Health
Vol. 4 No. 8 (2012) , Article ID: 22007 , 4 pages DOI:10.4236/health.2012.48085
Clinical critics in the management of diabetes mellitus*
![]()
1School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia;
#Corresponding Author: wasifgillani@gmail.com
2Hospital Pulau Pinang, Penang, Malaysia
3Ziauddin College of Pharmacy, Ziauddin University, Karachi, Pakistan
4Pharmacy Department, Hospital Universiti Sains Malaysia, Kota Bharu, Malaysia
Received 11 May 2012; revised 14 June 2012; accepted 21 June 2012
Keywords: diabetes mellitus; self-care practices; glycaemic control; management of DM
ABSTRACT
There is a global epidemic of diabetes with its prevalence expected to increase from 5.1% in 2003 to 6.3% in 2025. This increase in diabetes is occurring in all nations, however, developing nations are particularly at risk. It spares no group and affects men, women, the elderly, young and people from very racial and socioeconomic background. Nevertheless, certain ethnic groups including Asians are affected more than Caucasians. Large randomized clinical trials have shown that improvement in glycaemic control, together with management of diabetes-related risk factors like blood pressure and lipid control significantly reduce the micro and macro complications in individuals with type 1 and type 2 diabetes. Patient education plays a crucial role in the prevention of diabetic fool problems. In Geneva, the rate of lower limb amputations was reduced by almost 75% after an educational intervention. People with diabetes must acquire the knowledge and skills through education to provide daily self-care in diabetes management which involves maintenance of healthy living, recognition and management of diabetes problems when they arise and taking preventive measures. Some factors include patients’ biomedical variables, the psychosocial environment, the knowledge, attitudes and beliefs of patients themselves, home careers and health care providers, healthcare systems’ accessibility and availability and even the national political context may influence these self-care behaviors.
1. INTRODUCTION
Diabetes is a chronic progressive metabolic disease characterized by hyperglycemia due mainly to absolute insulin insufficiency (type 1 diabetes) or relative insulin deficiency and insulin resistance (type 2 diabetes). Partly due to the metabolic perturbations caused by hyperglycemia, diabetes affects virtually every system of the body with long term and severe damage if diabetes control over time proves to be suboptimal [1].
1.1. How Common Is Diabetes?
There is a global epidemic of diabetes with its prevalence expected to increase from 5.1% in 2003 to 6.3% in 2025. This increase in diabetes is occurring in all nations, however, developing nations are particularly at risk. It spares no group and affects men, women, the elderly, young and people from very racial and socio-economic background. Nevertheless, certain ethnic groups including Asians are affected more than Caucasians. Nearly half of all diabetes cases occur in people older than 65 years of age [2-4].
Although type 2 diabetes is predominantly a disease of adults, during the last few decades, the number of type 2 diabetes children and adolescents has increased globally and particularly in some parts of the Asian-Pacific regions. In some countries in these regions, type 2 diabetes in the young outnumbers type 1 diabetes by a ratio of 4:1 [5,6].
1.2. What Are the Chronic Complications of Diabetes?
These are two categories of vascular complications in diabetes: microvascular (retinopathy, nephropathy and neuropathy) and macrovascular: coronary heart disease (CHD), cereberovascular disease (CVD) and peripheral vascular disease (PVD).
1.3. Can Microvascular Complications of Diabetes Be Reduced?
Large randomized clinical trials have shown that improvement in glycaemic control, together with management of diabetes-related risk factors like blood pressure and lipid control significantly reduce the micro and macro complications in individuals with type 1 and type 2 diabetes. These trials demonstrated that for every 1% absolute reduction in glycated haemoglobin, microvascular complications fell by 30% - 35% and macrovascular complications by 14% - 16% as shown in table below [7-9].
1.4. Can Macrovascular Complications Be Reduced in Diabetes?
Patient education plays a crucial role in the prevention of diabetic fool problems. In Geneva, the rate of lower limb amputations was reduced by almost 75% after an educational intervention [10]. In another study of 242 type 2 diabetic patients, there were fewer recurrences of ulcers and the healing process was faster in subjects adhering to the foot care advice, when compared to those who did not follow the advice [11] (Table 1). However, there is no convincing evidence based on randomized clinical trials but improving glycaemic control can decrease CHD/CVD morbidity and mortality as shown in table below [12-14]. The evidence is largely based on epidemiological studies that 1% increase of A1c is associated with a 15% - 18% increase in the relative risk of CVD for patients with type 1 and type 2 diabetes [15]. Whereas lowering hypertension has been shown to decrease morbidity and mortality associated with CHD and CVD [16,17]. Many clinical trials report decrease morbidity and mortality due to CHD in people with diabetes when their dyslipidemia (high LDL cholesterol or lower HDL cholesterol) is treated [18,19]. In the management of dyslipidemia and hypertension, patient education leading to self-care can play a critical role.
1.5. Diabetes Currents
Diabetes mellitus is a chronic disease that requires lifelong medical treatment and lifestyle adjustments. The main treatment goals are to prevent or minimize the acute and chronic complications of diabetes, the challenge is to delay their progression. This lifelong need to manage diabetes is challenging and daunting for people who have to manage their disease alone or with family members for more than 95% of their life span. Not only are they
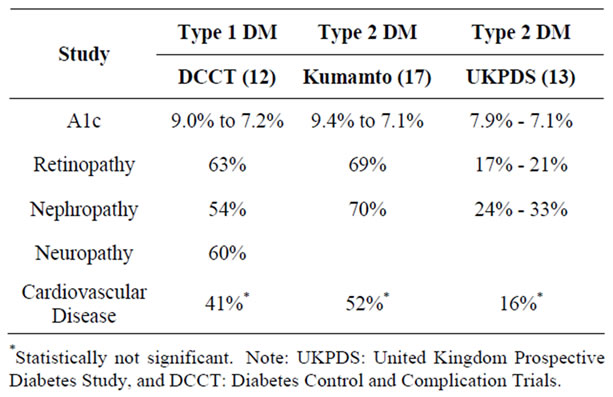
Table 1. Diabetes related disease co morbidities and associated preva-lence.
required to adhere to their lifelong daily medication intake but also lifelong lifestyle adjustment. Individuals with diabetes need to follow their meal plans daily, to lose weight if they are overweight or obese, and engage in appropriate physical activity, monitor their blood glucose levels regularly, if not daily. They also need to make decisions regarding the adjustment of diet, physical activity level or medication if necessary, to avoid hypoglycemia or hyperglycemia and perform daily foot care and quiet smoking if they are current smokers.
1.6. Diabetes Self-Care/Self-Management
People with diabetes must acquire the knowledge and skills through education to provide daily self-care in diabetes management which involves maintenance of healthy living, recognition and management of diabetes problems when they arise and taking preventive measures. To complicate self-care in diabetes management, the relationship between self-care and clinical outcomes are constantly influences by multiple factors in figure given below. These factors include patients’ biomedical variables, the psychosocial environment, the knowledge, attitudes and beliefs of patients themselves, home careers and health care providers, healthcare systems’ accessibility and availability and even the national political context may influence these self-care behaviors (Figure 1).
Although self-care plays a vital role in successful diabetes management, most people with diabetes do not have the advantage of having continuous assistance and supervision from health professionals such as during the DCCT or UKPDS trials. Instead they spend more than 95% of their life outside their doctors’ office to manage their self-care [20,21] Helme (2004) and Legman (2005) found that only 7% to 25% of people with diabetes fully adhered to all aspects of the regimen [22,23]. Previous researchers reported that 40% - 60% of people with diabetes failed to comply with diet [24,25]. The frequency of non-adherence to glucose monitoring ranged from 30% - 80% and non-adherence to exercise programmes was as high as 70% - 80% [24,26-28]. Hence people with diabetes, their family members, and careers need to thoroughly understand the goals of diabetes management in order to successfully carry out the complex management strategies. It is important for health professionals to understand the factors that influence the self-care behaviors (dietary and medication intake, physical activity and PHCP) of people with diabetes.
1.7. Role of Diabetes Education in Treatment
The knowledge and skills needed for good self-care are acquired through diabetes education. Patient education has transformed and reinvented itself many times since its origins as early as Zulus Cornelius Celsius (25 BC to 50 AD) who promoted exercise and exhorted “people with diabetes should try to be his own doctor”. In 1921, Dr. Elliott Joslin from the Joslin Clinic in United States was one of the first physicians to start diabetes education and emphasized to his patients the importance of monitoring urine glucose at home [29].
Since then the traditional approach to diabetes was for the healthcare professionals to teach people with diabetes about the disease and do demonstrate the skills necessary to monitor the condition and administer their own medications. This traditional diabetes education focuses on the transfer of information which often does not result in the desired change in behavior or clinical outcomes [30,31]. This reflects a gap between what is being taught and what is being practiced by people with diabetes. To be effective, health professionals must change their approach to influence the self-care behavior of people with diabetes.
As discussed before, self-care in diabetes is constantly influenced by psychosocial, cultural beliefs and attitude of people with diabetes and their careers. To attain successful treatment, people with diabetes have to plan strategies, set goals, implement treatment plans and motivate themselves to continue this life-long process. Hence the American association of diabetes educators and the Australian diabetes educators association have advocated that diabetes self-management education involving daily
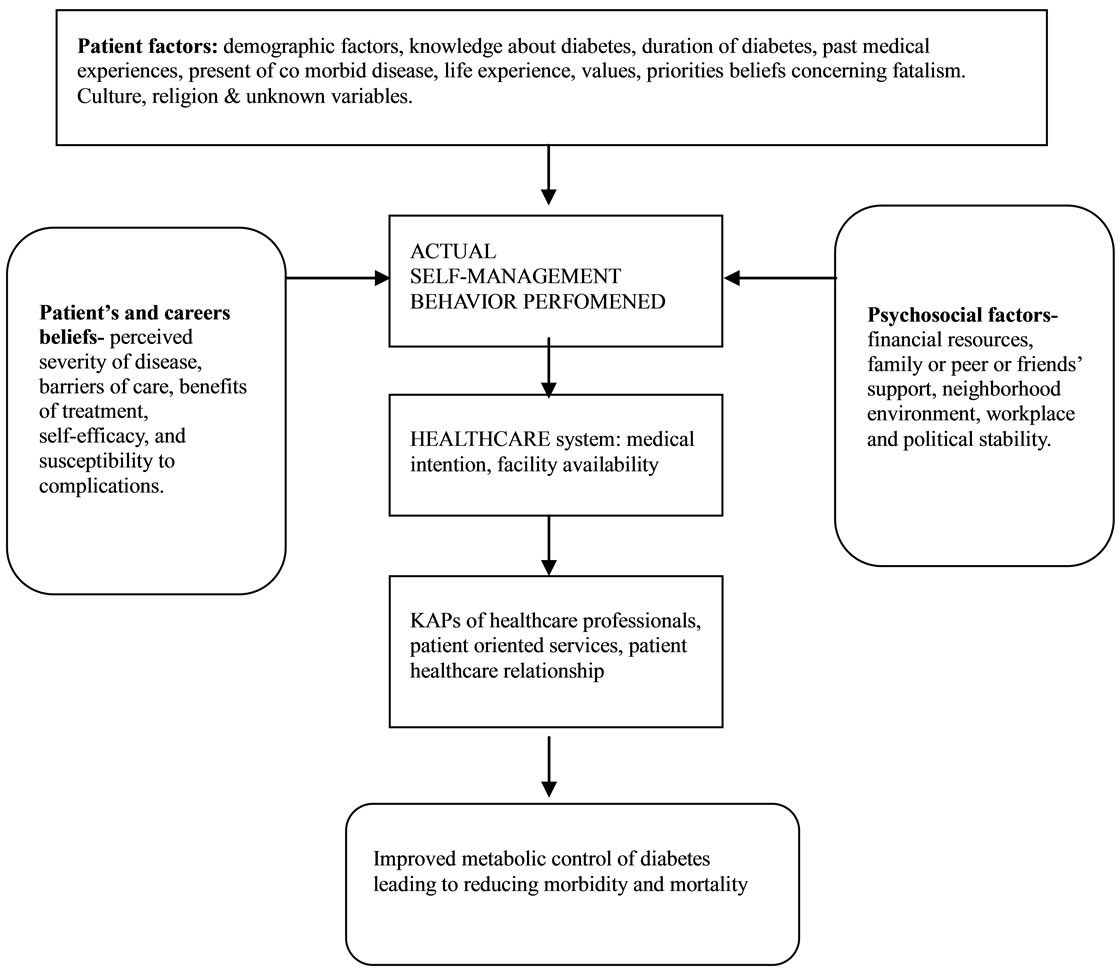
Figure 1. Factors associated to maintain diabetes tolerance.
medication and dietary intake, SMBG and physical exercise is insufficient. People with diabetes should also be taught problem-solving skills, setting goals and practicing risk reduction behavior by applying behavioral theory [32,33].
Since 1980s many behavior science theories had been incorporated in the management of diabetes and diabetes education such as empowerment, Locus of Control, the Health Belief Model and self-efficacy.
2. ADVANCES IN THE SELF-CARE PRACTICES
2.1. Significance of Self Care in Diabetes Management
The results of the diabetes control and complication trials (DCCT) and the United kingdom prospective diabetes study (UKPDS) had shown that individual who adhere to daily self-care of diabetes followed a meal plan, take medication as prescribed, exercise regularly and monitor their blood glucose levels usually achieved better shortand long-term health outcomes [34,35]. This is because more than 95% of diabetes self-care tasks involved the individuals with diabetes and/or their family members [36,37].
Despite positive outcomes from self-care interventions, the incidence and prevalence of low adherence to self-care in diabetes management has not changed over the decades. Several possible explanations have been explored. The process of self-care for diabetes is different from acute illness because it involves both maintenance and management. Besides maintaining daily self-care as previously discussed, the management phase requires individuals with diabetes to recognize sign or symptoms of diabetes complications, respond and treat symptoms, evaluate and monitor the effectiveness of the chosen treatment [38].
It is necessary to integrate all these behavioral tasks into a person’s daily routine which is constantly influenced by available resources, priorities, social responsibilities, health literacy and level of autonomy [39-42]. However, the beneficial clinical outcomes of diabetes self-care practices are not seen immediately. This is unlike arthritis, where self-care improves daily function and quality of life thus increasing the adherence rate [43]. Furthermore compared with self-care management of asthma, hypertension or heart failure, self-care practices in diabetes are more numerous, complex, involving lifestyle changes, expensive in term of self-monitoring blood glucose (SMBG) and restrictive especially in dietary selfcare [44-47].
To do diabetes self-care in daily life, diabetes knowledge is necessary. Studies of British Pakistani women and illiterate patients have indicated a gradient of improved diabetes knowledge with better self-care and glycaemic control [48,49]. Other researchers reported knowledge explained 16% - 17% of the variance in HbA1c [50-52]. In contrast, some researchers have reported increased diabetes knowledge correlated with poorer self-care and glycaemic control [53,54]. One possible explanation was that patients with greater access to education were also those with longer duration and advances complications.
2.2. Dietary Self-Care
Dietary glucose from carbohydrates contributes to the prevailing blood glucose level. Nutritional intervention improves glycaemic control of individuals with diabetes [55-57]. Subjects with the lowest dietary adherence had the poorest glycaemic control [58,59]. Additionally, lifestyle modifications (nutritional and exercise interventions) reduce diabetes complications by improving cardiovascular risk factors like hypertension, dyslipidemia and weight reduction [60-63].
2.3. Prevalence of Dietary Adherence
Researchers in the United States, Europe and Asia reported that 40% - 90% of individuals with diabetes had received dietary education. However across these continents less than 40% of both type 1 and type 2 diabetes patients followed strict dietary requirements and 10% - 25% did not follow any meal plan. The majority sought to balance their dietary habits with some recommendations. This illustrates the widespread difficulty in adhering to dietary recommendations and the discrepancy between diabetes knowledge and self-care practices [64-70]. It also implies other factors influence dietary behavior.
2.4. Confounder to Dietary Adherence
Several researchers have reported that some women with diabetes were more obsessed with food and practices binge-eating when experiencing times of depression [59,71]. Furthermore the multiple care roles that women accept requires them to balance their personal needs with those of the family resulted in less adherence to dietary habit [59,72,73]. A study with predominantly male subjects supported the above findings, with its subjects listing emotional factor and food craving as minimal dietary barriers [74]. In contrast the results of another male dominated study (n = 242) indicated an association between dietary non-adherence and depression, but the findings was not statistically significant [58].
Some studies have reported that there is no gender difference in dietary adherence. It is postulated that female subjects with better family and social support are able to follow the recommend diet [59,62,72,75-77]. Another study that used both survey and focus group interviews to assess the association of family support and dietary adherence reported significant findings from focus group interviews, but not survey. However, it was clear whether both the survey and focus group subjects were from the same study population [74].
Several other researchers also reported that age was inversely associated with poor dietary adherence with no cause inferred due to study design limitations [58,65, 66,76]. Irregular meal patterns and lack of consistency of day-to-day carbohydrates intake in conventional diabetes regimens contribute to poor glycaemic control [56,78]. Thus rigid meal schedules with lack of self-efficacy in time management of meal schedule during working and social hours pose dietary problems especially among the younger subjects [58,74,76,79].
High prevalence of depression also reported amongst the diabetic population globally. Subjects who were depressed had problems with acceptance of diabetes. They considered self-care to be a low priority resulting in little dietary adherence leading to poor metabolic control [59, 66,71,80-82].
While evaluation of physician-patient relationship, findings reported its contribution to dietary adherence through increased understanding and satisfaction [80,83]. This findings is supported by other studies that have observed a positive association between poor physicianpatient relationship and dietary non-adherence behavior [69,74,77]. Beside exercise and medication regimen cultural influences also dietary adherence also identified by Sherman and colleagues in 2000 [80]. Prior eating practices has been shown to be a strong indicator of dietary behavior [69,77].
2.5. Physical Activity
Physical activity increases glucose utilization in muscles and fats and thereby influencing the prevailing blood glucose level [84]. In people with diabetes (type 1 and type 2), regular aerobic exercise has been shown to improve glycaemic control, reduce cardiovascular risk factors, weight reduction and improve general well-being [85-87]. A recent geriatric fitness program for diabetes over 65 years of age showed reduced mortality over a 10-year period. However, the small sample size and supervised research setting limit the generalization of these findings to other clinical settings [88].
2.6. Confounders for Physical Activity Self-Care
Predictors for inactivity include negative attitude towards exercise like physical discomfort or illness, lack of family and social support, lack of confidence and time, depression and environmental barriers [89-92]. These findings’ validity is supported by researchers who also reported that self-efficacy and family supports are important predictors for performing physical exercise [76, 93-96]. Another survey (n = 375) reported that only 38% of the subjects were given advice by their healthcare providers on exercise in comparison to 90% being advised on diet and weight loss. Lack of direct comparison between perceived advice and actual advice received weaken the validity of this findings [97].
Studies on Pakistanis and Indians with type 2 diabetes in the United Kingdom have highlighted other social a cultural barriers to exercise self-care amongst Pakistani and Indian families. Taking time out to exercise could be interpreted as selfish and culturally inappropriate act. Many women in the study also found it difficult to increase their physical activities due to lack of socialization skills and culturally sensitive exercise facilities [73].
Demographic factors reported mixed results as determinants of exercise. Several studies found younger subjects exercise more than older subjects [93,98-101]. Plontikoff and colleagues in 2000 reported no significance difference between age groups. However 90% of their study subjects (n = 69) were under 55 years of age [95]. Lower socio-economic status was found to have significant association with inactivity in studies reported by Nelson and colleagues in 2002 but not by Hays and Clark in 1999. Seventy-eight percent of the subjects in Hays and Clark’s study were socio-economically poor in comparison with 20% of subjects in Nelso et al. [68,93]. Several other studies using the survey approach found women exercised less then men. This could be due to assessment bias as only leisure activities instead of total daily activities were measures [68,79,93,98].
Some studies found ethnicity correlated to level of physical activity [44,73,102-104]. These studies showed lower levels of physical activities and fitness among diabetic and non-diabetic Asian populations compare to the general or Caucasian population. Although the sizes of the different reports varied across studies, they were broadly consistent and not related to method of measurement. No reason was stated due to observational design.
2.7. Medication Intake
People with diabetes, depending on the anti-hyperglycemic medication prescribed, different medications reduce the blood glucose level via different mechanisms. For example, metformin primarily decrease insulin resistance and increase utilization of glucose in muscles and fats. Insulin and sulphonlyurease increase insulin secretion and decrease hepatic glucose production and increase glucose utilization. Alpha glucosidase inhibitors slow the digestion of complex carbohydrate and delay their absorption. Adherence of medication intake therefore can influence the prevailing blood glucose in many ways.
2.7.1. Correlates of Medication Adherence and Glycaemic Control
Literature found no association between medication adherence and Hb1Ac reduction [105,106]. In recent years, both prospective and retrospective studies had shown significantly better adherence to glycaemic control (p < 0.05) regardless negative findings in earlier studies were probably due to small study population samples and shorter follow-up period of less than 24 weeks compared to the later findings [107]. Despite these known consequences, adherence rates have remained unchanged since the 1970s which means that exploring other factors concerning medication adherence is justified.
2.7.2. Factors to Medication Adherence
Most patients with type 2 diabetes eventually require multiple medications to achieve glycaemic control because of its progressive deterioration of beta-cell function [108-110]. Medication adherence is influenced by the patient, medication and the healthcare system factors.
2.7.3. Patient Factors
Lower-socioeconomic status leading to depression, financial problems, lack of knowledge and poor social support are significant factors in medication non-adherences [109,111-115].
2.7.4. Medication Factors
There is a consistent finding of decreased medication adherence with complexity of treatment like polypharmacy therapy, multiple daily dosing and medication sideeffects [116-120].
2.7.5. Healthcare System
study conducted in New Zealand found good patientphysician communication improved medication adherence by one-third when compared to control group [121]. Other researchers also reported the same findings, although the validity of most of these studies was limited by self-report [115,121,122].
2.8. Effectiveness of Self-Monitoring of Blood Glucose
2.8.1. Effect on Type 1 Diabetes
Consistent findings of improved glycaemic control with increased frequency of SMBG with type 1 diabetes subjective have been reported [123-125].
2.8.2. Effect on Type 2 Diabetes on Insulin Therapy
Earlier studies did not find a beneficial effect from self-monitoring among type 2 diabetes subjects on insulin treatment [123,126-128]. More recent studies found increased frequency of SMBG and treatment modification were associated with better glycaemic and metabolic control. Yet the findings were limited by lack of information of other confounders like dietary change or exchange effects [129-131].
2.8.3. Type 2 Diabetes on Oral-Antihyperglycemic Medication
Two recent systemic reviews on the relationship of SMBG with glycaemic control using randomized controlled trials have been reported. The first by Sarol in 2005 analysed eight studies which include 1307 subjects with duration of 12 - 44 weeks reported SMBG as part of a multi-component management produced a mean reduction of HbA1c by 0.42%. Wlesch in his 2005 systemic review which include six studies also reported a 0.39% decrease in HbA1c with treatment adjustment compared to control group. Both systemic reviews were methodologically sound and included studies from several databases. However they were limited by the quality of the primary studies [132,133]. Although the role of SMBG in type 2 diabetes regarding both OAM and insulin treatment is inconclusive, recent evidence is emerging that it has a beneficial effect.
2.8.4. Factors to Effectiveness of SMBG
Karter and colleagues observed an association between increased frequency of monitoring with better glycaemic control in a managed care population (n = 23,312) regardless of type of diabetes or therapy [124]. Similar findings were reported in other community-based studies [134,135]. In contrast, other studies found glycaemic deterioration with increased monitoring frequency among poorly controlled individuals with type 2 diabetes on insulin treatment [126,129]. No cause effect could be determined due to cross-sectional study design.
2.9. Confounders to Adherence to SMBG
The prevalence of SMBG is consistently correlated with treatment mode. Insulin users practice more testing that subject on oral medication and the least users were those on diet control [126,127,136,137]. Patients with type 1 diabetes test more often than those with type 2 diabetes [124,138,139]. Some studies found decreased testing frequency with depression and fewer physician visits [54,140]. Family support and self-efficacy were noted to increase testing frequency [124,125,135,141, 142]. Cost is another significant predictor of less frequent monitoring [124,125,135,141,142]. Although Harris in 2001 found no association between socio-economic status and SMBG frequency, 90% of his subjects had health insurance [126]. Other demographic factors were inconclusive. Cross-sectional design of these studies prevents causal inferences.
3. CONCLUSION
Beside advance in the clinical sciences still some factors include patients’ biomedical variables, the psychosocial environment, the knowledge, attitudes and beliefs of patients themselves, home careers and health care providers, healthcare systems’ accessibility and availability and even the national political context may influence these self-care behaviors.
![]()
![]()
REFERENCES
- World Health Organization (1999) Definition diagnosis and classification of diabetes mellitus and its complications. World Health Organization, Geneva.
- Fried, L. (2000) Epidemiology of aging. Epidemiology Reviews, 22, 95-106. doi:10.1093/oxfordjournals.epirev.a018031
- International Diabetes Federation (2008) Diabetes atlasprevalence. http://www.eatlas.idf.org/Prevalence
- Wild, S., Roglic, G., Green, A., Sicree, R. and King, H. (2004) Global prevalence of diabetes estimates for the year 2000 and projections for 2030. Diabetes Care, 27, 1047-1063. doi:10.2337/diacare.27.5.1047
- Yoon, K.-H., Lee, J.-H., Kim, J.-W., Cho, J.-H., Choi, Y.-H., Ko, S.-H., et al. (2006) Epidemic obesity and type 2 diabetes in Asia. Lancet, 368, 1681-1688. doi:10.1016/S0140-6736(06)69703-1
- Cockram, C. (2000) The epidemiology of diabetes mellitus in the Asia-Pacific region. Hong Kong Medical Journal, 6, 43-52.
- Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine, 329, 977-986. doi:10.1056/NEJM199309303291401
- United Kingdom Prospective Diabetes Study Group (1998) Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. British Medical Journal, 317, 703-713. doi:10.1136/bmj.317.7160.703
- Ohkubo, Y., Kishikawa, H., Araki, E., Myata, T., Isamu, S., Motoyoshi, S., et al. (1995) Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with type 2 diabetes mellitus: A randomized prospective 6-year study. Diabetes Research and Clinical Practice, 28, 103-117. doi:10.1016/0168-8227(95)01064-K
- Assal, J.P. and Lacroix, A. (1990) Educating the patient to manage his disease: The example of diabetes mellitus. Journal of Human Hypertension, 1, 13-20.
- Viswanathan, V. (2007) The diabetic foot: Perspectives from Chennai, South India. Lower Extremity Wounds, 6, 34-36. doi:10.1177/1534734606297987
- Kirkman, M.S., McCarren, M., Shah, J., Duckworth, W. and Abraira, C. (2006) The VADT study group. The association between metabolic control and prevalent macrovascular disease in Type 2 diabetes: The VA Cooperative study in diabetes. Journal of Diabetes and its Complications, 20, 75-80. doi:10.1016/j.jdiacomp.2005.06.013
- The Action to Control Cardiovascular Risk in Diabetes Study Group (2008) Effect of intensive glucose lowering in type 2 diabetes. New England Journal of Medicine, 358, 2545-2559. doi:10.1056/NEJMoa0802743
- The Advance Collaborative Group (2008) Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. The New England Journal of Medicine, 358, 2560-2752. doi:10.1056/NEJMoa0802987
- United Kingdom Prospective Diabetes Study Group (1998) Intensive blood glucose control with sulphonylurease or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet, 352, 837-853. doi:10.1016/S0140-6736(98)07019-6
- AACE Diabetes Mellitus Clinical Practice Guidelines Task Force (2007) American association of clinical endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocrine Practice, 13, 1-108.
- Adler, A.I., Stratton, I.M., Neil, H.A.W., Yudkin, J.S., Mathews, D.R., Cull, C.A., et al. (2000) Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): Prospective observational study. British Medical Journal, 321, 412-419. doi:10.1136/bmj.321.7258.412
- Colhoun, H., Betterodge, D., Durrington, P., Hitman, G., Nell, H.A., Livngstone, S., et al. (2004) Primary prevention of cardiovascular disease with atrovastatin in type 2 diabetes in the Collaborative Atrovastatin Diabetes Study (CARDS): Multicenter randomized placebo-controlled trial. Lancet, 364, 685-694. doi:10.1016/S0140-6736(04)16895-5
- Pyorala, K., Pedersen, T., Kjekshus, J., Faergeman, O., Olsson, A. and Thorgeirsson, G. (1997) Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care, 20, 614-620. doi:10.2337/diacare.20.4.614
- Grant, R.W., Pirraglio, P.A., Megis, J.B. and Singer, D.E. (2004) Trends in complexity of diabetes care in the United States from 1991 to 2000. Archives of Internal Medicine, 164, 1134-1139. doi:10.1001/archinte.164.10.1134
- Anderson, R., Funnell, M., Butler, P., Arnold, M., Fitzgerald, J. and Feate, C. (1995) Patient empowerment results of a randomized controlled tria. Diabetes Care, 18, 943-949. doi:10.2337/diacare.18.7.943
- Lerman, I. (2005) Adherence to treatment. The key for avoiding long-term complications of diabetes. Archives of Medical Research, 36, 300-306. doi:10.1016/j.arcmed.2004.12.001
- Helme, D.W. and Harrington, N.G. (2004) Patient accounts for noncompliance with diabetes self-care regimens and physician compliance-gaining response. Patient Education and Counseling, 55, 281-292. doi:10.1016/j.pec.2003.10.004
- Nelson, K., Reiber, G. and Boyko, E. (2002) Diet and exercise among adults with type 2 diabetes: Findings from the third national health and nutritional examination survey (NHANES III). Diabetes Care, 25, 1722-1728. doi:10.2337/diacare.25.10.1722
- Travis, T. (1997) Patient perceptions of factors that affect adherence to dietary regimens for diabetes mellitus. The Diabete’s Educator, 23, 152-156. doi:10.1177/014572179702300205
- Hays, L. and Clark, D. (1999) Correlates of physical activity in a sample of older adults with type diabetes. Diabetes Care, 22, 706-712. doi:10.2337/diacare.22.5.706
- Harris, M. (2001) Frequency of blood glucose monitoring in relation to glycaemic control in patients with type 2 diabetes. Diabetes Care, 24, 979-982. doi:10.2337/diacare.24.6.979
- Evans, J., Newton, R., Ruta, D., MacDonald, T., Stevenson, R. and Morris, A. (1999) Frequency of blood monitoring in relation to glycemic control: Observational study diabetes database. British Medical Journal, 319, 83-86. doi:10.1136/bmj.319.7202.83
- Allen, N.A. (2003) The history of diabetes nursing, 1914- 1936. The Diabetes Educator, 29, 976-989. doi:10.1177/014572170302900608
- Brown, S. (1988) Effects of education interventions in diabetes care: A meta analysis of findings. Nursing Research, 37, 223-230. doi:10.1097/00006199-198807000-00010
- Brown, S. (1992) Meta analysis of diabetes patient education research: Variations in intervention effects across studies. Research in Nursing and Health, 15, 409-419. doi:10.1002/nur.4770150603
- Austalian Diabetes Educators Association (2008) New diabetes self-care resources for consumers and diabetic educators. Australian Diabetes Educators, 11, 6.
- Funnell, M.M., Brown, T.L., Childs, B.P., Haas, K.B., Hosey, G.M., Fensen, B., et al. (2008) National standards for diabetes self-management education. Diabetes Care, 31, S97-S104. doi:10.2337/dc08-S097
- Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine, 329, 977-986. doi:10.1056/NEJM199309303291401
- United Kingdom Prospective Diabetes Study Group (1998) Intensive blood glucose control with sulphonylurease or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet, 352, 837-853. doi:10.1016/S0140-6736(98)07019-6
- Anderson, R., Funnell, M., Butler, P., Arnold, M., Fitzgerald, J. and Feate, C. (1995) Patient empowerment results of a randomized controlled trial. Diabetes Care, 18, 943-949. doi:10.2337/diacare.18.7.943
- Jacobson, A. (1996) Current concepts: The psychological care of patients with insulin-dependent diabetes mellitus. New England Journal of Medicine, 334, 1249-1254. doi:10.1056/NEJM199605093341907
- Toljamo, M. and Hentinen, M. (2001) Adherence to selfcare and glycaemic control among people with insulindependent diabetes mellitus. Journal of Advanced Nursing, 34, 780-786. doi:10.1046/j.1365-2648.2001.01808.x
- Russell, L.B., Suh, D.-C. and Safford, M.M. (2005) Time requirements for diabetes self-management: Too much for many? The Journal of Family Practice, 54, 52-56.
- Wen, L.K., Parchman, M.L. and Shepherd, M.D. (2004) Family support and diet barriers among older Hispanic adults with type 2 diabetes. Family Medicine, 36, 423-430.
- Safford, M.M., Russell, L.B., Suh, D.-C., Roman, S. and Pogach, L. (2005) How much time do patients with diabetes spend on self-care? Journal of American Board Family Practice, 18, 262-270. doi:10.3122/jabfm.18.4.262
- Paterson, B.L., Russell, C. and Throne, S. (2002) Critical analysis of everyday self-care decision making in chronic illness. Journal of Advanced Nursing, 35, 335-341. doi:10.1046/j.1365-2648.2001.01850.x
- Zhang, J. and Verhoel, M.J. (2002) Illness management strategies among Chinese immigrants living with arthritis. Social Science & Medicine, 55, 1795-1802. doi:10.1016/S0277-9536(01)00311-2
- Hunt, J., Pugh, J. and Valenzuela, M. (1998) How patients adapt diabetes self-care recommendations in everyday life. The Journal of Family Practice, 46, 207-215.
- Blaiss, M.S. (2004) Asthma disease management: A critical analysis. Annals of Allergy, Asthma & Immunology, 95, S10-S16. doi:10.1016/S1081-1206(10)61004-6
- Bodenheimer, T., Lorig, K., Homan, H. and Grumbach, K. (2002) Patient self-management of chronic disease in primary care. Journal of America Medical Association, 288, 2469-2475. doi:10.1001/jama.288.19.2469
- Ni, H., Nauman, D., Donna, B., Wise, K., Crispell, K. and Hershberger, R.E. (2006) Factors influencing knowledge of and adhehrence to self-care among patients with heart failure. Archives of Internal Medicine, 159, 1613-1619. doi:10.1001/archinte.159.14.1613
- Hawthorne, K. and Tomlinson, S. (1999) Pakistani Moslems with type 2 diabetes mellitus: Effect of gender, literacy skills, know diabetic complications and place of care on diabetic knowledge, reported self-monitoring management and glycaemic control. Diabetic Medicine, 16, 591-597. doi:10.1046/j.1464-5491.1999.00102.x
- Hawthorne, K. (2001) Effect of culturally appropriate health education on glycaemic control and knowledge of diabetes in British Pakistani women with type 2 diabetes mellitus. Health Education Research, 16, 373-381. doi:10.1093/her/16.3.373
- Hartz, A., Kent, S., James, P., Xu, Y.H., Kelly, M. and Daly, J. (2006) Factors that influence improvement for patients with poorly controlled type 2 diabetes. Diabetes Research and Clinical Practice, 74, 227-232. doi:10.1016/j.diabres.2006.03.023
- Taylor, M., Frier, B.M., Gold, A. and Deary, I. (2003) Psychological factors and diabetes related outcomes following diagnosis of Type 1 diabetes in adults: The Edinburgh prospective diabetes study. Diabetic Medicine, 20, 135-146. doi:10.1046/j.1464-5491.2003.00887.x
- Tu, K.S. and Gay, J.T. (1993) Diabetes self-care knowledge, behaviors and metabolic control of older adults— The effect of a posteducational follow-up program. The Diabetes Educator, 19, 25-30.
- Jacobson, A., Alder, A., Wolfsdorf, J., Anderson, B. and Derby, L. (1990) Psychological characteristics of adults with IDDM. Comparison of patients in poor and good glycaemic control. Diabetes Care, 13, 375-381. doi:10.2337/diacare.13.4.375
- Lerman, I., Lazano, L., Villa, A.R., Hermandez-Jimmenez, S., Weinger, K., Caballero, A.E., et al. (2004) Psyhological factors associated with poor diabetes selfmanagement in a specialized center in Mexico City. Biomedicine & Pharmacotherapy, 58, 566-570. doi:10.1016/j.biopha.2004.09.003
- Delahanty, L. and Hiford, B. (1993) The role of diet behaviors in achieving improved glycaemic control in intensively treated patient in the diabetes control and complications trials. Diabetes Care, 16, 1453-1458. doi:10.2337/diacare.16.11.1453
- Franz, M., Monk, A., Barry, B., McClain, K., Weaver, T., Cooper, N., et al. (1995) Effectiveness of medical nutrition therapy provided by dieticians in the management of non-insulin dependent diabetes mellitus: A randomized controlled clinical trial. Journal of the American Dietetic Association, 95, 1009-1017. doi:10.1016/S0002-8223(95)00276-6
- Pastors, J., Warshaw, H., Daly, A., Franz, M. and Kulkarni, K. (2002) The evidence for the effectiveness of medical nutritional therapy in diabetes management. Diabetes Care, 25, 608-613. doi:10.2337/diacare.25.3.608
- Murata, G., Shah, J., Duckworth, W., Wendel, C., Mohler, M. and Hoffman, R. (2004) Food frequency questionnaire results correlate with metabolic control in insulin-related veterans with type 2 diabetes: The diabetes outcomes in Veterans study. Journal of American Dietetic Association, 12, 1816-1826. doi:10.1016/j.jada.2004.09.026
- McLean, H. (1991) Patterns of diet related self-care in diabetes. Social Science and Medicine, 32, 689-696. doi:10.1016/0277-9536(91)90148-6
- Brunner, E., White, I., Thorogood, M., Bristow, A., Curle, D. and Marmot, M. (1997) Can dietary interventions change diet and cardiovascular risk factors? A meta analysis of randomized controlled trials. American Journal of Public Health, 87, 1415-1422. doi:10.2105/AJPH.87.9.1415
- Cernea, S., Hancu, N. and Raz, I. (2003) Diet and coronary heart disease in diabetes. Acta Diabetologia, 40, S389-S400. doi:10.1007/s00592-003-0125-8
- Klein, S., Sheard, N.F., Pi-Sunyer, X., Daly, A., WylieRosett, J., Kulkarni, K., et al. (2004) Weight management through lifestyle modification for the prevention and management of type 2 diabetes: Rationale and strategies. Diabetes Care, 27, 2067-2073. doi:10.2337/diacare.27.8.2067
- Moore, H., Summerbell, C.D., Hooper, L., Nield, L., Cruickshank, K., Vyas, A., et al. (2004) Dietary advice for treatment of type 2 diabetes mellitus in adults. The Cochrane Database of Systematic Reviews, 3, CD004097.
- Ruggiero, L., Glassgow, R., Dryfoos, J., Rossi, J., Prochaska, J., Orleans, C., et al. (1997) Diabetes self-management: Self-reported recommendations and patterns in a large population. Diabetes Care, 20, 568-576. doi:10.2337/diacare.20.4.568
- Chang, H.Y., Chious, C.J., Lin, M.C., Lin, S.H. and Tai, T.Y. (2005) A population study of the self-care behaviours and their associated factors of diabetes in Taiwan: Results from the 2001 national health interview survey in Taiwan. Preventive Medicine, 40, 344-348. doi:10.1016/j.ypmed.2004.06.012
- Cox, R., Carpenter, J., Bruce, F., Poole, K. and Gaylord, C. (2004) Characteristics of low-income African-American and Caucasian adults that are important in self-management of type 2 diabetes. Journal of Community Health, 29, 155-170. doi:10.1023/B:JOHE.0000016719.89848.b1
- Meeto, D. (2004) Dietry pattern of self-care among Asian and Caucasians diabetic patients. British Journal of Nursing, 13, 1074-1078.
- Nelson, K., Reiber, G. and Boyko, E. (2002) Diet and exercise among adults with type 2 diabetes: Findings from the third national health and nutritional examination survey (NHANES III). Diabetes Care, 25, 1722-1728. doi:10.2337/diacare.25.10.1722
- Nthangeni, G., Steyn, N.P., Alberts, M., Steyn, K., Levitt, N.S., Laubscher, R., et al. (2002) Dietry intake and barriers to dietry compliance in black type 2 diabetic patients attending primary healthcare services. Public Health Nutrition, 5, 329-338. doi:10.1079/PHN2002256
- Toobert, S., Hampson, S. and Glasgow, R. (2000) The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23, 943-950. doi:10.2337/diacare.23.7.943
- Savoca, M.R., Miller, C.K. and Ludwig, D.A. (2004) Food habits are related to glycaemic control among people with type 2 diabetes mellitus. Journal of the American Dietetic Association, 104, 560-566. doi:10.1016/j.jada.2004.01.013
- Albarran, N.B., Balleseros, M.N., Morales, G.G. and Ortega, M.I. (2006) Dietary behavior and type 2 diabetes care. Patient Education and Counseling, 61, 191-199. doi:10.1016/j.pec.2005.03.008
- Lawton, J., Ahmad, N., Hallowell, N., Hanna, K. and Douglas, M. (2005) Perceptions and experience of taking oral hypoglycemic agents among people of Pakistani and Indian origin: Qualitative study. British Medical Journal, 330, 1247-1251. doi:10.1136/bmj.38460.642789.E0
- Vijen, S., Stuart, N., Fitzgerald, J., Ronis, D., Hayward, R. and Slater, S. (2004) Barriers to following dietary recommendation in type 2 diabetes. Diabetic Medicine, 22, 32-38. doi:10.1111/j.1464-5491.2004.01342.x
- Whittemore, R. (2000) Strategies to facilitate lifestyle change associated with diabetes mellitus. Journal of Nursing Scholarship, 32, 225-232. doi:10.1111/j.1547-5069.2000.00225.x
- Wen, L., Shepherd, M. and Parchaman, M. (2004) Family support, diet and exercise among older Mexican Americans with type 2 diabetes. The Diabetes Educator, 30, 980-993. doi:10.1177/014572170403000619
- Savoca, M., Miller, C. and Quandt, S. (2004) Profiles of people with type 2 diabetes mellitus. The extremes of glycaemic control. Social Science and Medicine, 58, 2655- 2666. doi:10.1016/j.socscimed.2003.09.031
- Wolever, T.M.S., Hamad, S., Chiasson, J.-L., Josse, R.G., Leiter, L.A., Rodger, W., et al. (1999) Day-to-day consistency in amount and source of carbohydrate intake associated with improved blood glucose control in type 1 diabetes. Journal of the American College of Nutrition, 18, 242-247.
- Whittemore, R., Melkus, G. and Grey, M. (2005) Metabolic control, self-management and psychosocial adjustment in women with type 2 diabetes. Journal of Clinical Nursing, 14, 195-199. doi:10.1111/j.1365-2702.2004.00937.x
- Sherman, A.M., Bowen, D.J., Vitolins, M., Sevick, M.A. and Ockene, J.K. (2000) Dietary adherence: Characteristics and interventions. Controlled Clinical Trial, 21, 206S- 211S. doi:10.1016/S0197-2456(00)00080-5
- Vallis, T. (1998) Understanding diabetes non-adherence: Psychosocial factors associated with poor self-care. Canadian Journal of Diabetes Care, 22, 13-21.
- Peyrot, M., Rubint, R., Lauritzen, T., Snoek, F., Mathews, D., Skovlund, S., et al. (2005) Psychosocial problems and barriers to improved diabetes management: Results of the cross-sectional Diabetes Attitudes, Wishes and Needs (DAWN) study. Diabetic Medicine, 22, 1379-1385. doi:10.1111/j.1464-5491.2005.01644.x
- Jerant, A., von Friederichs-Fitzwater, M. and Moore, M. (2005) Pateints percieved barriers to active self-management of chronic conditions. Patient Education Counseling, 57, 300-307. doi:10.1016/j.pec.2004.08.004
- Funnell, M.M., Hunt, C., Kulkarni, K., Rubin, R.R. and Yorborough, P.C. (1998) A core curriculum for diabetes education. 3rd Edition, American Association Diabetes Educators, Chicago.
- Agurus-Collins, T., Kumanyika, S., Ten Have, T. and Adams Campbell, L. (1997) A randomized control trial of weight reduction and exercise for diabetes maanagment in older African-American subjects. Diabetes Care, 20, 1503-1511. doi:10.2337/diacare.20.10.1503
- Boule, N., Haddad, E., Kenny, G., Wells, G. and Sigal, R. (2001) Effects of exercise on glycaemic control and body mass in type 2 diabetes mellitus: A meta analysis of xontrolled clinical trials. Journal of American Medical Association, 286, 1218-1227. doi:10.1001/jama.286.10.1218
- Hu, G., Jousilahti, P., Barengo, N.C., Qiag, Q., Lakka, T.A. and Tuomilehto, J. (2005) Physical activity, cardiovascular risk factors, and mortality among Finnish adults with diabetes. Dianbetes Care, 28, 799-803. doi:10.2337/diacare.28.4.799
- Morey, M.C., Pieper, C.F., Crowley, G.M., Sullivan, R.J. Jr. and Publisi, C.M. (2002) Exercise adherence and 10 year-mortality in chronically ill older adults. Journal of American Geriatric Society, 50, 1929-1933. doi:10.1046/j.1532-5415.2002.50602.x
- Nothwehr, F. and Stump, T. (2000) Health promoting behaviors among adults with type 2 diabetes: Findings from the health and retirement study. Preventive Medicine, 30, 407-414. doi:10.1006/pmed.2000.0658
- Dutton, G.R., Johnson, J., Whitehead, D., Bodenlos, J.S. and Brantely, P. (2005) Barriers to physical activity among predominantly low-incomce African-American patients with Type 2 diabetes. Diabetes Care, 28, 1209-1210. doi:10.2337/diacare.28.5.1209
- Dye, C., Haley-Zitlin, V. and Willoughly, D. (2003) Insights from older adults with type 2 diabetes: Making dietary and exercise changes. The Diabetes Educator, 29, 116-127. doi:10.1177/014572170302900116
- Swift, C., Armstrong, J., Berman, K., Cambell, R. and Pond-Smith, D. (1995) Attitudes and beliefs about exercise among persons with non-insulin dependent diabetes. The Diabetes Educator, 21, 523-540. doi:10.1177/014572179502100607
- Hays, L. and Clark, D. (1999) Correlates of physical activity in a sample of older adults with type 2 diabetes. Diabetes Care, 22, 706-712. doi:10.2337/diacare.22.5.706
- Shin, Y., Yun, S., Pender, N. and Jang, H. (2005) Test of the health promotion model as a casual model of commitment to a plan for exercise among Korean Adults with chronic disease. Research in Nursing & Health, 28, 117- 125. doi:10.1002/nur.20060
- Plotnikoff, R.C., Brez, S. and Hotz, S.B. (2000) Exercise behavior in a community sample with diabetes: Understanding the determinants of exercise behavioral change. The Diabetes Educator, 26, 450-459. doi:10.1177/014572170002600312
- Aljasem, L.I., Peyrot, M., Wissow, L. and Rubin, R.R. (2001) The impact of barriers and self-efficacy on self care behaviors in type 2 diabetes. The Diabetes Educator, 27, 393-404. doi:10.1177/014572170102700309
- Jorgensen, W., Polivka, B. and Lennie, T. (2002) Perceived adherence to prescribed or recommended standards of care among adults with diabetes. The Diabetes Educator, 28, 989-998. doi:10.1177/014572170202800613
- Thomas, N., Alder, E. and Lesse, G. (2004) Barriers to physical activity in patients with diabetes. Postgraduate Medical Journal, 80, 287-291. doi:10.1136/pgmj.2003.010553
- Lim, K. and Taylor, L. (2005) Factors associated with physical activity among older people—A population based study. Preventive Medicine, 40, 33-40. doi:10.1016/j.ypmed.2004.04.046
- Allen, N. (2004) Cognitive theory in diabetes exercise research: An integrative literature review. The Diabetics Educator, 30, 805-819. doi:10.1177/014572170403000516
- Estacio, R.O., Wolfel, E.E., Regensteiner, J.G., Ferrers, B., Javramel, E.P., Sabage, S., et al. (1996) Effects of risk factors on exercise capacity in NIDDM. Diabetes, 45, 79-85. doi:10.2337/diabetes.45.1.79
- Fischbachler, C., Hunt, S. and Alexander, L. (2004) How physically active are South Asians in the United Kingdom? A literature review. Journal of Public Health, 26, 250- 258. doi:10.1093/pubmed/fdh158
- Kandula, N.R. and Lauderdale, D.S. (2005) Leisure time, non-leisure time and occupational physical activity in Asian Americans. Annals of Epidemiology, 15, 257-265. doi:10.1016/j.annepidem.2004.06.006
- Lawton, J., Ahmad, N., Hanna, L., Douglas, M. and Hallowell, N. (2005) “I can’t do any serious exercise”: Barriers to physical activity amongst people of Pakistani and Indian origin with type 2 diabetes. Health Education Research, 20, 1-12.
- Wooldridge, K., Wallston, K., Graber, A., Brown, A. and Davidson, P. (1992) The relationship between health beliefs, adherence and metabolic control of diabetes. Diabetes Education, 18, 495-500. doi:10.1177/014572179201800608
- Diehl, A., Bauer, R. and Sigarel, N. (1987) Correlates of medication compliance in non-insulin dependent diabetes mellitus. South Medical Journal, 80, 332-335. doi:10.1097/00007611-198703000-00014
- Rhee, M.K., Slocum, W., Ziemer, D.C., Culler, S.D., Cook, C.B., El-Kebbi, I.M., et al. (2005) Patient adherence improves glycaemic control. The Diabetic Educator, 31, 240- 250. doi:10.1177/0145721705274927
- Balkrishnan, R. (2005) The importance of medication adherence in improving chronic-disease related outcomes: What we know and what we need to further know. Medical Care, 43, 517-520. doi:10.1097/01.mlr.0000166617.68751.5f
- Rubin, R.R. (2005) Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. The American Journal of Medicine, 118, 275-345. doi:10.1016/j.amjmed.2005.04.012
- Blaum, C., Velve, K., Hiss, R. and Halter, J. (1997) Characteristics related to poor glycaemic control in NIDDM patients in community practice. Diabetes Care, 20, 7-11. doi:10.2337/diacare.20.1.7
- Mojtabal, R. and Olfson, M. (2003) Medication costs, adherence and health outcomes among medicare beneficiaries. Health Affairs, 23, 220-229. doi:10.1377/hlthaff.22.4.220
- Lin, E.H., Katon, W.J., Von Korff, M., Rutter, C., Simon, G.E., Oliver, M., et al. (2004) Relationship of depression and diabetes self-care, medication adherence and preventive care. Diabetes Care, 27, 2154-2160. doi:10.2337/diacare.27.9.2154
- Piette, J.D., Heisler, M. and Wagner, T.H. (2006) Medication characteristics beyond cost alone influence decisions to underused pharmacotherapy in response to financial pressure. Journal of Clinical Epidemiology, 59, 739-746. doi:10.1016/j.jclinepi.2005.11.023
- Haynes, R.B., McDonald, H.P., Garg, A. and Montague, P. (2002) Interventions for helping patients to follow prescriptions for medication (review). Cochrane Database of Systemic Reviews, 2, CD000011.
- Bartel, D. (2004) Adherence to oral therapy for type 2 diabetes, opportunities for enhancing glycaemic control. Journal of the American Academy of Nursing Practitioners, 16, 8-16.
- Boccuzzi, S., Wogen, J., Fox, J., Sung, J., Shah, A. and Kim, J. (2005) Utilization of oral hypoglycaemic agents in drug insured US population. Diabetes Care, 28, 78-83.
- Donnan, P., MacDonald, T. and Morris, A. (2002) Adherence to prescribed oral hypoglycaemic medication in population of patients with type 2 diabetes: A retrospective cohort study. Diabetic Medicine, 19, 279-284. doi:10.1046/j.1464-5491.2002.00689.x
- Cramer, J. (2004) A systemic review of adherence with medication for diabetes. Diabetes Care, 27, 1218-1224. doi:10.2337/diacare.27.5.1218
- Pladvell, M., Williams, L., Potts, L., Dividne, G., Xi, H. and Lafata, J. (2004) Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care, 27, 2800-2805. doi:10.2337/diacare.27.12.2800
- Hertz, R.P., Unger, A.N. and Lustik, M.B. (2005) Adherence with pharmacotherapy for type 2 diabetes: A retrospective cohort study of adults with employer sponsored health insurance. Clinical Therapeutics, 27, 1064-1073. doi:10.1016/j.clinthera.2005.07.009
- Piette, J.D., Heisler, M., Krein, S. and Kerr, E.A. (2005) The role of patient physician trust in moderating medication nonadherence due to cost pressures. Archives of Internal Medicine, 165, 1749-1755. doi:10.1001/archinte.165.15.1749
- Ciechanowski, P.S., Katon, W., Russo, J. and Walker, E. (2001) The patient provider relationship: Attachment theory and adherence to treatment in diabetes. American Journal of Psychiatry, 158, 29-35. doi:10.1176/appi.ajp.158.1.29
- Evans, J., Newton, R., Ruta, D., MacDonald, T., Stevenson, R. and Morris, A. (1999) Frequency of blood glucose monitoring in relation to glycaemic control: Observational study with diabetes database. British Medical Journal, 319, 83-86. doi:10.1136/bmj.319.7202.83
- Karter, A.J., Ferrara, A., Darbinian, J.A., Ackerson, L.M. and Selby, J.V. (2001) Self monitoring of blood glucoselanguage and financial barriers in a managed care population with diabetes. Diabetes Care, 23, 477-483. doi:10.2337/diacare.23.4.477
- Nyomba, B., Berard, L. and Murphy, L. (2003) Facilitating access to glucometer reagents increase blood glucose self-monitoring frequency and improves glycaemic control: A prospective study in insulin treated diabetes patients. Diabetic Medicine, 21, 129-135. doi:10.1046/j.1464-5491.2003.01070.x
- Harris, M. (2001) Frequency of blood glucose monitoring in relation glycaemic control in patients with type 2 diabetes. Diabetes Care, 24, 979-982. doi:10.2337/diacare.24.6.979
- Oki, J., Flora, D. and Isley, W. (1997) Frequency and impact to SMBG on glycaemic control in patients with NIDDM in an urban teaching hospital clinic. The Diabetes Educator, 23, 419-424. doi:10.1177/014572179702300406
- Coster, S., Gulliford, M., Seed, P., Powriet, J. and Seaminathan. R. (2000) Self monitoring in type 2 diabetes mellitus: A meta-analysis. Diabetic Medicine, 17, 755-761. doi:10.1046/j.1464-5491.2000.00390.x
- Franciosi, M., Pellegrini, F., De Beradis, G., Belfiglio, M., Cavaliere, D., Nardo, B.D., et al. (2001) The impact of blood glucose self-monitoring on metabolic control and quality of life in type 2 diabetic patients: An urgent need for better educational strategies. Diabetic Care, 24, 1871- 1877. doi:10.2337/diacare.24.11.1870
- Ozmen, B. and Boyvada, S. (2003) The relationship between self-monitorong of blood glucose control and glycosylated haemoglobin in patients with type 2 diabetes with and without diabetic retinopathy. Journal of Diabetes and the Complication, 17, 128-134.
- Kibriya, M., Ali, L., Banik, N. and Khan, A. (1999) Home monitoring of blood glucose (HMBG) in type 2 diabetes mellitus in a developing country. Diabetes Research Clinical Practice, 46, 253-257. doi:10.1016/S0168-8227(99)00093-5
- Welschen, L.M., Bloemendal, E., Nijpels, G., Dekker, J., Heine, R.J., Stalman, W.A., et al. (2005) Self-monitoring of blood glucose in patients with type 2 diabetes who are not using insulin. The Cochrane Database of Systematic Reviews, 18, CD005060.
- Sarol, J. Jr, Nicodemus, N. Jr, Tan, K. and Grave, M. (2005) Self-monitoring of blood glucose as part of mutlicomponent therapy among non-insulin requiring type 2: Meta-analysis (1996-2004). Current Medical Research and Opinion, 21, 173-183. doi:10.1185/030079904X20286
- Guerci, B., Drouin, P., Grange, V., Bougneres, P., Fontaine, P., Kerlan, V., et al. (2003) Self-monitoring of blood glucose significanlty improves metabolic control in patients with type 2 diabetes mellitus: The Auto-Surveillance Intervention active (ASIA) study. Diabetes & Metabolism, 29, 587-594. doi:10.1016/S1262-3636(07)70073-3
- Soumerai, S., Mah, C., Fang, Z., Adam, A., Barton, M., Fajtova, V., et al. (2004) Effects of health maintainance organization coverage of self-monitoring devices on diabetes self-care and glycaemic control. Archives of Internal Medicine, 164, 645-652. doi:10.1001/archinte.164.6.645
- Adam, A., Mah, C., Soumeri, S., Zhang, F., Barton, M. and Ross-Degnam, D. (2003) Barriers to self-monitoring of blood glucose among adults with diabetes in an HMO: A cross sectional study. BMJ Health Services Research, 3, 6-10. doi:10.1186/1472-6963-3-6
- Bjorsness, D.K., Krezowski, P.A., Harwell, T.S., McDowall, J.M., Butcher, M.K., Helgerson, S.D., et al. (2003) Self-monitoring blood glucose practices: Do patients know and act on their target? Diabetes Care, 26, 3353-3354. doi:10.2337/diacare.26.12.3353
- Storimans, M., Talsma, H., Kungel, O. and de Blaey, C. (2004) Dispensing glucose test materials in Dutch community pharmacies. Pharmacy World Science, 26, 52-55. doi:10.1023/B:PHAR.0000013475.75062.55
- Vincze, G., Barner, J. and Lopez, D. (2004) Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. The Diabetes Educator, 30, 112-125. doi:10.1177/014572170403000119
- Mcgee, B., Stoll, J., Misra, M., Perlmuter, L. and Singh, S. (2002) Subsyndromal depression and self-monitoring of blood glucose. Diabetes, 51, A619-A620.
- Bowker, S., Mitchell, C., Majunmdar, S., Toth, E. and Johnson, J. (2004) Lack of insurance coverage for testing supplies is associated with poorer glycaemic control in patients with type 2 diabetes. Journal of the Canadian Medical Association, 17, 39-43. doi:10.1503/cmaj.1031830
- Zgibor, J. and Simmons, D. (2002) Barriers to blood glu- cose monitoring in a multiethenic community. Diabetes Care, 25, 1772-1777. doi:10.2337/diacare.25.10.1772
NOTES
*All these authors contributed equally to this work. Conflict of interest: NO.

