Paper Menu >>
Journal Menu >>
 Vol.2, No.4, 295-299 (2010) Health doi:10.4236/health.2010.24043 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Predicting maximum voluntary ventilation in normal healthy individuals using indirect inspiratory muscle strength measurements: a correlation study Rohit Sontakke1, Mangesh Deore2, Dhara Kothari3 1Masterskill University College of Health, Cheras, Malaysia; rohitrohits@yahoo.com 2Sancheti Institute of Orthopedics, Pune, India 3Nivara Physiotherapy Center, Pune, India Received 17 November 2009; revised 7 December 2009; accepted 15 December 2009. ABSTRACT Maximum Voluntary Ventilation (MVV), one of the components of Pulmonary Function Testing (PFT), has multiple uses. Various factors in- cluding the inspiratory muscle strength (IMS) influence it s magnitude. Our aim was to quantify the IMS indirectly using an economical and non invasive bedside assessment tool, determine its association with MVV and then develop a pre- dictive equation for MVV. 41 healthy non-athletic physical therapy students participated in the study. IMS measurement was performed with a sphygmomanometer. Average of the three net deflections in sphygmomanometer following deepest possible breaths was taken as indirect measurement of IMS in mm of Hg. MVV was measured according to ATS guidelines using a spirometer. Results from the data analysis re- vealed a significant correlation between IMS and MVV(r = 0.83, p < 0.001) and the coefficient of determination = 0.68. So, we developed a re- gression equation: Y = 1.9669(X) + 49.838 with SEE: 13.02L/min and ANOVA for the equation was (F=68.9, p < 0.001). Hence, it can be con- cluded that a strong correlation between the indirect IMS and MVV was established and a predictive equation to estimate MVV was de- veloped. This equation proved to have a high predictive value with a small error of estimation. This indicates that the value of the indirect IMS measurement obtained using the sphygmoma- nometer can be used to estimate MVV in normal healthy individuals without the use of a con- ventional spirometer. Keywords: Healthy Physical Therapy Students; Maximum Voluntary Ventilation; Inspiratory Muscle Strength; Regressio n Equation; Sp hygmomanom eter 1. INTRODUCTION Evidence-based support for pulmonary rehabilitation in the management of patients with chronic respiratory dys- function has grown tremendously, and this comprehen- sive intervention has clearly demonstrated to reduce dyspnea and health care costs, increase exercise per- formance, and improve health-related quality of life (HRQL) [1-6]. One of the factors responsible for exercise limitations and reduced HRQL in patients with respiratory disorders is dyspnea [7,8]. Weakness or mechanical inefficiency of the respiratory muscles results in a mismatch between central respiratory motor output and ach ieved ventilation . This mismatch can also explain the dyspnea experienced by patients with neuromuscular diseases affecting the respiratory musculature [9] and in patients with respira- tory muscle fatigue [10]. As the pressure-generating ca- pacity of the respiratory muscles falls and as the ratio of the pressures produced by the respiratory muscles to the maximum pressure that can be achieved increases dysp- nea progressively worsens [11]. Since there is an estab- lished association between respiratory muscle dysfunc- tion and dyspnea, an improvement in respiratory muscle function with inspiratory muscle training (IMT) could lead to a reduction in dyspnea [12,13]. A meta-analysis of IMT in 17 clinical trials found limited support for its use in terms of improving pulmonary function, respira- tory muscle strength and endurance, exercise capacity, and functional status in patients with COPD [14-16]. A consistent improvement in baseline d yspnea index (BDI) and transitional dyspnea index was shown following IMT [17]. Also, fewer dyspnea was reported by patients who used IMT with a threshold loading device at 30% of Pimax nevertheless, those who used either a very light load or sham treatments also reported less dyspnea [18]. Inspiratory muscle training has also been found to re- duce dyspnea during exertion not only in patients with respiratory ailments but also in normal healthy indiv idu- 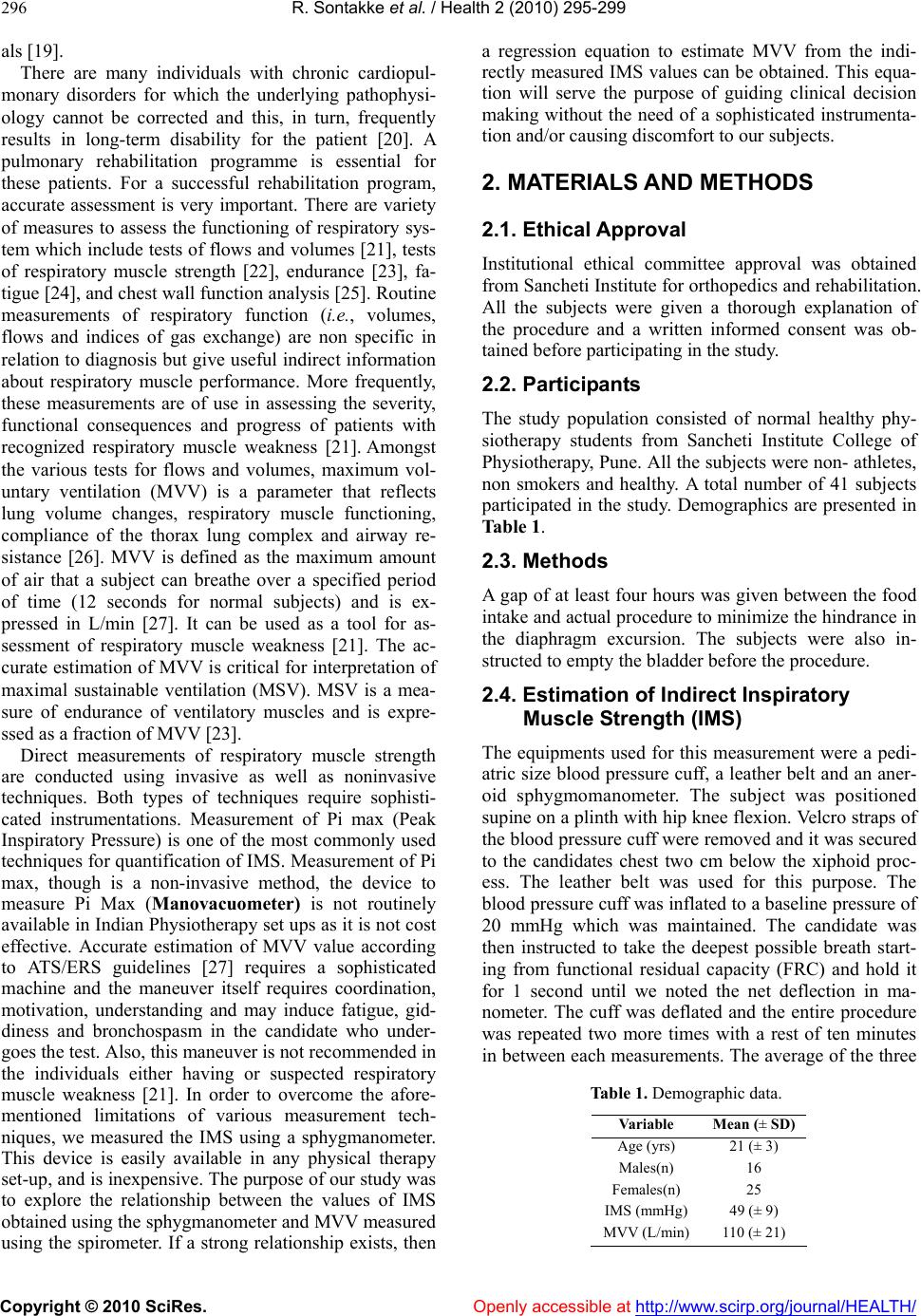 R. Sontakke et al. / Health 2 (2010) 295-299 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 296 als [19]. There are many individuals with chronic cardiopul- monary disorders for which the underlying pathophysi- ology cannot be corrected and this, in turn, frequently results in long-term disability for the patient [20]. A pulmonary rehabilitation programme is essential for these patients. For a successful rehabilitation program, accurate assessment is very important. There are variety of measures to assess the functioning of respiratory sys- tem which include tests of flows and volumes [21], tests of respiratory muscle strength [22], endurance [23], fa- tigue [24], and chest wall function analysis [25]. Routine measurements of respiratory function (i.e., volumes, flows and indices of gas exchange) are non specific in relation to diagnosis but give useful indirect information about respiratory muscle performance. More frequently, these measurements are of use in assessing the severity, functional consequences and progress of patients with recognized respiratory muscle weakness [21]. Amongst the various tests for flows and volumes, maximum vol- untary ventilation (MVV) is a parameter that reflects lung volume changes, respiratory muscle functioning, compliance of the thorax lung complex and airway re- sistance [26]. MVV is defined as the maximum amount of air that a subject can breathe over a specified period of time (12 seconds for normal subjects) and is ex- pressed in L/min [27]. It can be used as a tool for as- sessment of respiratory muscle weakness [21]. The ac- curate estimation of MVV is critical for interpretation of maximal sustainable ventilation (MSV). MSV is a mea- sure of endurance of ventilatory muscles and is expre- ssed as a fraction of MVV [23]. Direct measurements of respiratory muscle strength are conducted using invasive as well as noninvasive techniques. Both types of techniques require sophisti- cated instrumentations. Measurement of Pi max (Peak Inspiratory Pressure) is one of the most commonly used techniques for quantificatio n of IMS. Measurement of Pi max, though is a non-invasive method, the device to measure Pi Max (Manovacuometer) is not routinely available in Indian Physiotherapy set ups as it is not cost effective. Accurate estimation of MVV value according to ATS/ERS guidelines [27] requires a sophisticated machine and the maneuver itself requires coordination, motivation, understanding and may induce fatigue, gid- diness and bronchospasm in the candidate who under- goes the test. Also, this maneuver is not recommended in the individuals either having or suspected respiratory muscle weakness [21]. In order to overcome the afore- mentioned limitations of various measurement tech- niques, we measured the IMS using a sphygmanometer. This device is easily available in any physical therapy set-up, and is inexpensiv e. The purpose of our study was to explore the relationship between the values of IMS obtained using the sphygmanometer and MVV measured using the spirometer. If a strong relationship exists, then a regression equation to estimate MVV from the indi- rectly measured IMS values can be obtained. This equa- tion will serve the purpose of guiding clinical decision making without the need of a sophisticated instrumenta- tion and/or causing discomfort to our subjects. 2. MATERIALS AND METHODS 2.1. Ethical Approval Institutional ethical committee approval was obtained from Sancheti Institute for orthoped ics and rehabilitation . All the subjects were given a thorough explanation of the procedure and a written informed consent was ob- tained before participating in the study. 2.2. Participants The study population consisted of normal healthy phy- siotherapy students from Sancheti Institute College of Physiotherapy, Pune. All th e subjects were non- athletes, non smokers and healthy. A total number of 41 subjects participated in the study. Demographics are presented in Table 1. 2.3. Methods A gap of at least four hours was given between the food intake and actual procedure to minimize the hindrance in the diaphragm excursion. The subjects were also in- structed to empty the bladder before the procedure. 2.4. Estimation of Indirect Inspiratory Muscle Strength (IMS) The equipments used for this measurement were a pedi- atric size blood pressure cuff, a leather belt and an aner- oid sphygmomanometer. The subject was positioned supine on a plinth with hip knee flexion. Velcro straps of the blood pressure cuff were removed and it was secured to the candidates chest two cm below the xiphoid proc- ess. The leather belt was used for this purpose. The blood pressure cuff was inflated to a baseline pressure of 20 mmHg which was maintained. The candidate was then instructed to take the deepest possible breath start- ing from functional residual capacity (FRC) and hold it for 1 second until we noted the net deflection in ma- nometer. The cuff was deflated and the entire procedure was repeated two more times with a rest of ten minutes in between each measurements. The average of the three Table 1. Demographic data. Variable Mean (± SD) Age (yrs) 21 (± 3) Males(n) 16 Females(n) 25 IMS (mmHg)49 (± 9) MVV (L/min)110 (± 21) 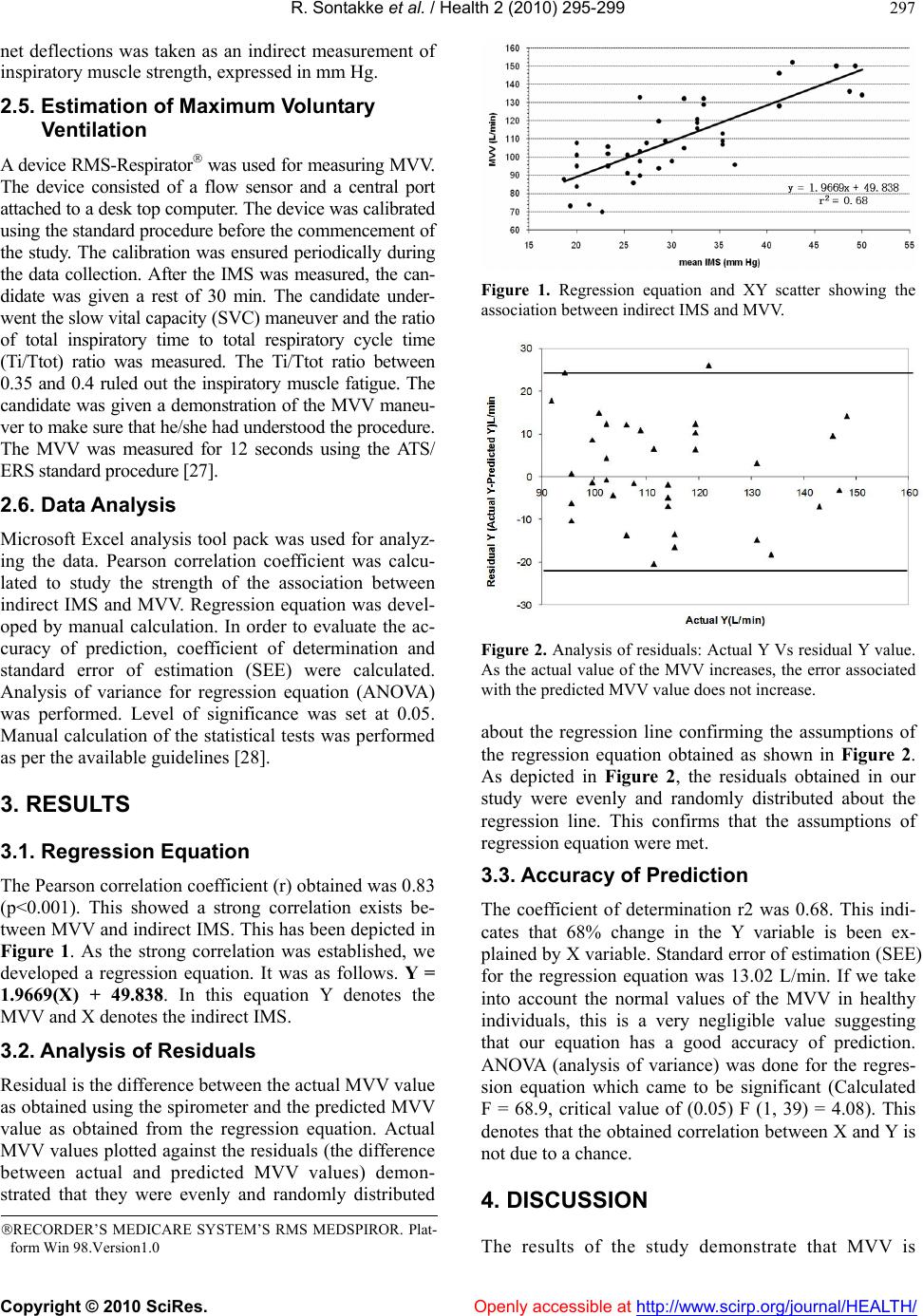 R. Sontakke et al. / Health 2 (2010) 295-299 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 297 net deflections was taken as an indirect measurement of inspiratory muscle strength, expressed in mm Hg. 2.5. Estimation of Maximum Voluntary Ventilation A device RMS-Resp irator was used for measuring MVV. The device consisted of a flow sensor and a central port attached to a desk top computer. The device was calibrated using the standard procedure before the commencement of the study. The calibration was ensured periodically during the data collection. After the IMS was measured, the can- didate was given a rest of 30 min. The candidate under- went the slow vital capacity (SVC) maneuver and the ratio of total inspiratory time to total respiratory cycle time (Ti/Ttot) ratio was measured. The Ti/Ttot ratio between 0.35 and 0.4 ruled out the inspiratory muscle fatigue. The candidate was given a demonstration of the MVV maneu- ver to make sure that he/she had understood the procedure. The MVV was measured for 12 seconds using the ATS/ ERS standard procedure [27]. 2.6. Data Analysis Microsoft Excel analysis tool pack was used for analyz- ing the data. Pearson correlation coefficient was calcu- lated to study the strength of the association between indirect IMS and MVV. Regression equation was devel- oped by manual calculation. In order to evaluate the ac- curacy of prediction, coefficient of determination and standard error of estimation (SEE) were calculated. Analysis of variance for regression equation (ANOVA) was performed. Level of significance was set at 0.05. Manual calculation of the statistical tests was performed as per the available guidelines [28]. 3. RESULTS 3.1. Regression Equation The Pearson correlation coefficient (r) obtained was 0.83 (p<0.001). This showed a strong correlation exists be- tween MVV and indirect IMS. This has been depicted in Figure 1. As the strong correlation was established, we developed a regression equation. It was as follows. Y = 1.9669(X) + 49.838. In this equation Y denotes the MVV and X denotes the indirect IMS. 3.2. Analysis of Residuals Residual is the difference between the actual MVV value as obtained using the sp irometer and the predicted MVV value as obtained from the regression equation. Actual MVV values plotted against the residuals (the difference between actual and predicted MVV values) demon- strated that they were evenly and randomly distributed Figure 1. Regression equation and XY scatter showing the association between indirect IMS and MVV. Figure 2. Analysis of residuals: Actual Y Vs residual Y value. As the actual value of the MVV increases, the error associated with the predicted MVV value does not increase. about the regression line confirming the assumptions of the regression equation obtained as shown in Figure 2. As depicted in Figure 2, the residuals obtained in our study were evenly and randomly distributed about the regression line. This confirms that the assumptions of regression equation were met. 3.3. Accuracy of Prediction The coefficient of determination r2 was 0.68. This indi- cates that 68% change in the Y variable is been ex- plained by X variable. Standard error of estimation (SEE) for the regression equation was 13.02 L/min. If we take into account the normal values of the MVV in healthy individuals, this is a very negligible value suggesting that our equation has a good accuracy of prediction. ANOVA (analysis of variance) was done for the regres- sion equation which came to be significant (Calculated F = 68.9, critical value of (0.05) F (1, 39) = 4.08). This denotes that the obtained correlation between X and Y is not due to a chance. 4. DISCUSSION The results of the study demonstrate that MVV is RECORDER’S MEDICARE SYSTEM’S RMS MEDSPIROR. Plat- form Win 98.Version1.0  R. Sontakke et al. / Health 2 (2010) 295-299 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 298 strongly correlated with the indirect IMS and MVV can be predicted with a good accuracy using the indirect IMS in a group of normal healthy college students. In addition, the prediction equation has proved to have ex- cellent validity when ANOVA and analysis of the re- siduals was done. Coefficient of determination of 0.68 suggests that 68% of the variance in MVV can be ex- plained by variance in IMS. This is because in addition to IMS, expiratory muscle strength, complian ce of lungs and chest wall, airway resistance also contributes to MVV [ 2 6] . Peak inspiratory pressure (Pi Max) is one of the sim- plest and commonly u sed tool that is used for quantifica- tion of IMS. But, this device is not routinely av ailable in physical therapy set ups in India. Due to this reason we chose to quantify the IMS indirectly instead of using Pi max. The reasons for trying to quantify the indirect IMS and then predicting MVV from it are multiple. Patients could possibly save time, expenses, and invasive proce- dures if an accurate prediction of their maximum volun- tary ventilation could be made from their indirect IMS. A common equation used for MVV estimation is MVV = 35.0 × FEV1. The usefulness of this equation has been established in predicting MVV, in American African girls [29]. This method may underestimate the maximum exercise ventilation in COPD patients [31] Also, this equation requires the actual value of FEV1 to be substi- tuted which can be obtained only with the use of a spi- rometer. In contrast to, these limitations, our study en- ables the clinicians to estimate the MVV using the re- gression equation which requires IMS value which can be obtained without the need of a spirometer or any other complicated device. Applicability of Caucasian regression equations was also studied on Indian population for prediction of forced vital capacity (FVC), forced expiratory volume in first second (FEV 1) [31]. The conclusion of this study was that the commonly used Caucasian prediction equa- tions, or a fixed percentage of their predicted values, were leading to the improper interpretation of the data obtained; that is, there was a significant difference be- tween the values obtained using the equation and the values obtained by actual performing the maneuver. This happened in a significant proportion of patients and the study reflected that there is a need to assess performance of more than one regression equation before choosing any single prediction equation in Indian population as the most important step in diagnosing abnormality of lung function in individuals is to define whether they are within or out side the healthy subjects range. Though in this study it was the vital capacity (VC) which was stud- ied, we can still expect that we can apply the conclusions from this study to the MVV also as VC is been found to have proportionate reductions to MVV [21]. None of these studies which studied the predictive equations for MVV had focused on the direct or indirect IMS measurement. Also the studies which focus on IMS have used the devices which are still expensive in India and not routinely available in Indian Physiotherapy set ups. Our technique of estimating IMS was inexpensive, non invasive, uncomplicated and can be used in any small clinical set up and also in ambulatory care set up. Thus, our study overcomes the previously mentioned drawbacks of the techniques for quantification of IMS and MVV in Indian set up. Here, it was the chest expan- sion that is, overall chest wall movement that was used for assessment of IMS. Throughout the study it was taken into account that the changes in the intrathoracic blood volume could have resulted in the difference be- tween actual lung volume change and change in the volume of the thorax or simply the chest expansion. But this difference being negligible has not influenced our results [25]. This means that the chest wall motion has reflected the volume changes occurring in the lungs during breathing as there in no disparity between volume changes in the lungs and volume changes of the thoracic wall. One more confounding factor can be the elasticity of the chest wall tissues. But, it has been shown that the tissues of the chest wall being essentially in compressible, volume changes of the chest wall surface are nearly equal to volume changes of the lungs and can be used for indirect measure of IMS [25]. Regression equation will be useful only when the IMS value lies between 18.67 mm Hg to 50 mm Hg and for the age gro up of 18 to 24 yrs. The quantification indirect inspiratory muscle strength needs to be studied in wider age range and dis- eased population to increase its clinical applicability. Also, the contribution of expiratory muscle strength to MVV was not taken into account. Along with this, reli- ability and validly of this new tool for evaluating IMS needs to be studied. 5. CONCLUSIONS A strong correlation between the indirect IMS and MVV was established. A regression equation was developed. This equation was tested for its ability to accurately pre- dict the MVV and it proved to have a high predictive value with a small error of estimation. Th is signifies that by substituting the value of the indirect IMS in the ob- tained equation, we can estimate MVV in normal healthy individuals. This prediction will have a good accuracy. REFERENCES [1] Von Leupoldt, A., Hahn, E., Taube, K., Schubert-Heu- keshoven, S., Magnussen and H., Dahme, B. (2008) Ef- fects of 3-week outpatient pulmonary rehabilitation on exercise capacity, dyspnea, and quality of life in COPD.  R. Sontakke et al. / Health 2 (2010) 295-299 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 299 Lung, 186(6), 387-391. [2] Güell, R., Resqueti, V., Sangenis, M., Morante, F., Martorell, B., Casan, P., et al. (2006) Impact of pulmo- nary rehabilitation on psychosocial morbidity in patients with severe COPD. Chest, 129(4), 899-904. [3] Verrill, D., Barton, C., Beasley, W. and Lippard, W.M. (2005) The effects of short-term and long-term pulmo- nary rehabilitation on functional capacity, perceived dyspnea, and quality of life. Chest, 128(2), 673-683. [4] Cecins, N., Geelhoed, E. and Jenkins, S.C. (2008) Re- duction in hospitalization following pulmonary rehabili- tation in patients with COPD. Australian Health Review, 32(3), 415-422. [5] Kyung, K.A. and Chin, P.A. (2008) The effect of a pul- monary rehabilitation programme on older patients with chronic pulmonary disease. Journal of Clinical Nursing, 17(1), 118-125. [6] Hui, K.P., Alison, B. and Hewitt, A.B. (2003) Simple pul- monary rehabilitation program improves health outcomes and reduces hospital Utilization in patients with COPD. Chest, 124, 94-97. [7] Nici, L., Donner, C., Wouters, E., Zuwallack, R., Am- brosino, N., Bourbeau, J., et al. (2006) American thoracic society/European respiratory society statement on pul- monary rehabilitation. American Journal of Respiratory and Critical Care Medicine, 173, 390-1413. [8] Hill, K., Jenkins, S.C., Hillman, D.R. and Eastwood, P.R. (2004) Dyspnea in COPD: Can inspiratory muscle train- ing help? Australian Journal of Physiotherapy, 50(3), 169-180. [9] Rochester, D. (1993) Respiratory muscles and ventilatory failure. American Journal of Medical Science, 305, 394- 402. [10] Altose, M.D. (1992) Respiratory muscles and dyspnea. Seminars in Respiratory Medicine, 13, 1-6. [11] Killian, K.J. and Jones, N.L. (1988) Respiratory muscles and dyspnea. Clinics in Chest Medicine, 9, 237-248. [12] Weiner, P., Magadle, R., Beckerman, M., Weiner, M. and Berar-Yanay, N. (2004) Maintenance of inspiratory mus- cle training in COPD patients: One year follow-up. European Respiratory Journal, 23(1) , 61-65. [13] Battaglia, E., Fulgenzi, A., Bernucci, S., Giardini, M.E. and Fererro, M.E. (2006) Home respiratory muscle training in patients with chronic obstructive pulmonary disease. Respirology. 11(6), 799-804. [14] Smith, L., Cook, D., Guyatt, G., Madhavan, J. and Ox- man, A. (1992) Respiratory muscle training in chronic airflow limitation: 8 meta-analyses. American Review of Respiratory Disease, 145, 533-539. [15] Padula, C.A. and Yeaw, E. (2006) Inspiratory muscle training: Integrative review. Research and Theory for Nursing Practice, 20(4), 291-304. [16] Lötters, F., van Tol, B., Kwakkel, G. and Gosselink, R. (2002) Effects of controlled inspiratory muscle training in patients with COPD: A meta-analysis. European Res- piratory Journal, 20(3), 570-576. [17] Harver, A., Mahler, D.A. and Daubenspeck, J.A. (1989) Targeted inspiratory muscle training improves respiratory muscle function and reduces dyspnea in chronic obstruc- tive pulmonary disease. Annals of Internal Medicine, 11 1, 117-124. [18] Kim, M., Larson, J., Covey, M., Vitalo, C., Alex, C. and Patel, M. (1993) Inspiratory muscle training in patients with chronic obstructive pulmonary disease. Nursing Research, 42, 356-362. [19] McConnell, A.K. and Romer, L.M. (2004) Dyspnoea in health and obstructive pulmonary disease: The role of respiratory muscle function and training. Sports Medi- cine, 34(2), 117-132. [20] American Thoracic Society. (1999) Dyspnea: Assessment, mechanism and management: A consensus statement. American Journal of Respiratory and Critical Care Medicine, 159, 321-340. [21] Gibson, G.J., Whitelaw, W. and Nikolaos, S.N. (2002) Tests of over all respiratory function. ATS/ERS state- ment on respiratory muscle testing. American Journal of Respiratory and Critical Care Medicine, 166, 521-526. [22] Green, M., Road, J. and Sieck, G.C. (2002) ATS/ERS statement on respiratory muscle testing. American Jour- nal of Respiratory and Critical Care Medicine, 166, 528-542. [23] Clanton, T., Calverly, P.M. and Celli, B.R. (2002) Tests of respiratory muscle endurance. ATS/ERS statement on respiratory muscle testing. American Journal of Respi- ratory and Critical Care Medicine, 166, 559-569. [24] Supinski, G.S., Fitting, J.W. and Bellemare, F. (2002) Assessment of Respiratory Muscle fatigue. ATS/ERS statement on respiratory muscle testing. American Jour- nal of Respiratory and Critical Care Medicine, 166, 571-578. [25] Loring, S.H., Troyer, A. and Grassino, A,E. (2002) As- sessment of Chest Wall Function. ATS/ERS statement on respiratory muscle testing. American Journal of Respi- ratory and Critical Care Medicine, 166, 580-586. [26] Sheldon, R.L. (2000) Pulmonary Function Testing. In Wilkins, R.L., Krider, Susan, J., Clinical assessment in respiratory care. 4th Edition, Mosby, St. Louis, 141-160. [27] Millre, M.R., Hankinson, J. and Brusasco, V. (2005) Maximum voluntary ventilation. Standardisation of spi- rometry: SERIES ‘‘ATS/ERS task force: Standardization of lung function testing’’. European Respiratory Journal, 26, 331-334. [28] Portney, L.G. and Watkins, M.P. (2009) Foundations of clinical research applications to practice. 3rd Editon, Prentice Hall, New Jersey, 539-567. [29] Fulton, J.E., Pivarnik, J.M., Taylor, W.C., Snider, S.A., Tate, A.L. and Frankowski, R.F. (1995) Prediction of ma- ximum voluntary ventilation (MVV) in African-Ameri- can adolescent girls. Pediatric Pulmonology, 20(4), 225- 233. [30] Pride, N.B. (2001) Tests of forced inspiration and expira- tion. Clinics in Chest Medicine, 22(4), 599-622. [31] Aggarwal, A.N., Gupta, D., Behera, D. and Jindal, S.K. (2005) Applicability of commonly used Caucasian pre- diction equations for spirometry interpretation in India. Indian Journal of Medical Research, 122(2), 153-164. |

