appliances and seal fissures [15].
They are a combination of inorganic particles, organic resinous matrix and coupling agents. The inorganic particles are made of quartz, ceramic and silica [4] and they provide material strengthening and reinforcement [3]. Diverse types, shapes, sizes, volume fractions, and distributions of filler particles affect the material’s properties, such as hardness, thermal stability, radio-opacity, gloss retention and roughness, water sorption, viscoelastic creep and recovery, fracture toughness, fracture behaviour and, elastic moduli [3]. Properties like water sorption, the linear expansion coefficient and polymerization shrinkage decrease with increased filler content, whereas, the compressive and tensile strength, the modulus of elasticity and wear resistance rises with increased filler content [4]. The resin matrix consists of organic monomers, photo initiators, co-initiators, polymerization inhibitors, UV-stabilizers and small amounts of additional components that vary according the manufacturer [3]. The monomer, which is present in larger amounts, in the resin matrix is Bis-GMA (bisphenol-A-glycidyldimethacrylate) [3,4]. This monomer makes the resin viscosity very high, so it is mixed in different combinations with short-chain monomers such as TEGDMA (triethylenglycol-dimethacrylate) [3,4]. However, as negative effects, the addition of TEGDMA to the resin formulation increases water sorption [3] and polymerization shrinkage [3,4]. Furthermore, it increases the tensile but reduces the flexural strength of the resin [4]. There are other monomers that have also been used and tested [3]. The coupling agents are used to bond the inorganic filler with the organic matrix, since these do have chemical affinity. The common agent is y-MPTS (y-methacryloxypropyl-triethoxysilane [3]. Silanisation of the filler is important for material strength [4].
The integrity of the marginal seal is essential to increase the longevity of the restoration [16]. That integrityis compromised when microleakage occurs resulting from polymerization shrinkage. As previously mentioned, polymerization shrinkage is the most common cause of failure of direct posterior composite restorations. Polymerization shrinkage is a very complex phenomenon dependent upon the boundary conditions, the amount of material in the polymerization reaction and the material’s formulation [3]. This phenomenon occurs because monomer molecules are converted into a polymer network and, therefore, exchange Van der Walls spaces into covalent bond spaces, creating contraction stresses in the resin composite leading to microleakage [1]. It divides into two phases: pre-gel-polymerization, in which the composite is able to flow and stress within the structure is relieved, and after gelation, flow ceases and cannot compensate the stress; and post-gel polymerization, causing significant stress in the surrounding tooth structure and composite-tooth bond [6].
Different resin composites have different formulations and consequently different polymerization shrinkage. Many studies have suggested the use of an incremental layering technique to reduce this shrinkage [1,3,17]. Nowadays, traditional placement techniques for composite resins include this technique [3]. Most practitioners recommend placing composites in 2 mm increments. However, every dentist who places posterior composite resins needs a composite material that can be used using a bulk fill technique similar to that of dental amalgam.
The magnitude of the stress depends upon other factors, such as the configuration factor (C-factor) of the cavity and also the effect of light-curing mode. In our study the cavities were the same dimensions, the same C-factor, and the light-curing mode was the same for all the restoration specimens [18].
In this study we used two resin composites: a conventional one, FiltekTM SupremeXTE, and a bulk fill activated system, SonicFillTM. FiltekTM SupremeXTE is a nanocomposite that contains nanometric particles and nanoclusters, and presents high translucency, high polish and polish retention similar to microfilled composites and physical properties and wear resistance equivalent to several hybrid composites [19]. SonicFillTM was introduced in the dental market in 2010 and it combines the properties of a flow able composite with those of a universal composite: oscillation energy temporarily increases flow ability of the composite to achieve precise filling of cavities. An advantage of this composite is the rapid placement through a single increment up to 5 mm due to reduced polymerization shrinkage, thereby reducing working time [13].
The aim of this study was to evaluate the microleakage of the dental restorations with SonicFillTM, compared with a universal composite.
Thirty noncarious extracted human molars were selected. Despite all the teeth being molars, they present differences in respect of their length, diameter and anatomy. However, with the random division of the teeth into the four groups it was expected that a fair comparison between the different groups would be obtained. Class V cavities were prepared on the buccal/palatal surface of each tooth with cavity dimensions approximately 4 mm mesiodistally, 3 mm occlusogingivally and 3 mm in depth [20].
The success of composite restorations depends on the adhesion of restorative materials to hard tooth tissue. The dental adhesives have different tooth-composite interface morphologies, different bond strengths and different abilities in microleakage prevention [21]. To promote adhesion of the composite to enamel and dentina two-step self-etch adhesive was chosen, ClearfilTM SE BOND. Self-etch adhesive systems promote the dissolution of the inorganic phase of dentin using acidic monomer, with simultaneous infiltration of adhesive monomer around the collagen network that results in fewer exposed collagen fibrils [22]. According to Yuasa et al. these adhesive systems have the advantage of saving time, reducing procedural errors and with their lower etching ability, decreasing the potential for iatrogenic damage to dental hard tissue [23]. De Goes et al. advocate that ClearfilTM SE BOND presents significantly higher bond strengths than other self-etching adhesives [24]. The enamel was etched previously with 35% phosphoric acid gel, increasing the bond strengths significantly [25].
Posteriorly, cavities in group 1 and group 4 were restored with a single increment of SonicFillTM, as recommended by the manufacturer; and cavities in group 3 were restored with FiltekTM SupremeXTE using the incremental technique, recommended by several authors. [3,26,27] According to Schneider et al. [3], Park et al. [26] and Lee et al. [27] the use of an incremental filling technique reduces the cuspal deflection resultant from polymerization shrinkage. Nevertheless the literature is not conclusive concerning the advantages promoted by the incremental technique. Versluis et al. [28] and Loguercio et al. [29] argue that the incremental filling technique produces higher polymerization stresses at the restoration interface compared with bulk fill. In this study it was found that the polymerization shrinkageis similar in both methods, since there was no statistically significant difference as regards microleakage with SonicFillTM and FiltekTM SupremeXTE.
The same operator performed all restorative procedures, to reduce human operator error, as some authors have recommended [10,17,20,30]. The specimens were stored in distilled water at 37˚C for one week [2,14] and after thermocycling 500 cycles between 5˚C and 55˚C with a dwell time of 30 seconds [10,22,29,31]. Composite restorations are exposed to various influences in the oral cavity, and therefore to evaluate microleakage methods to reproduce these features are required. Storage in water is the most common artificial ageing technique, as mentioned by Amaral et al. and Yuasa et al. [22,23] Another widely used method is thermocycling [11,23,30]. For Geerts et al. thermocycling is the only in vitro test for stimulating thermal stress in teeth [32]. Thermocycling, according Helvatjoglu-Antoniades et al., simulates the introduction of hot and cold extremes in the oral cavity and shows the relationship of the linear coefficient of thermal expansion between tooth tissues and restorative materials [6]. For Souza et al. thermocycling is a combination of hydrolytic and thermal degradation that simulates the temperature of the oral cavity through sudden changes in temperature [33]. Thermocycling regimens vary between studies with respect to the number of cycles, temperature and dwell time. The International Organization for Standardization (ISO) TR 11450 standard (1994) indicates a thermocycling regimen comprising 500 cycles in water between 5˚C and 55˚C [10,23,31,34]. However, some authors report that this number of cycles is probably too low to achieve a realistic ageing effect [22,23].
In order to prevent the infiltration of the isotope, two coats of varnish were placed on the surface of the tooth up to 2 mm from margins around the restorations, except in group 4 where the entire surface was sealed [1]. The negative control in this experiment was intended to evaluate the reliability of the varnish, with regard to sealing, and this has been proven by the low scores in this group. Before gamma camera readings the varnish was removed, which influenced loss of tooth structure upon removal.
There are several methods by which microleakage can be studied such as the use of dyes, chemical tracers, radioactive isotopes, artificial caries, scanning electron microscopy, neutron activation analysis, and electrical conductivity [11]. In this study the radionuclide 99mTc was used due to the fact that this is the most widely use dradionuclide in the field of nuclear medicine, This radionuclide was selected as it is the most used of cold kits in the field of nuclear medicine for single photon emission, in addition to the fact of its half-decay time being approximately 6 hours [14,35]. The immersion time of the teeth in the solution of sodium pertechnetate was set a3 hours in order to have time for the foregoing procedures to measure theradiation by gamma camera. The samples were carefully prepared for quantification by gamma camera after immersion to prevent possible contamination after the immersion time. A gamma camera provided accurate radioactivity results in each sample.
When analysing the results, a statistically significant difference was observed between the control groups and study groups (p < 0.05), demonstrating that they were effective.
Both composite materials tested presented microleakage. In this study there was no statistically significant difference (p > 0.05) between the study groups. However, more microleak age occurred in group 1.
Between the negative control group and positive control group a highly significant difference was found (p < 0.001). Analysing the mean and standard deviation reveals that the negative control group presented the lowest values, while positive control group showed the highest values.
5. CONCLUSIONS
Within the limitations of this study, it can be concluded that:
• SonicFillTM and Filtek SupremeXTE do not differ regarding to microleakage.
• SonicFillTM only has the advantage of better clinical handling, reducing labour time.
• Using the radioisotope 99mTc as a marker of infiltration is simple, quick and fulfils the objective of a quantitative method in the evaluation of microleakage.
Long-term clinical studies need to be carried out to substantiate the results of this study.
REFERENCES
- Radhika, M., Sajjan, G., Kumaraswamy, B. and Mittal, N. (2010) Effect of different placement techniques on marginal microleakage of deep class-II cavities restored with two composite resin formulations. Journal of Conservative Dentistry, 13, 9-15. doi:10.4103/0972-0707.62633
- Ben-Amar, A., Slutzky, H. and Matalon, S. (2007) The influence of 2 condensation techniques on the marginal seal of packable resin composite restorations. Quintessence International, 38, 423-428.
- Schneider, L., Cavalcante, L. and Silikas, N. (2010) Shrinkage stresses generated during resin-composite applications: A review. Journal of Dental Biomechanics, 2010, 1-14.
- Zimmerli, B., Strub, M., Jeger, F., Stadler, O. and Lussi, A. (2010) Composite materials: Composition, properties and clinical applications. Schweiz Monatsschr Zahnmed, 120, 972-979.
- Vyver, P. (2000) Clinical application of a new flowable base material for direct and indirect restorations. International Dentistry, 12, 18-27.
- Helvatjoglu-Antoniades, M., Kalinderis, K., Pedulu, L. and Papadogiannis, Y. (2004) The effect of pulse activetion on microleakage of a “packable” composite resin and two “ormocers”. Journal of Oral Rehabilitation, 31, 1068-1074. doi:10.1111/j.1365-2842.2004.01337.x
- Burke, F., Crisp, R., James, A., Mackenzie, L., Pal, A., Sands, P., et al. (2011) Two year clinical evaluation of a low-shrink resin composite material in UK general dental practices. Dental Materials, 27, 622-630. doi:10.1016/j.dental.2011.02.012
- Mahmound, S. and Al-Wakeel, E. (2011) Marginal adaptation of ormocer-, silorane-, and methacrylate-based composite restorative systems bonded to dentin cavities after water storage. Quintessence International, 42, e131-e139.
- Hickel, R. and Manhart, J. (2001) Longevity of restorations in posterior teeth and reasons for failure. Journal of Adhesive Dentistry, 3, 45-64.
- Vicente, A., Ortiz, A. and Bravo, L. (2009) Microleakage beneath brackets bonded with flowable materials: Effect of thermocycling. European Journal of Orthodontics, 31, 390-396. doi:10.1093/ejo/cjn126
- Gogna, R., Jagadis, S. and Shashikal, K. (2011) A comparative in vitro study of microleakage by a radioactive isotope and compressive strength of three nanofilled composite resin restorations. Journal of Conservative Dentistry, 14, 128-131. doi:10.4103/0972-0707.82609
- Ernst, C.P., Brandenbusch, M., Meyer, G., Canbek, K., Gottschalk, F. and Willershausen, B. (2006) Two-year clinical performance of a nanofillervs a fine-particle hybrid resin composite. Clinical Oral Investigations, 10, 119-125. doi:10.1007/s00784-006-0041-8
- Sybron Dental Specialties Inc., “SonicFillTM System,” 2011. www.sonicfill.eu/
- U. Mazzi, “Techenetium in Medicine,” In: Zolle, I., Ed., Technetium-99m pharmaceuticals: Preparation and quality control in nuclear medicine. Springer, Berlin, 2007.
- Heintze, S. and Zimmerli, B. (2011) Relevance of in vitro tests of adhesive and composite dental materials (part 1). Schweiz Monatsschr Zahnmed, 121, 810-815.
- Majety, K. and Pujar, M. (2011) In vitro evaluation of microleakage of class II packable composite resin restorations using flowable composite and resin modified glass ionomers as intermediate layers. Journal of Conservative Dentistry, 14, 414-417. doi:10.4103/0972-0707.87215
- Roggendorf, M., Krämer, N., Appelt, A., Naumann, M. and Frankenberger, R. (2011) Marginal quality of flowable 4-mm base vs conventionally layered resin composite. Journal of Dentistry, 39, 643-647. doi:10.1016/j.jdent.2011.07.004
- Van Ende, A., Mine, A., De Munck, J., Poitevin, A. and Van Meerbeek, B. (2012) Bonding of low-shrinking composites in high C-factor cavities. Journal of Dentistry, 4, 295-303. doi:10.1016/j.jdent.2012.01.004
- Andrade, A., Duarte, R., Medeiros e Silva, F., Batista, A., Lima, K., Pontual, M., et al. (2011) 30-month randomised clinical trial to evaluate the clinical performance of a nanofill and a nanohybrid composite. Journal of Dentistry, 39, 8-15. doi:10.1016/j.jdent.2010.09.005
- Nalcacl, A. and Ulusoy, N. (2007) Effect of thermocycling on microleakage of resin composites polymerized with LED curing techniques. Quintessence International, 38, e433-e439.
- Mortazavi, V., Fathi, M. and Soltani, F. (2011) Effect of postoperative bleaching on etch-and-rinse and self-etch adhesives. Dental Research Journal, 8, 16-21.
- Amaral, F., Colucci, V., Palma-Dibb, R. and Corona, S. (2007) Assessment of in vitro methods used to promote adhesive interface degradation: A critical review. Journal of Esthetic and Restorative Dentistry, 19, 340-354. doi:10.1111/j.1708-8240.2007.00134.x
- Yuasa, T., Iijima, M., Ito, S., Muguruma, T., Saito, T. and Mizoguchi, I. (2010) Effects of long-term storage and thermocycling on bond strength of two self-etching primer adhesive systems. European Journal of Orthodontics, 32, 285-290. doi:10.1093/ejo/cjp118
- De Goes, M., Giannini, M., Di Hipólito, V., Carrilho, M., Daronch, M. and Rueggeberg, F. (2008) Microtensile bond strength of adhesive systems to dentin with or without application of an intermediate flowable resin layer. Brazilian Dental Journal, 19, 51-56. doi:10.1590/S0103-64402008000100009
- Perdigão, J., Dutra-Corrêa, M., Anauate-Netto, C., Castilhos, N., Carmo, A., Lewgoy, H., et al. (2009) Two-year clinical evaluation of self-etching adhesive posterior restorations. Journal of Adhesive Dentistry, 11, 149-159.
- Park, J., Chang, J., Ferracane, J. and Lee, I.B. (2008) How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dental Materials, 24, 1501-1505. doi:10.1016/j.dental.2008.03.013
- Lee, M.-R., Cho, B.-H., Son, H.-H., Um, C.-M. and Lee, I.-B. (2007) Influence of cavity dimension and restoration methods on the cusp deflection of premolars in composite restoration. Dental Materials, 23, 288-295. doi:10.1016/j.dental.2006.01.025
- Versluis, A., Douglas, W.H., Cross, M. and Sakaguchi, R.L. (1996) Does an incremental filling technique reduce polymerization shrinkage stresses? Journal of Dental Research, 75, 871-878. doi:10.1177/00220345960750030301
- Loguercio, A.D., Reis, A. and Ballester, R.Y. (2004) Polymerization shrinkage: Effects of constraint and filling technique in composite restorations. Dental Materials, 20, 236-243. doi:10.1016/S0109-5641(03)00098-8
- Penido, S., Penido, C., Santos-Pinto, A., Sakima, T. and Fontana, C. (2008) Estudo in vivo e in vitro com e sem termociclagem, da resistência ao cisalhamento de braquetes colados com fonte de luz halógena. Revista Dental Press de Ortodontia e Ortopedia Facial, 13, 66-76.
- Loguercio, A., Bauar, J., Reis, A. and Grande, R. (2004) In vitro microleakage of packable composites in Class II restorations. Quintessence International, 35, 29-34.
- Geerts, S., Seidel, L., Albert, A. and Gueders, A. (2010) Microleakage after thermocycling of three self-etch adhesives under resin-modified glass-ionomer cement restorations. International Journal of Dentistry, 2010, 1-6.
- Souza, R., Özcan, M., Michida, S., Melo, R., Pavanelli, C., Bottino, M., et al. (2010) Conversion degree of indirect resin composites and effect of thermocycling on their physical properties. Journal of Prosthodontics, 19, 218-225. doi:10.1111/j.1532-849X.2009.00551.x
- Turk, T., Elekdag-Turk, S., Isci, D., Cakmak, F. and Ozkalayci, N. (2010) Shear bond strength of a self-etching primer after 10,000 and 20,000 thermal cycles. Journal of Adhesive Dentistry, 12, 117-122.
- Ferreira, M., Botelho, M., Abrantes, M., Oliveiros, B. and Carrilho, E. (2010) Quantitative scintigraphic analysis of pulp revascularization in autotransplanted teeth in dogs. Archives of Oral Biology, 55, 825-829. doi:10.1016/j.archoralbio.2010.07.005

