Paper Menu >>
Journal Menu >>
 Vol.2, No.4, 376-380 (2010) Health doi:10.4236/health.2010.24056 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Cardio-Toxicity during chemotherapy: feasibility of new diagnostic approaches Fable Zustovich1, Mario Trivellato2, Renato Ceravolo1, Davide Pastorelli1, Rosanna Canton2, Lorena Buratin2, Monica Mion3, Martina Zaninotto3, Martina Mattiazzi1, Mario Plebani3, Giuseppe Cartei1 1Oncologia Medica 1° piano, IOV – IRCCS, Padova, Italy; fable.zustovich@ioveneto.it 2Servizio di Cardiologia ULSS16 c/o IRA, Padova, Italy 3Dipartimento di Medicina di Laboratorio, Università – Azienda Ospedaliera, Padova, Italy Received 25 October 2009; revised 28 November 2009; accepted 5 December 2009. ABSTRACT Chemotherapy induced cardio-toxicity is a well known side effect of anticancer treatments, moreover the 70% of all tumors involve patients over 65 years-old, frequently with cardiac co- morbidity. We evaluated the feasibility of the application during chemotherapy administration of some of the most recent diagnostic tech- niques as 12-diagnostic leads telemetry, 7 days EKG monitoring device (R-Test Evolution 3R), blood level dosage of Brain Natriuretic Peptide (BNP) and Ischemia Modified Albumin (IMA). Some sub-clinical changes in the investigated parameters were found in patients undergoing chemotherapy, mostly containing fluorouracil, as shown in the following paper. Far from sug- gesting a widespread use of these methods during chemotherapy administration, we think that some more tools are needed to prevent cardiac toxicity in high-risk patients and some of what we studied may deserve further valua- tion in chemotherapy clinical trials. Keywords: Cardio-Toxicity Diagnostic 1. INTRODUCTION The rising percentage of older subjects among cancer patients has led oncologists to manage chemotherapy administration often dealing with severe concomitant diseases, mostly cardiovascular. Chemotherapy induced cardio-toxicity is a well known side effect of anticancer treatment. Among the most cardio- toxic a gents there are anthr acyclines, 5-fluor ouracil, t a x a n e s and Trastuzumab. These agents may cause left ventricu- lar dysfunction as well as arrhyth mias and/or ST-T wave changes [1]. The evaluation of the cardiac safety during cardio toxic chemotherapy is usually based on standard EKG, EKG Holter and mostly using echo-color doppler car- diography. All these methods reveal cardiac damage when macroscopic morphological alterations have been reached, thus when damage is already present and often irreversible. New methods of investigation are needed in attempt to detect a subclinical damage and to prevent the symptomatic cardiac failure. We evaluated the feasibility of some new techniques planning prospective preliminary studies monitoring patients undergoing potentially cardio toxic chemotherapy with 12-diagnostic leads EKG telemetry (TDLT), 7 days EKG monitoring dev ice (R-Test Evolution 3R), blood level dosages of Brain Natriuretic Peptide (BNP) and Ischemia Modified Albumin (IMA). 2. TWELVE-DIAGNOSTIC LEADS TE- LEMETRY (TDLT) The TDLT monitors continuously 12 diagnostic leads electrocardiogram and gives a real time analysis with events comparing with basal reference. The telemetry monitor (Mortara Rangoni Europe) had the following characteristics: acquisition data amplifier with analogue digital converter (ADC) = 20 bit; sam- pling sample channel (SSC) = 10000 Hz; low significant bit (LSB) = 1.2 microVolt; band with 0.05-100 Hz; te- lemetry transmission = 2.4 GHz. The system has high accuracy for arrhythmias and ischemia. Comparison among different time events and ST movements histo- grams with automatic continuous bit by bit data storage were also available. Patients were allowed to walk dur- ing TDLT. We firstly studied prospectively some aspects of car- diac toxicity in patients during gemcitabine chemother- apy infusion for non-small cell lung cancer (NSCLC) [2]. Seventeen patients were evaluated, 12 male and 5 female, 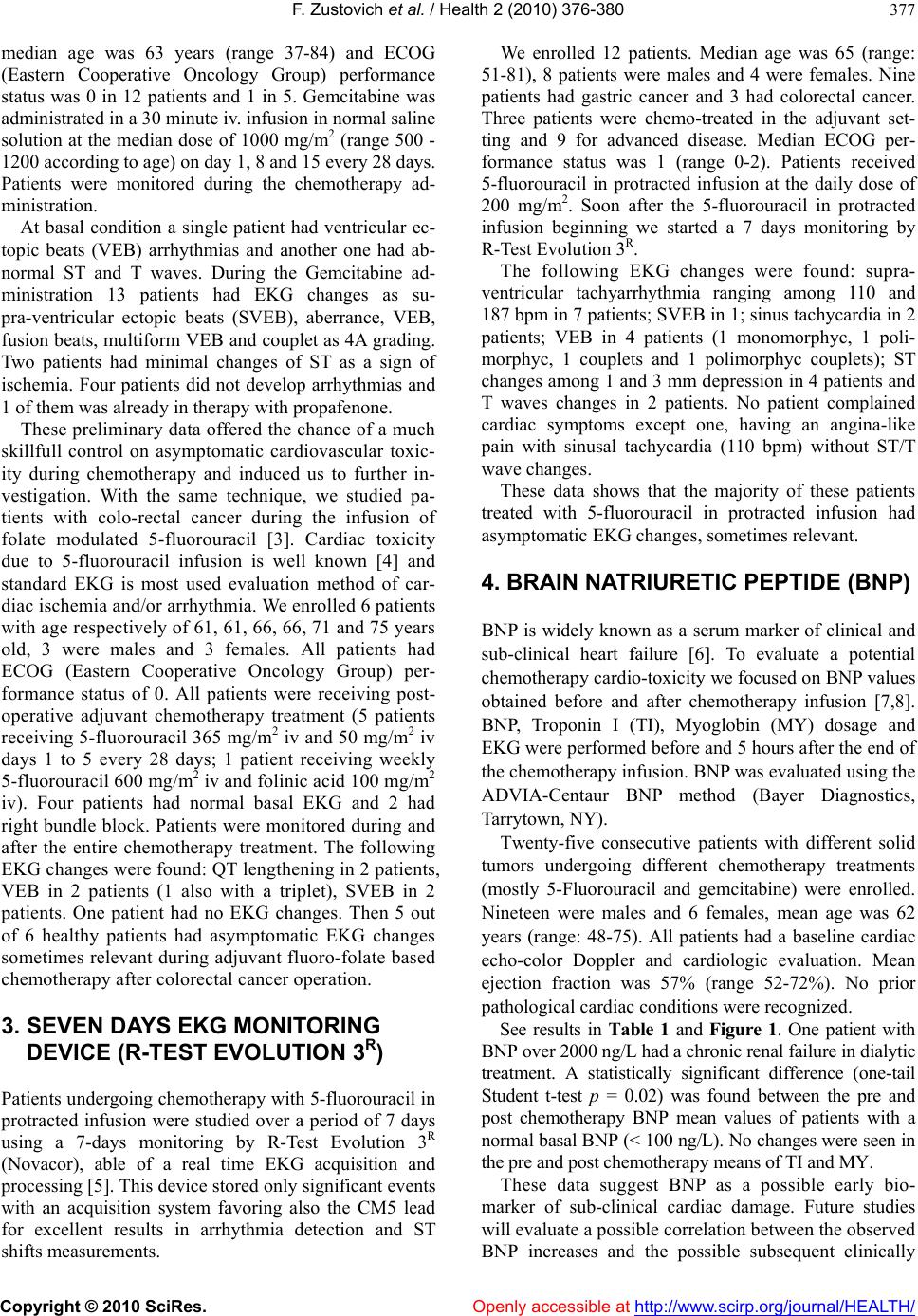 F. Zustovich et al. / Health 2 (2010) 376-380 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 377 median age was 63 years (range 37-84) and ECOG (Eastern Cooperative Oncology Group) performance status was 0 in 12 patients and 1 in 5. Gemcitabine was administrated in a 30 minute iv. infusion in normal saline solution at the median dose of 1000 mg/m2 (range 500 - 1200 according to age) on day 1, 8 and 15 every 28 days. Patients were monitored during the chemotherapy ad- ministration. At basal condition a single patient had ventricular ec- topic beats (VEB) arrhythmias and another one had ab- normal ST and T waves. During the Gemcitabine ad- ministration 13 patients had EKG changes as su- pra-ventricular ectopic beats (SVEB), aberrance, VEB, fusion beats, multiform VEB and couplet as 4A grading. Two patients had minimal changes of ST as a sign of ischemia. Four patients did not develop arrhythmias and 1 of them was already in therapy with propafenone. These prelimin ary data offered the chance of a much skillfull control on asymptomatic cardiovascular toxic- ity during chemotherapy and induced us to further in- vestigation. With the same technique, we studied pa- tients with colo-rectal cancer during the infusion of folate modulated 5-fluorouracil [3]. Cardiac toxicity due to 5-fluorouracil infusion is well known [4] and standard EKG is most used evaluation method of car- diac ischemia and/or arrhythmia. We enrolled 6 patients with age respectively of 61, 61, 66, 66, 71 and 75 years old, 3 were males and 3 females. All patients had ECOG (Eastern Cooperative Oncology Group) per- formance status of 0. All patients were receiving post- operative adjuvant chemotherapy treatment (5 patients receiving 5-fluorouracil 365 mg/m2 iv and 50 mg/m2 iv days 1 to 5 every 28 days; 1 patient receiving weekly 5-fluorouracil 600 mg/m2 iv and folinic acid 100 mg/m2 iv). Four patients had normal basal EKG and 2 had right bundle block. Patients were monitored during and after the entire chemotherapy treatment. The following EKG changes were found: QT lengthening in 2 patients, VEB in 2 patients (1 also with a triplet), SVEB in 2 patients. One patient had no EKG changes. Then 5 out of 6 healthy patients had asymptomatic EKG changes sometimes relevant during adjuvant fluoro-folate based chemotherapy after colorectal cancer operation. 3. SEVEN DAYS EKG MONITORING DEVICE (R-TEST EVOLUTION 3R) Patients undergoing chemotherapy with 5-fluorouracil in protracted infusion were studied over a period of 7 days using a 7-days monitoring by R-Test Evolution 3R (Novacor), able of a real time EKG acquisition and processing [5]. This device stored only significant events with an acquisition system favoring also the CM5 lead for excellent results in arrhythmia detection and ST shifts measurements. We enrolled 12 patients. Median age was 65 (range: 51-81), 8 patients were males and 4 were females. Nine patients had gastric cancer and 3 had colorectal cancer. Three patients were chemo-treated in the adjuvant set- ting and 9 for advanced disease. Median ECOG per- formance status was 1 (range 0-2). Patients received 5-fluorouracil in protracted infusion at the daily dose of 200 mg/m2. Soon after the 5-fluorouracil in protracted infusion beginning we started a 7 days monitoring by R-Test Evolution 3R. The following EKG changes were found: supra- ventricular tachyarrhythmia ranging among 110 and 187 bpm in 7 patients; SVEB in 1; sinus tachycardia in 2 patients; VEB in 4 patients (1 monomorphyc, 1 poli- morphyc, 1 couplets and 1 polimorphyc couplets); ST changes among 1 and 3 mm depression in 4 patients and T waves changes in 2 patients. No patient complained cardiac symptoms except one, having an angina-like pain with sinusal tachycardia (110 bpm) without ST/T wave changes. These data shows that the majority of these patients treated with 5-fluorouracil in protracted infusion had asymptomatic EKG changes, sometimes relevant. 4. BRAIN NATRIURETIC PEPTIDE (BNP) BNP is widely known as a serum marker of clinical and sub-clinical heart failure [6]. To evaluate a potential chemotherapy cardio-toxicity we focused on BNP values obtained before and after chemotherapy infusion [7,8]. BNP, Troponin I (TI), Myoglobin (MY) dosage and EKG were performed be fore and 5 hours after the end of the chemotherapy infusion. BNP was evaluated using the ADVIA-Centaur BNP method (Bayer Diagnostics, Tarrytown, NY ). Twenty-five consecutive patients with different solid tumors undergoing different chemotherapy treatments (mostly 5-Fluorouracil and gemcitabine) were enrolled. Nineteen were males and 6 females, mean age was 62 years (range: 48-75). All patients had a baseline cardiac echo-color Doppler and cardiologic evaluation. Mean ejection fraction was 57% (range 52-72%). No prior pathological cardiac conditions were recognized. See results in Table 1 and Figure 1. One patient with BNP over 2000 ng/L had a chronic renal fail ure in dialyti c treatment. A statistically significant difference (one-tail Student t-test p = 0.02) was found between the pre and post chemotherapy BNP mean values of patients with a normal basal BNP (< 100 ng/L). No changes were seen in the pre and post chemotherapy means of TI and MY. These data suggest BNP as a possible early bio- marker of sub-clinical cardiac damage. Future studies will evaluate a possible correlation between the observed BNP increases and the possible subsequent clinically 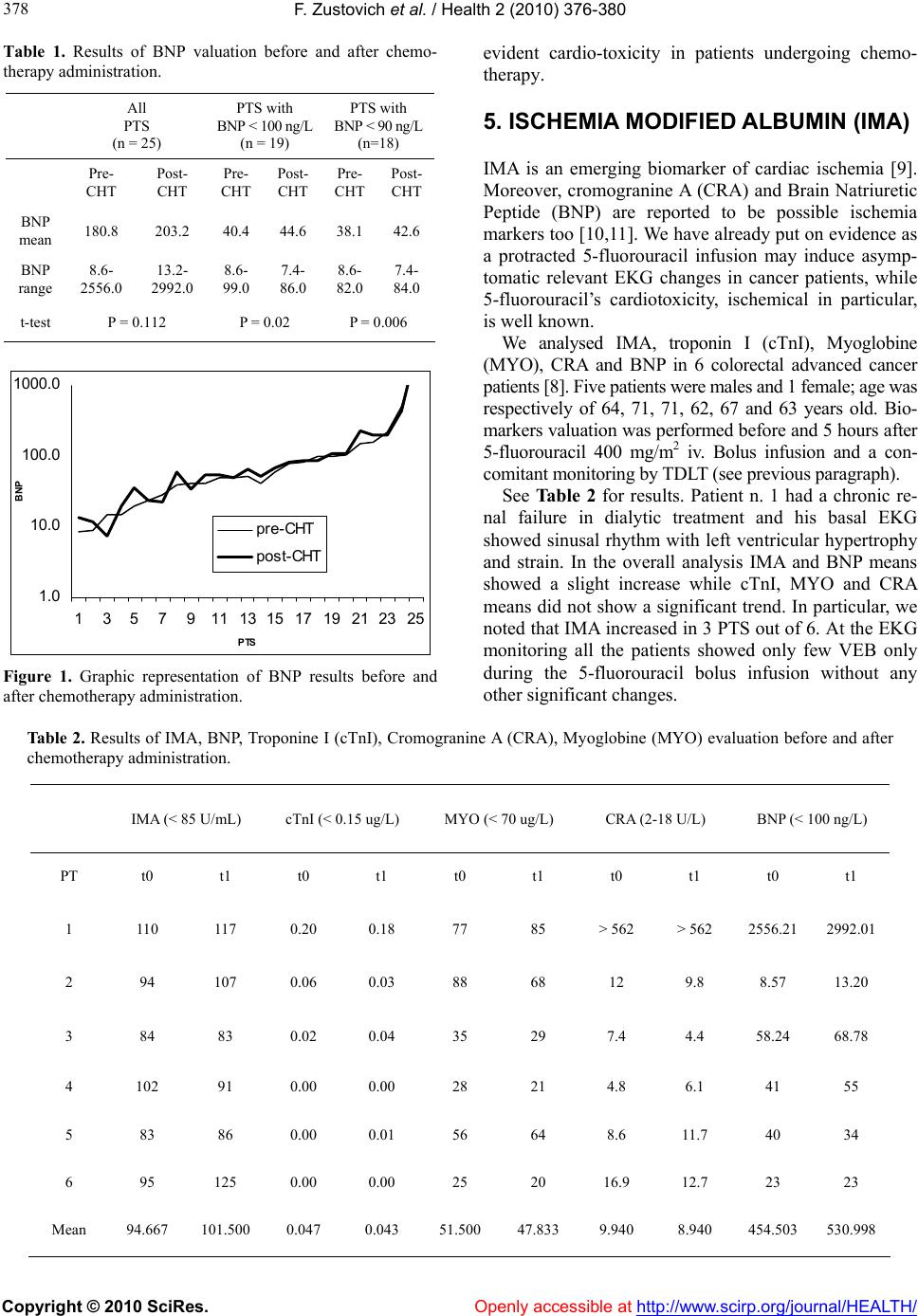 F. Zustovich et al. / Health 2 (2010) 376-380 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 378 Table 1. Results of BNP valuation before and after chemo- therapy administration. All PTS (n = 25) PTS with BNP < 100 ng/L (n = 19) PTS with BNP < 90 ng/L (n=18) Pre- CHT Post- CHT Pre- CHT Post- CHT Pre- CHT Post- CHT BNP mean 180.8 203.2 40.4 44.6 38.142.6 BNP range 8.6- 2556.0 13.2- 2992.0 8.6- 99.0 7.4- 86.0 8.6- 82.0 7.4- 84.0 t-test P = 0.112 P = 0.02 P = 0.006 1.0 10.0 100.0 1000.0 1357911 1315 17 19 2123 25 PTS BNP pre-CHT post-CHT Figure 1. Graphic representation of BNP results before and after chemotherapy administration. evident cardio-toxicity in patients undergoing chemo- therapy. 5. ISCHEMIA MODIFIED ALBUMIN (IMA) IMA is an emerging biomarker of cardiac ischemia [9]. Moreover, cromogranine A (CRA) and Brain Natriuretic Peptide (BNP) are reported to be possible ischemia markers too [10,11]. We have already put on evidence as a protracted 5-fluorouracil infusion may induce asymp- tomatic relevant EKG changes in cancer patients, while 5-fluorouracil’s cardiotoxicity, ischemical in particular, is well known. We analysed IMA, troponin I (cTnI), Myoglobine (MYO), CRA and BNP in 6 colorectal advanced cancer patients [8]. Five patients were males and 1 female; age was respectively of 64, 71, 71, 62, 67 and 63 years old. Bio- markers valuation was performed before and 5 hours after 5-fluorouracil 400 mg/m2 iv. Bolus infusion and a con- comitant monitoring by TDLT (see previous paragraph). See Table 2 for results. Patient n. 1 had a chronic re- nal failure in dialytic treatment and his basal EKG showed sinusal rhythm with left ventricular hypertrophy and strain. In the overall analysis IMA and BNP means showed a slight increase while cTnI, MYO and CRA means did not show a significant trend. In particular, we noted that IMA increased in 3 PTS out of 6. At the EKG monitoring all the patients showed only few VEB only during the 5-fluorouracil bolus infusion without any other significant changes. Table 2. Results of IMA, BNP, Troponine I (cTnI), Cromogranine A (CRA), Myoglobine (MYO) evaluation before and after chemotherapy administration. IMA (< 85 U/mL) cTnI (< 0.15 ug/L) MYO (< 70 ug/L) CRA (2-18 U/L) BNP (< 100 ng/L) PT t0 t1 t0 t1 t0 t1 t0 t1 t0 t1 1 110 117 0.20 0.18 77 85 > 562 > 562 2556.21 2992.01 2 94 107 0.06 0.03 88 68 12 9.8 8.57 13.20 3 84 83 0.02 0.04 35 29 7.4 4.4 58.24 68.78 4 102 91 0.00 0.00 28 21 4.8 6.1 41 55 5 83 86 0.00 0.01 56 64 8.6 11.7 40 34 6 95 125 0.00 0.00 25 20 16.9 12.7 23 23 Mean 94.667 101.500 0.047 0.043 51.500 47.833 9.940 8.940 454.503 530.998 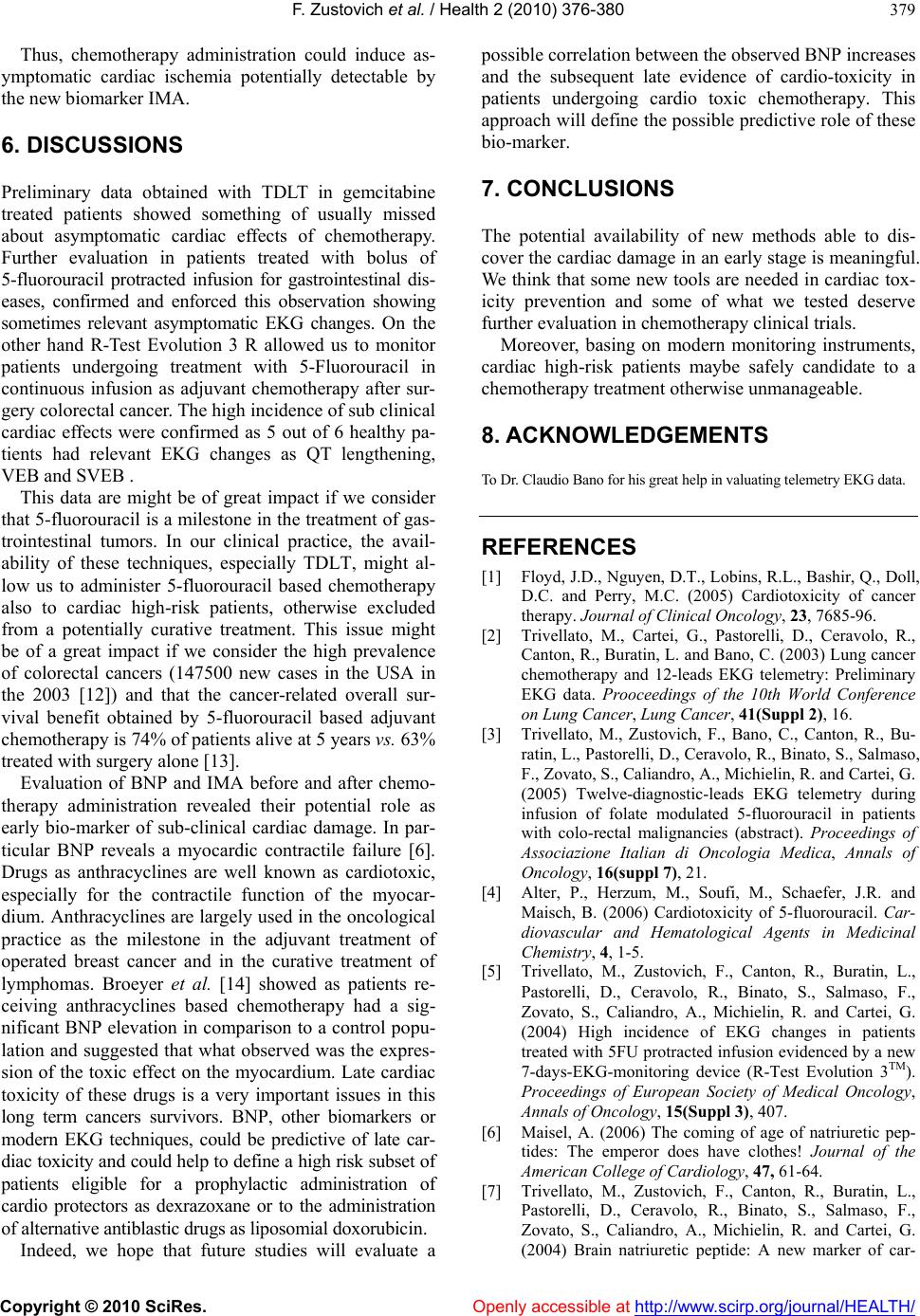 F. Zustovich et al. / Health 2 (2010) 376-380 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 379 Thus, chemotherapy administration could induce as- ymptomatic cardiac ischemia potentially detectable by the new biomarker IMA. 6. DISCUSSIONS Preliminary data obtained with TDLT in gemcitabine treated patients showed something of usually missed about asymptomatic cardiac effects of chemotherapy. Further evaluation in patients treated with bolus of 5-fluorouracil protracted infusion for gastrointestinal dis- eases, confirmed and enforced this observation showing sometimes relevant asymptomatic EKG changes. On the other hand R-Test Evolution 3 R allowed us to monitor patients undergoing treatment with 5-Fluorouracil in continuous infusion as adjuvant chemotherapy after sur- gery colorectal cancer. The high incidence of sub clinical cardiac effects were confirmed as 5 out of 6 healthy pa- tients had relevant EKG changes as QT lengthening, VEB and SVEB . This data are might be of great impact if we consider that 5-fluorouracil is a milestone in the treatment of gas- trointestinal tumors. In our clinical practice, the avail- ability of these techniques, especially TDLT, might al- low us to administer 5-fluorouracil based chemotherapy also to cardiac high-risk patients, otherwise excluded from a potentially curative treatment. This issue might be of a great impact if we consider the high prevalence of colorectal cancers (147500 new cases in the USA in the 2003 [12]) and that the cancer-related overall sur- vival benefit obtained by 5-fluorouracil based adjuvant chemotherapy is 74% of patients alive at 5 years vs. 63% treated with surgery alone [13]. Evaluation of BNP and IMA before and after chemo- therapy administration revealed their potential role as early bio-marker of sub-clinical cardiac damage. In par- ticular BNP reveals a myocardic contractile failure [6]. Drugs as anthracyclines are well known as cardiotoxic, especially for the contractile function of the myocar- dium. Anthracyclines are largely used in the oncological practice as the milestone in the adjuvant treatment of operated breast cancer and in the curative treatment of lymphomas. Broeyer et al. [14] showed as patients re- ceiving anthracyclines based chemotherapy had a sig- nificant BNP elevation in comparison to a control popu- lation and suggested that what observed was the expres- sion of the toxic effect on the myocardium. Late cardiac toxicity of these drugs is a very important issues in this long term cancers survivors. BNP, other biomarkers or modern EKG techniques, could be predictive of late car- diac toxicity and could help to define a high risk subset of patients eligible for a prophylactic administration of cardio protectors as dexrazoxane or to the administration of alternative antiblasti c drugs as liposom ial doxorubicin. Indeed, we hope that future studies will evaluate a possible correlation between the observed BNP increases and the subsequent late evidence of cardio-toxicity in patients undergoing cardio toxic chemotherapy. This approach will define the possible predictive role of these bio-marker. 7. CONCLUSIONS The potential availability of new methods able to dis- cover the cardiac damage in an early stage is meaningful. We think that some new tools are needed in cardiac tox- icity prevention and some of what we tested deserve further evaluation in chemotherapy clinical trials. Moreover, basing on modern monitoring instruments, cardiac high-risk patients maybe safely candidate to a chemotherapy treatm e nt otherwi se unmanageable. 8. ACKNOWLEDGEMENTS To Dr. Cla ud io B ano for his gr ea t hel p in val uat in g telemetry EKG data . REFERENCES [1] Floyd, J.D., Nguyen, D.T., Lobins, R.L., Bashir, Q., Doll, D.C. and Perry, M.C. (2005) Cardiotoxicity of cancer therapy. Journal of Clinical Oncology, 23, 7685-96. [2] Trivellato, M., Cartei, G., Pastorelli, D., Ceravolo, R., Canton, R., Buratin, L. and Bano, C. (2003) Lung cancer chemotherapy and 12-leads EKG telemetry: Preliminary EKG data. Prooceedings of the 10th World Conference on Lung Cancer, Lung Cancer, 41(Suppl 2), 16. [3] Trivellato, M., Zustovich, F., Bano, C., Canton, R., Bu- ratin, L., Pastorelli, D., Ceravolo, R., Binato, S., Salmaso, F., Zovato, S., Caliandro, A., Michielin, R. and Cartei, G. (2005) Twelve-diagnostic-leads EKG telemetry during infusion of folate modulated 5-fluorouracil in patients with colo-rectal malignancies (abstract). Proceedings of Associazione Italian di Oncologia Medica, Annals of Oncology, 16(suppl 7), 21. [4] Alter, P., Herzum, M., Soufi, M., Schaefer, J.R. and Maisch, B. (2006) Cardiotoxicity of 5-fluorouracil. Car- diovascular and Hematological Agents in Medicinal Chemistry, 4, 1-5. [5] Trivellato, M., Zustovich, F., Canton, R., Buratin, L., Pastorelli, D., Ceravolo, R., Binato, S., Salmaso, F., Zovato, S., Caliandro, A., Michielin, R. and Cartei, G. (2004) High incidence of EKG changes in patients treated with 5FU protracted infusion evidenced by a new 7-days-EKG-monitoring device (R-Test Evolution 3TM). Proceedings of European Society of Medical Oncology, Annals of Oncology, 15(Suppl 3), 407. [6] Maisel, A. (2006) The coming of age of natriuretic pep- tides: The emperor does have clothes! Journal of the American College of Cardiology, 47, 61-64. [7] Trivellato, M., Zustovich, F., Canton, R., Buratin, L., Pastorelli, D., Ceravolo, R., Binato, S., Salmaso, F., Zovato, S., Caliandro, A., Michielin, R. and Cartei, G. (2004) Brain natriuretic peptide: A new marker of car-  F. Zustovich et al. / Health 2 (2010) 376-380 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 380 diac ischemia in neoplastic patients during chemotherapy? Proceedings of the 15th International Congress on anti- cancer Treatment. [8] Trivellato, M., Zustovich, F., Zaninotto, M., Mion, M., Ceravolo, R., Pastorelli, Canton, R., Buratin, L., Calian- dro, A., Michielin, R., Plebani, M. and Cartei, G. (2005) Ischemia Modified Albumin (IMA), brain natriuretic peptide and chromogranin a after fluorouracil bolus in colo-rectal cancer patients. Proceedings of European So- ciety of Medical Oncology GI Symposium, Advances in Gastrointestinal Cancers. [9] Collinson, P.O., Gaze, D.C., Bainbridge, K., Morris, F., Morris, B., Price, A. and Goodacre, S. (2006) Utility of admission cardiac troponin and “Ischemia Modified Al- bumin” measurements for rapid evaluation and rule out of suspected acute myocardial infarction in the emer- gency department. Emergency Medicine Journal, 23, 256-261. [10] Omland, T., Dickstein, K. and Syversen, U. (2003) As- sociation between plasma chromogranin A concentration and long-term mortality after myocardial infarction. American Journal of Medicine, 114, 25-30. [11] Schnabel, R., Lubos, E., Rupprecht, H.J., Espinola-Klein, C., Bickel, C., Lackner, K.J., Cambien, F., Tiret, L., Munzel, T. and Blankenberg, S. (2006) B-type natriu- retic peptide and the risk of cardiovascular events and death in patients with stable angina: Results from the Athero Gene study. Journal of the American College of Cardiology, 47, 552-8. [12] Jemal, A., Murray, T., Samuels, A., Ghafoor, A., Ward, E. and Thun, M.J. (2003) Cancer statistics. CA Cancer Journal for Clinicians, 53, 5-26. [13] O’Connell, M.J., Maillard, J.A., Kahn, M.J., Macdonald, J.S., Haller, D.G., Mayer, R.J. and Wieand, H.S. (1997) Controlled trial of fluorouracil and low-dose leucovorin given for 6 months as postoperative adjuvant therapy for colon cancer. Journal of Clinical Oncology, 15, 246-50. [14] Boeyer, F.J.F., Osanto, S., Ritsema, van Eck, H.J., A.Q.M.J., van Steijn, Ballieux, B.E.P.B., Schoemaker, R.C., Cohen, A.F. and Burgraaf (2008) Evaluation of biomarkers for cardio toxicity of anthracyclin-based che- motherapy. Journal of Cancer Research and Clinical Oncology, 134, 961-968. |

