L. M. LAPALORCIA ET AL.483
Assessment of graft’s survival was verified on POD 5.
3. Discussion
Use of autologous chondrocutaneous graft from the
auricular region has been first described in the fifties by
Sathyanarayana Setty Pr et al. 12 in the sixties 13, in
the eighties 6,7 and in the nineties in a microvascular-
ized variant described by Pribaz and Tanaka 14,15.
Subsequently several applications have been used in
multiple reconstructive setting s such as reconstruction of
ear defects, alar rim, nasal tip, nasal lower third aesthetic
subunits 3-5 with f a v orable results f o r p at ie n ts .
Use of bilateral grafts approached medially to recon-
struct a complete dome in a burned patient has not been
described and the success of the graft was encouraging
for us and aesthetically and function ally effective for the
patient.
Minimal morbidity of the donor site for extensive fa-
cial grafting was encountered and no complications oc-
curred 10,11.
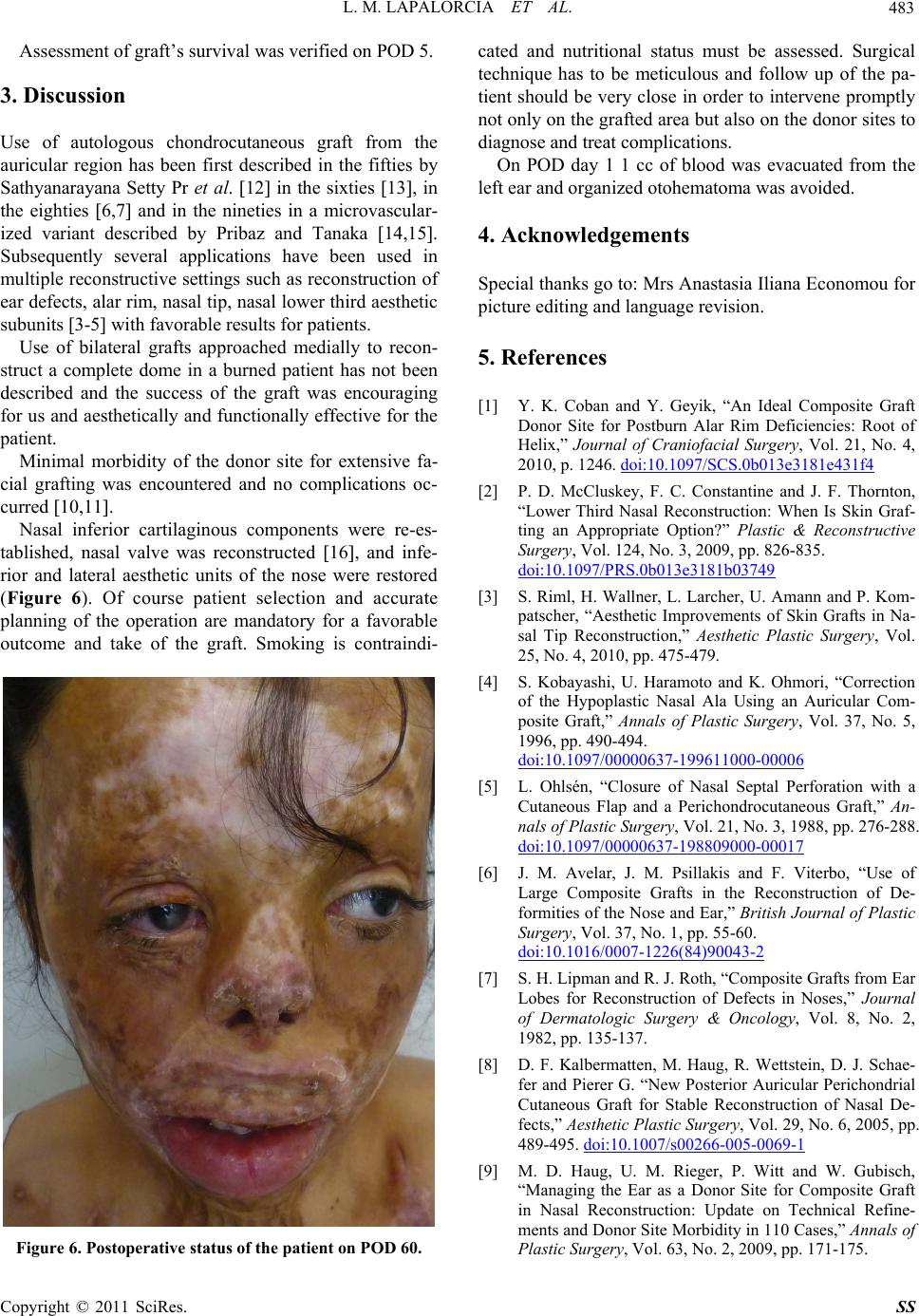
Nasal inferior cartilaginous components were re-es-
tablished, nasal valve was reconstructed 16, and infe-
rior and lateral aesthetic units of the nose were restored
(Figure 6). Of course patient selection and accurate
planning of the operation are mandatory for a favorable
outcome and take of the graft. Smoking is contraindi-
Figure 6. Postoperative status of the patient on POD 60.
cated and nutritional status must be assessed. Surgical
technique has to be meticulous and follow up of the pa-
tient should be very close in order to intervene promptly
not only on the grafted area but also on the donor sites to
diagnose and treat complications.
On POD day 1 1 cc of blood was evacuated from the
left ear and organized otohematoma was avoided.
4. Acknowledgements
Special thanks go to: Mrs Anastasia Iliana Eco nomou for
picture editing and language revision.
5. References
[1] Y. K. Coban and Y. Geyik, “An Ideal Composite Graft
Donor Site for Postburn Alar Rim Deficiencies: Root of
Helix,” Journal of Craniofacial Surgery, Vol. 21, No. 4,
2010, p. 1246. doi:10.1097/SCS.0b013e3181e431f4
[2] P. D. McCluskey, F. C. Constantine and J. F. Thornton,
“Lower Third Nasal Reconstruction: When Is Skin Graf-
ting an Appropriate Option?” Plastic & Reconstructive
Surgery, Vol. 124, No. 3, 2009, pp. 826-835.
doi:10.1097/PRS.0b013e3181b03749
[3] S. Riml, H. Wallner, L. Larcher, U. Amann and P. Kom-
patscher, “Aesthetic Improvements of Skin Grafts in Na-
sal Tip Reconstruction,” Aesthetic Plastic Surgery, Vol.
25, No. 4, 2010, pp. 475-479.
[4] S. Kobayashi, U. Haramoto and K. Ohmori, “Correction
of the Hypoplastic Nasal Ala Using an Auricular Com-
posite Graft,” Annals of Plastic Surgery, Vol. 37, No. 5,
1996, pp. 490-494.
doi:10.1097/00000637-199611000-00006
[5] L. Ohlsén, “Closure of Nasal Septal Perforation with a
Cutaneous Flap and a Perichondrocutaneous Graft,” An-
nals of Plastic Surgery, Vol. 21, No. 3, 1988, pp. 276-288.
doi:10.1097/00000637-198809000-00017
[6] J. M. Avelar, J. M. Psillakis and F. Viterbo, “Use of
Large Composite Grafts in the Reconstruction of De-
formities of the Nose and Ear,” British Journal of Plastic
Surgery, Vol. 37, No. 1, pp. 55-60.
doi:10.1016/0007-1226(84)90043-2
[7] S. H. Lipman and R. J. Roth, “Composite Grafts from Ear
Lobes for Reconstruction of Defects in Noses,” Journal
of Dermatologic Surgery & Oncology, Vol. 8, No. 2,
1982, pp. 135-137.
[8] D. F. Kalbermatten, M. Haug, R. Wettstein, D. J. Schae-
fer and Pierer G. “New Posterior Auricular Perichondrial
Cutaneous Graft for Stable Reconstruction of Nasal De-
fects,” Aesthetic Plastic Surgery, Vol. 29, No. 6, 2005, pp.
489-495. doi:10.1007/s00266-005-0069-1
[9] M. D. Haug, U. M. Rieger, P. Witt and W. Gubisch,
“Managing the Ear as a Donor Site for Composite Graft
in Nasal Reconstruction: Update on Technical Refine-
ments and Donor Site Morbidity in 110 Cases,” Annals of
Plastic Surgery, Vol. 63, No. 2, 2009, pp. 171-175.
Copyright © 2011 SciRes. SS