Open Journal of Preventive Medicine
Vol.3 No.2(2013), Article ID:30921,4 pages DOI:10.4236/ojpm.2013.32035
Prescription of intermittent preventive therapy (IPTp) among doctors practicing in an army hospital in Lagos, Nigeria
![]()
1Department of Medicine, 68 Nigerian Army Reference Hospital Yaba Lagos, Lagos, Nigeria; *Corresponding Author: nke1207@yahoo.com
2Department of Community Health and Primary Care, College of Medicine, University of Lagos Idi-Araba, Lagos, Nigeria
3Clinical Divisions, Nigerian Institute of Medical Research Yaba Lagos, Lagos, Nigeria
Copyright © 2013 Nkechinyere E. Harrison et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 13 January 2013; revised 11 March 2013; accepted 20 April 2013
Keywords: Prescription; Intermittent Preventive Therapy for Malaria; Army Hospital
ABSTRACT
Background: Malaria infestation in pregnancy is a major public health concern and ranks amongst the commonest complications of pregnancy in Nigeria. Approximately 50,000 Nigerian women die each year from largely preventable pregnancy related complications. Intermittent preventive therapy for malaria in pregnancy (IPTp) is a key recommendation in the National guideline for malaria treatment in Nigeria. This study assessed the prescription pattern of intermittent preventive therapy with Sulphadoxine-Pyrimethamine for pregnant women among doctors practicing in 68 Nigerian Army Reference Hospital, Yaba, Lagos, Nigeria. Methods: This was a retrospective study using case notes of pregnant women seen at antenatal clinic of 68 Nigerian Army Reference Hospital, Yaba, Lagos, Nigeria from January, 2008 to December, 2008. A total of 336 case notes were reviewed. The findings were precoded, data entry and analysis was done using EPI INFO 2002. Results: A good proportion of the women (82.9%) booked for antenatal clinic within the first and second trimesters of pregnancy. Most commonly prescribed by doctors was the weekly pyrimethamine (daraprim) for malaria prophylaxis in pregnancy (100.0%). Very few doctors prescribed intermittent preventive therapy with sulfadoxine-pyrimethamine, and the few who did prescribed just one dose. Conclusion: The study showed a very low level of prescription of IPTp among doctors practicing at 68 Nigerian Army Reference Hospital, Yaba, Lagos, Nigeria. There is a great need for training of these doctors and other health professionals on the recommendations of the current National Antimalarial Treatment Guidelines.
1. BACKGROUND
Each year approximately 50 million women living in malaria-endemic countries throughout the world become pregnant, of whom over half live in tropical areas of Africa with intense transmission of Plasmodium falciparum [1]. Nigeria accounts for a quarter of all malaria cases in the World Health Organization (WHO) African region [2]. Approximately 50,000 Nigerian women die each year from largely preventable pregnancy related complications [3].
Malaria infestation in pregnancy is a major public health concern and ranks amongst the commonest complications of pregnancy in Nigeria [4]. Pregnant women in malarious areas may experience a variety of adverse consequences from malaria infection including maternal anaemia, low birth weight of neonates from prematurity and intrauterine growth retardation, amongst others [5,6]. Resistance of Plasmodium falciparum to drugs is the most important problem in malaria chemotherapy; this resistance also affects drugs used in pregnancy for prophylaxis and treatment of clinical malaria [4].
In response to WHO recommendation, the Nigerian National Antimalarial Treatment guideline was released in May 2005, by the Federal Ministry of Health [7].
This policy and guidelines recommend the use of Intermittent Preventive Therapy (IPTp) with one full dose of sulfadoxine-pyrimethamine (SP) during the second and third trimesters of pregnancy given not earlier than 16 weeks gestation nor later than 36 weeks gestation
[7,8]. For clinical malaria, quinine is considered safe in pregnancy and can be used in all trimesters; artemisinin based combination therapy is considered safe in second and third trimesters and can be used then [7,8].
This study assessed the prescription pattern of intermittent preventive therapy with SP for pregnant women among doctors practicing in 68 Nigerian Army Reference Hospital, Yaba, Lagos, Nigeria.
2. METHODS
The study area lies in south western Nigeria, in the gulf of Guinea west of the Niger River delta. It is located on the longitude 3˚24'E and latitude 6˚27'N. The monthly rainfall varies from the lowest of 35 mm (1.5 inches) in January to the highest of 300 mm (12 inches) in July [9].
The study was done at 68 Nigerian Army Reference Hospital Yaba, Lagos which is located in Yaba Local Council Development Area of Lagos State with 500 bed capacity and operates as a tertiary centre. It runs two antenatal clinics weekly with average clinic attendance of 58 pregnant women.
Three hundred and thirty six case notes of pregnant women booked for antenatal care from January to December 2008 and followed up till delivery were reviewed; this data was extracted between November 2009 and February 2010. However case notes of women with booking gestational age greater than 36 weeks were excluded from the analysis. There were 15 in number hence 321 case notes were analyzed. The study was reviewed and approved by 68 Nigerian Army Reference Hospital Yaba, Lagos Ethical Committee. Data entry and processing was done using EPI-INFO 2002. Test of significance was done using chi-square test, and statistical significance was considered at 95% confidence level.
The Nigeria National antimalarial treatment policy and guidelines (2005) was used in this study as benchmark for recommended malaria treatment practices [7,8].
3. RESULTS
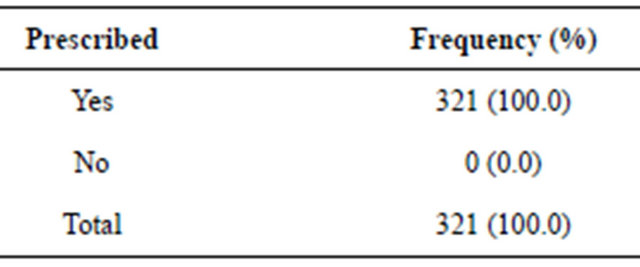
The mean age of the women was 28.5 (SD ± 4.6 years). Less than half of the women were wives of army personnel (Table 1). A little above one-fifth (21.5%) of the women booked for antenatal care in the first trimester of pregnancy, 60.4% in the second trimester and 18.1% in the third trimester (Table 2). Husband occupation as army or civilian showed no significant relationship when compared with gestational age at booking (p = 0.36). Weekly pyrimethamine prophylaxis was prescribed for all the cases reviewed (Table 3). Intermittent preventive therapy with sulfadoxine-pyrimethamine was prescribed for 3.7% of cases reviewed, and all received just one
Table 1. Demographic characteristics of clients, n = 321.
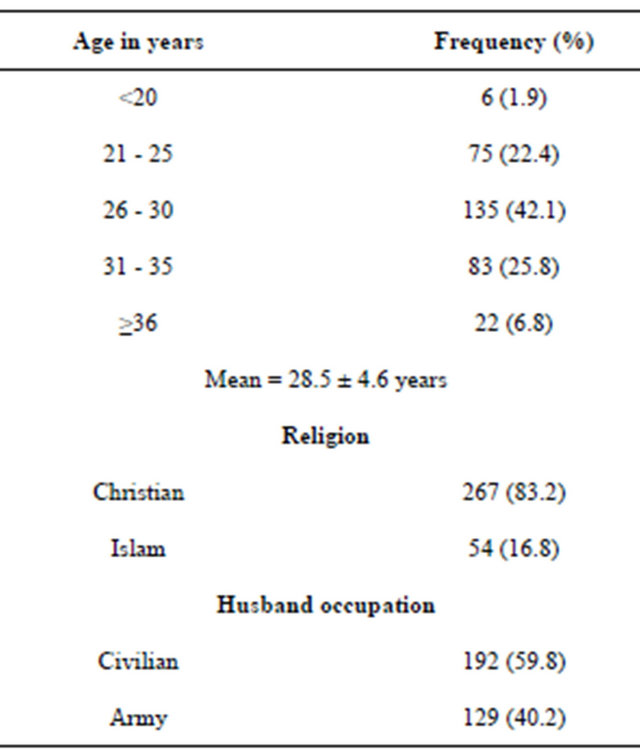
Table 2. Gestational age at anc booking.
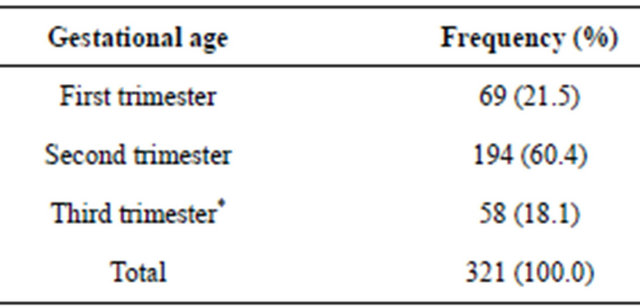
*>36 weeks excluded.
Table 3. Weekly Pyrimethamine (daraprim) prophylaxis.
dose (2.4% in second trimester and 1.3% in third trimester) (Table 4). Average number of antenatal clinic visits was 7.
Therapeutic treatment for clinical malaria was indicated in 18.75% of the case notes.
4. DISCUSSION
This study revealed a very low level of prescription of intermittent preventive therapy with sulfadoxine-pyrimethamine (SP) in pregnancy at the 68 Nigerian Army Reference Hospital Yaba, Lagos. All the case notes reviewed showed that all the women were given weekly pyrimethamine.
This implies that those who received IPTp were al-
Table 4. Intermittent Preventive therapy (iptp) using sulphadoxine/pyrimethamine (SP).
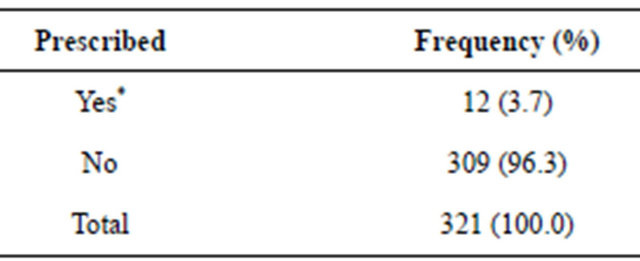
*All received one dose.
ready on weekly pyrimethamine therapy, and says a lot about the presciption patterns of the doctors studied. These results suggest that there is need for retraining and reorientation of the doctors, so as to bring their prescription practices in line with the current antimalarial treatment guidelines.
This low prescription pattern of IPTp is in keeping with an observation made by WHO in the World Malaria Report 2010, which noted that coverage with intermittent preventive therapy for pregnant women (IPTp) remains far from target level [10].
In addition, the 2008 Nigeria Demographic and Health Survey showed very low uptake of IPTp (8% for one dose and 5% for two doses) [11]. This low uptake could be due to inertia to change, lack of understanding of the policy/guideline, unavailability of the drugs amongst other reasons. There is need for further studies to unravel the reason for this low level of prescription both in this health facility and in others across the country. It was observed that though few countries have made notable progress, the percentage of women who received the second dose of IPTp ranged from 2.4% in Angola to 62% in Zambia according to a household survey in 8 countries for which data were available for 2007-2009 [10].
The observation in this study differs from that of a study in Koupala District of Burkino Faso where IPTp prescription for one dose was as high as 96.2% in the antenatal clinics and 93.5% in the delivery units (DU) [12]. In this instance, their Federal Ministry of Health piloted the program and accelerated the distribution of SP and ITNs and this could have contributed to the high level of prescription. Another study from Senegal where inspection of antenatal and outpatient clinic registries was done between 2000-2007 showed a high prescription of IPTp with 70% prescribing two doses of SP [13].
New delivery approaches based on community mobilization, community directed intervention and training resource persons have been shown to achieve better compliance to two doses of SP in studies done in Uganda and Akwa Ibom state, Nigeria [14,15].
More studies and possible application of these community based interventions coupled with capacity building of health workers could be a welcome means of achieving desired target for uptake of IPTp.
5. CONCLUSION
The study showed a very low level of prescription of IPTp among doctors practicing at 68 Nigerian Army Reference Hospital, Yaba, Lagos, Nigeria. There is a great need for training and retraining of these doctors and other health professionals on the recommendations of the current National Antimalarial Treatment Guidelines. There is also need to ensure availability of the IPTdrugs at the health facilities.
6. ACKNOWLEDGEMENTS
We thank Dr. Obioha Njideka T for assisting in the data collection.
REFERENCES
- World Health Organization (WHO) (2010) Malaria in pregnancy. WHO, Geneva.
- World Health Organization (2008) World malaria report. WHO, Geneva, 1-215.
- Erim, D.O., Resch, S.C. and Goldie, S.J. (2012) Assessing health and economic outcomes of interventions to reduce pregnancy-related mortality in Nigeria. BMC Public Health, 12, 786.
- Omo-Aghoja, L.O., Aghoja, C.O., Oghagbo, K., OmoAghoja, V.W. and Ezume, C. (2008) Prevention and treatment of malaria in pregnancy in Nigeria: Obstetrician’s knowledge of guidelines and policy changes—A call for action. Journal of Chinese Clinical Medicine, 3, 114-120.
- Steketee, R., Nahlen, B., Praise, M. and Menendez, C. (2001) The burden of malaria in pregnancy in malariaendemic areas. American Journal of Tropical Medicine and Hygiene, 64, 28-35.
- Steketee, R.W., Winam, J.J., Hightower, A.W., Slusker, L., Hymann, D.L. and Breman, J.G. (1996) The effect of malaria and malaria prevention on offspring birthweight, prematurity, intrauterine growth retardation in rural Malawi. American Journal of Tropical Medicine and Hygiene, 55, 33-41.
- Federal Ministry of Health (2005) National antimalarial treatment policy. Federal Ministry of Health, Abuja.
- Federal Ministry of Health (2005) National antimalarial treatment guidelines. Federal Ministry of Health, Abuja.
- Wikipedia, Lgos. http://www.en.wikipedia.org/wiki/lagos
- World Health Organization (2010) World malaria report. WHO, Geneva.
- NPC and ICF Macro (2009) Nigeria 2008 demographic and health survey: Key findings. NPC and ICF Macro, Calverton, 1-20.
- Sirima, S.B., Cotte, A.H., Konate, A., Moran, A.C., Asamoa, K., Bouquoma, E.C., Diarra, A., Quedraoqo, A., Praise, M.E. and Newman, R.D. (2006) Malaria Prevention during pregnancy: Assessing the disease burden one year after implementing a program of intermittent preventive treatment in Koupela District, Burkina Faso. American Journal of Tropical Medicine and Hygiene, 75, 205-211.
- Olliaro, P.L., Delenne, H., Cisse, M., Badiane, M., Olliaro, A., Vaillant, M. and Brasseur, P. (2008) Implementation of intermittent preventive treatment in pregnancy with sulphadoxine/pyrimethamine (IPTp-SP) at a district health centre in rural Senegal. Malaria Journal, 7, 234. doi:10.1186/1475-2875-7-234
- Mbonye, A.K., Byjbjerg, I.C. and Magnussen, P. (2008) Intermittent preventive treatment of malaria in pregnancy: A new delivery system and its effect on maternal health and pregnancy outcomes in Uganda. Bulletin of World Health Organization, 86, 8.
- Okeibunor, J.C., Orji, B.C., Brieger, W., Ishola, G., Otolorin, E., Rawlins, B., Ndekhedehe, E.U., Onyeneho, N. and Fink. G. (2011) Preventing Malaria in pregnancy through community-directed interventions: Evidence from Akwa Ibom State, Nigeria. Malaria Journal, 10, 227. doi:10.1186/1475-2875-10-227

