Open Journal of Anesthesiology
Vol.2 No.4(2012), Article ID:22234,4 pages DOI:10.4236/ojanes.2012.24037
Subcutaneous Dissociative Conscious Sedation (sDCS) a New Approach to Compromised Airway in Mediastinal Masses
![]()
1Department of Anesthesiology and Critical Care, Imam Khomeinee Medical Center, Tehran University of Medical Sciences, Tehran, Iran; 2Department of Thoracic Surgery, Imam Khomeinee Medical Center, Tehran University of Medical Sciences, Tehran, Iran.
Email: *mihanjavid@yahoo.com, jafarija@sina.tums.ac.ir
Received June 4th, 2012; revised July 8th, 2012; accepted July 30th, 2012
Keywords: Airway Management; Difficult Airway; Low Dose Ketamine; Mediastinal Masses; Subcutaneous Ketamine; Subcutaneous Dissociative Conscious Sedation
ABSTRACT
Purpose: Anesthesia and airway management for mediastinal masses are challenging and are accompanied by mortality and morbidity. Avoiding the loss of airway muscular tone in mediastinal masses has been confirmed necessary to avoid airway collapse. Sufficient spontaneous ventilation is of paramount importance in order to reduce the rate of mortality and morbidity. Various anesthetics and anesthesia techniques have been used for maintaining spontaneous ventilation and patent airway. In this report, a successful double lumen endobronchial intubation using “subcutaneous dissociative conscious sedation” as a novel method in the management of compromised airway (a case of a mediastinal mass) is presented. Clinical Features: A 42-year-old, 62 Kg man was presented for an open biopsy of a middle mediastinal mass. The patient had a history of chest pain, dyspnea, cough, fever and sweats for 2 months. Regarding to the life threatening nature of mediastinal masses resulting from unpredictable events of airway obstruction and the reported cases of deaths after induction of anesthesia in patients with mediastinal masses and regarding to the importance of not losing muscular tone and keeping airway tone intact in patients with mediastinal masses “subcutaneous Dissociative Conscious Sedation (a novel method of anesthesia)” was selected in order to guarantee the safety of the patient and keep the airway secure. Conclusion: Owing to the characteristics of the “subcutaneous dissociative conscious sedation” this method is suggested as an appropriate substitute to general anesthesia for Endobronchial Double Lumen Intubation in mediastinal masses and compromised airway.
1. Introduction
The life threatening nature of mediastinal masses resulting from unpredictable events of airway obstruction [1-6]. and the reported cases of deaths after induction of anesthesia in patients with mediastinal masses [7,8] emphasize on the paramount importance of the muscular tone of the airway and keeping the airway tone intact in patients with mediastinal masses. Sufficient spontaneous ventilation is of paramount importance in order to reduce the rate of mortality and morbidity and preserve the patients’
safety.
Dissociative Conscious Sedation (DCS) is a novel method which was designed in 2004 and reported in January 2011 as an alternative to general anesthesia in patients scheduled for laparoscopic peritoneal dialysis catheter insertion and then in October 2011 as an alternative to regional airway blocks in compromised airway. The first report of using subcutaneous DCS successfully, in the management of predicted difficult airway was presented by the author in 2009 in “The 1st International Congress of Airway Management/and Anesthesia in Head and Neck Surgery”.
The approval for the publication of this report was obtained from the ethics committee of Tehran University of Medical Sciences. Written consent for publication of the information and video clip was obtained from the patient.
Case History1
A 42-year-old, 62 Kg man was presented for an open biopsy of a middle mediastinal mass. The patient had a history of chest pain, dyspnea, orthopnea, cough, fever and sweats for 2 months.
Because of the proximity of the mass to the large vessels and vital organs, the trial for biopsy under CT guide was unsuccessful and ultimately an open biopsy through the right hemi-thorax was planned. Given the poor localization of the mass, in order to provide appropriate surgical access, insertion of a Double Lumen Endobronchial Tube and the establishment of one lung ventilation were needed (Figures 1 and 2).
2. Material and Method
After receiving a written consent, “Dissociative Conscious Sedation” was induced with an injection of subcutaneous ketamine 0.5 mg·kg–1, intravenous morphine sulfate 0.1 mg·kg–1 and intravenous fentanyl 100 ug. While the patient was asking to breathe, the narcotic administration was performed slowly and gradually in 10 minutes in order to keep spontaneous ventilation. Supplemental oxygen was administered through a face mask.
Extra fentanyl was considered if the patient was not cooperative enough for laryngoscopy.
The tongue and oropharynx were anesthetized with topical lidocaine spray (4%).
About 10 minutes after the subcutaneous injection of ketamine and achieving the appropriate level of anesthesia (the patient fell asleep and his eyes were closed), the patient was asked to open his mouth and local anesthetic stained blade of laryngoscope was gently inserted while the patient was asked to keep his mouth open and breathe normally. Then a left sided number 39 Double Lumen Tube was localized in the left bronchus while the patient was breathing spontaneously.
The Patient was evaluated for hemodynamic stability (heart rate and blood pressure), oxygen saturation (Spo2), patient cooperation (obedient to open the mouth for laryngoscopy and the number of tries for laryngoscopy), patient comfort (remaining moveless), hallucination and recall.
The patient was obedient and moveless during the laryngoscopy and endobronchial intubation.
Video Clip shows the feasibility of double lumen endobronchial intubation using “subcutaneous dissociative conscious sedation”: http://www.mavaratech.com/download/sDCSmethod.mp4 Given the integrity of the airway reflexes, stimulation of the patient’s cough reflex resulted in expelling an excessive amount of tracheobronchial secretions.
The respiratory secretions were removed by suctioning, then 50 mg sodium thiopental was administered intravenously and anesthesia was maintained with isoflurane 0.7% - 1.5% and ketamine infusion 40 - 80 mg/hour during the surgery. Administration of 50 mg sodium thiopental resulted in unintentional respiratory depression then controlled ventilation was established with no muscle relaxation.
During the 2.5 hour surgery the patient was hemodynamically stable. Oxygen saturation was between 90% - 98% and Etpco2 between 40 - 50 mmHg.
At the end of the surgery an epidural catheter was inserted through the L2 - L3 inter-vertebral space. The catheter was conducted into the thoracic epidural space and 10 ml marcaine 0.0625% was administered through the catheter.
Despite avoiding muscle relaxant, at the end of the surgery because of the surgical manipulation and congestion at the site of the mass, spontaneous ventilation was not sufficient enough. Then Double Lumen Tube was changed to an endotracheal tube number 8. The patient was transferred to the intensive care unit and respiratory support was established until the next morning. The patient was extubated successfully after 16 hours.
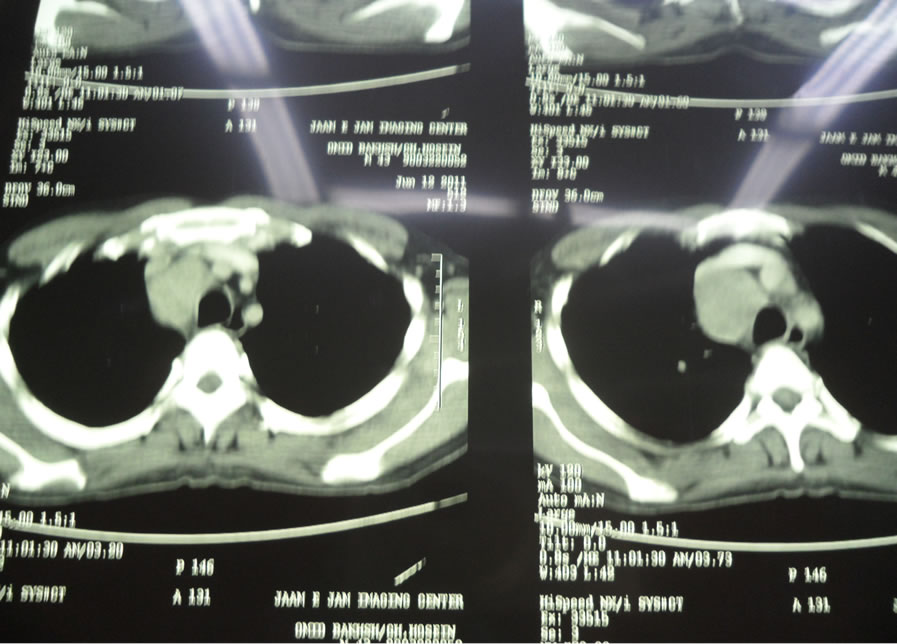
Figure 1. CT view of the mediastinal mass.
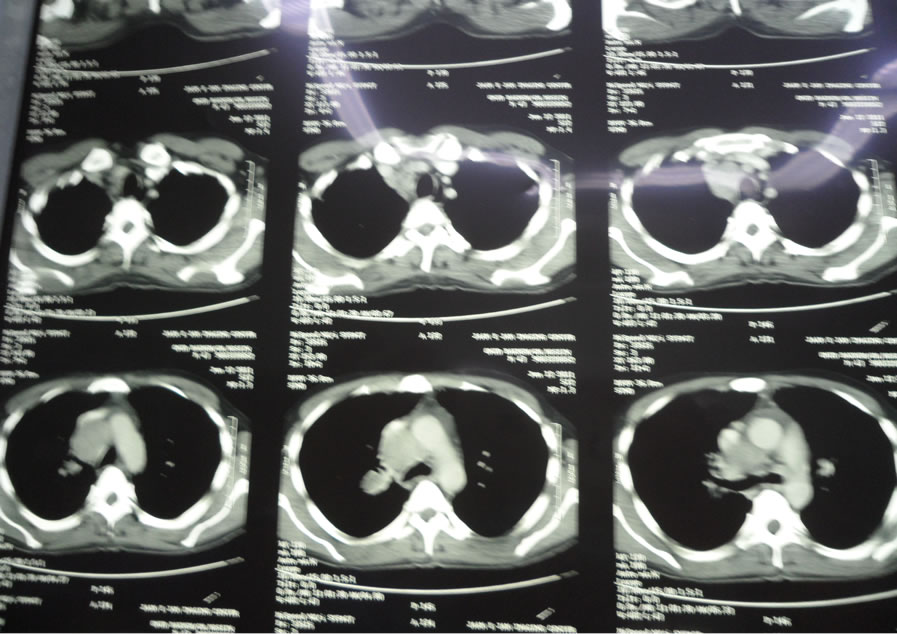
Figure 2. CT view of the tumor localization.
Large cell lymphoma was confirmed by pathologic examination.
3. Results
Direct laryngoscopy and first try endobronchial intubation with double lumen tube was performed successfully. The patient didn’t need extra fentanyl. The patient was cooperative enough during laryngoscopy and endobronchial intubation. No hemodynamic changes more than 20% were observed. Oxygen desaturation (Spo2 < 90%) did not occur. There was no hallucination. No recall was reported.
The aim of this report is introducing “subcutaneous dissociative conscious sedation” as an alternative to general anesthesia for double lumen endobronchial intubation in compromised airway.
4. Discussion
A review of the literature is indicative of the life threatening nature of mediastinal masses resulting from unpredictable events of airway obstruction [1-6]. Death after induction of anesthesia in patients with mediastinal masses has been reported [7,8].
During general anesthesia bronchial smooth muscle tone is lost [9] and general anesthesia is not safe in mediastinal tumors [10] and the importance of maintaining spontaneous ventilation and avoiding positive pressure ventilation has been emphasized in the literature [7-9].
Using muscle relaxants reduces normal trans-pleural pressure gradient and decreases the caliber of the airway and consequently enhances extrinsic compression [11].
Subcutaneous dissociative conscious sedation was used for the first time by the author in Laparoscopic peritoneal dialysis catheter implantation [12]. Then the method was introduced in 2009 [13] and in 2011 as a safe alternative to airway regional blocks in patients with predicted difficult airway [14].
According to previous reports “Dissociative conscious sedation is defined as using an intravenous or subcutaneous injection of low dose ketamine in conjunction with narcotics to achieve an acceptable level of sedation, pain relief and amnesia” [12,14]. Comparison of the subcutaneous and intravenous Dissociative Conscious Sedation in previous studies showed the superiority of subcutaneous dissociative conscious sedation [12,14].
An intradermal injection instead of subcutaneous injection is the most common cause of failure in this method.
Subcutaneous injection has been defined as a shot that delivers the drug into the layer of fat between the skin and the muscle (needle angle 45˚) (Figure 3).
One of the major drawbacks to the use of intravenous DCS in compromised airway is the probability of losing patient’s cooperation for opening the mouth and to be

Figutre 3.. Subcutaneous injection.
obedient during the laryngoscopy and intubation. Loss of consciousness and losing the patient’s cooperation has been reported while using intravenous DCS [12].
Ketamine as the most essential component of “dissociative conscious sedation or dissociative conscious anesthesia” [12,14] has some characteristics that makes the drug unique for using it in the management of predicted difficult airway.
Integrity of muscular tone of the upper airway [15] and the known bronchodilator effect of ketamine [16] are crucial for successful and safe management of compromised airway particularly in mediastinal masses. Stimulation of ventilation due to the direct effect of ketamine on the medullary respiratory neurons and the known role of hypercarbia in increasing the stimulatory effect of ketamine on ventilation are the other desirable effects of ketamine in airway management [16].
The possibility of maintaining spontaneous ventilation and keeping the patient alert enough to be cooperative and obedient during the airway manipulation are among the considerable advantages of subcutaneous DCS. On the other hand this method provides an appropriate level of analgesia, amnesia and patient satisfaction [12,14].
Previous experiences with subcutaneous dissociative conscious sedation showed that the patients reported no annoying recall at the end of the procedure [12,14].
In the subcutaneous route of injection, adverse effects of the intravenous ketamine are attenuated while desirable effects such as spontaneous ventilation, the tone of the upper airway and patient cooperation are preserved. The gradual absorption of ketamine while using it subcutaneously creates lower serum concentration and attenuates the adverse effects [14].
5. Conclusion
Owing to the characteristics of the “subcutaneous dissociative conscious sedation” this method is suggested as an appropriate substitute to general anesthesia for endobronchial intubation in mediastinal masses and compromised airway.
6. Acknowledgements
I would like to thank Mrs. Constance Martin for double checking the quality of written English. The approval for the publication of this report was obtained from the ethics committee of Tehran University of Medical Sciences. Written consent for publication of the information and video clip was obtained from the patient. There is no source of funding or financial support for this report.
REFERENCES
- U. B. Prakash, M. D. Abel and R. D. Hubmayer, “Mediastinal Mass and Tracheal Obstruction during General Anesthesia,” Mayo Clinic Proceedings, Vol. 63, No. 10, 1988, pp. 1004-1011.
- R. G. Azizkhan, D. L. Dudgeon, J. R. Buck, P. M. Colombani, M. Yaster, D. Nichols, C. Civin, S. S. Kramer and J. A. Haller Jr., “Lifethreatening Airway Obstruction as a Complication to the Management of Mediastinal Masses in Children,” Journal of Pediatric Surgery, Vol. 20, No. 6, 1985, pp. 816-822.
- D. R. Northrip, B. K. Bohman and K. Tsueda, “Total Airway Occlusion and Superior Vena Cava Syndrome in a Child with Anterior Mediastinal Tumour,” Anesthesia & Analgesia, Vol. 65, No. 10, 1986, pp. 1079-1082.
- D. Bitter, “Respiratory Obstruction Associated with Induction of General Anesthesia in a Patient with Mediastinal Hodgkin’s Disease,” Anesthesia & Analgesia, Vol. 54, No. 3, 1975, pp. 399-403.
- H. Levin, S. Bursztein and M. Heifetz, “Cardiac Arrest in a Child with an Anterior Mediastinal Mass,” Anesthesia & Analgesia, Vol. 64, No. 11, 1985, pp. 1129-1130.
- L. Létourneau, Y. Lacasse, D. Côté and J. S. Bussières, “Perioperative Cardiorespiratory Complications in Adults with Mediastinal Mass: Incidence and Risk Factors,” Anesthesiology, Vol. 100, No. 4, 2004, pp. 826-834.
- S. Viswanathan, C. E. Campbell and R. C. Cork, “Asymptomatic Undetected Mediastinal Mass: A Death during Ambulatory Anesthesia,” Journal of Clinical Anesthesiology, Vol. 7, 1995, pp. 151-155.
- T. P. Keon, “Death on Induction of Anesthesia for Cervical Lymph Node Biopsy,” Anesthesiology, Vol. 55, No. 4, 1981, pp. 471-472.
- R. K. Sharma, L. Swain and N. Dave, “Anesthetic Management of a Patient with Malignant Mediastinal Mass,” Indian Journal of Anaesthesia, Vol. 47, 2003, pp. 205- 207.
- P. Slinger and C. Karsli, “Management of the Patient with a Large Anterior Mediastinal Mass: Recurring Myths,” Current Opinion in Anesthesiology, Vol. 20, No. 1, 2007, pp. 1-3.
- M. H. Goh, X. Y. Liu and Y. S. Goh, “Anterior Mediastinal Masses: An Anesthetic Challenge,” Anesthesia, Vol. 54, No. 7, 1999, pp. 670-682.
- M. J. Javid, M. Rahimi and A. Keshvari, “Dissociative Conscious Sedation an Alternative to General Anesthesia for Laparoscopic Peritoneal Dialysis Catheter Implantation: A Randomized Trial Comparing Intravenous and Subcutaneous Ketamine,” Peritoneal Dialysis International, Vol. 31, No. 3, 2011, pp. 308-314. doi:10.3747/pdi.2010.00110
- M. J. Javid, “Conscious Sedation with Subcutaneous Ketamine as an Alternative to Airway Regional Blocks,” 1st International Congress of Airway Management and Anesthesia in Head and Neck Surgery, Tehran, 20-22 May 2009, p. 131.
- M. J. Javid, “Subcutaneous Dissociative Conscious Sedation (sDCS) an Alternative Method for Airway Regional blocks: A New Approach,” BMC Anesthesiology, Vol. 11, 2011, p. 19.
- G. Kim, S. M. Green, T. K. Denmark and B. Krauss, “Ventilatory Response during Dissociative Sedation in Children: A Pilot Study,” Academic Emergency Medicine, Vol. 10, No. 2, 2003, pp. 140-145.
- M. G. Soliman, G. F. Brinale and G. Kuster, “Response to Hypercapnia under Ketamine Anesthesia,” Canadian Anesthetists’ Society Journal, Vol. 22, No. 4, 1975, pp. 486- 494.
NOTES
*Corresponding author.
#Author contributions: Mihan J. Javid contributed substantially to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data and drafting the article; Mohammad B. Rahim contributed substantially to the interpretation of data; Shahab Rafiian contributed substantially to the interpretation of data.
1Patient consent: written consent for publication of the information and video clip was obtained from the patient.

