Open Journal of Pediatrics
Vol. 2 No. 1 (2012) , Article ID: 18011 , 5 pages DOI:10.4236/ojped.2012.21015
Primary amenorrhea with transverse vaginal septum and scant hematocolpos: A case report
![]()
1Department of Obstetrics and Gynecology, University of Rochester Medical Center, Rochester, USA
2Department of Obstetrics, Gynecology and Reproductive Science, School of Medicine, University of Pittsburgh, Pittsburgh, USA
Email: lori_homa@urmc.rochester.edu, thomas.semara@medstudent.pitt.edu, *sanfjs@mail.magee.edu
Received 13 September 2011; revised 28 November 2011; accepted 10 January 2012
Keywords: Amenorrhea; Hematocolpos; Distal Obstruction; Hypothalamic Dysfunction
ABSTRACT
Background: A genital outflow tract obstruction is an uncommon cause of primary amenorrhea. If ovulation occurs, menstrual bleeding is prevented. Patients typically present with abdominal/pelvic pain due to hematocolpos. Absence of significant hematocolpos could indicate a secondary source of primary amenorrhea and be challenging to the clinical diagnosis. Case: 17 year-old patient with primary amenorrhea, appropriate Tanner staging secondary sex characteristics, and transverse vaginal septum presents with virtual absence of hematocolpos. After vaginal septum resection, the patient began menstruating, although only evidenced by two cycles of vaginal spotting. Conclusion: Significant hematocolpos is an expected sequella of distal outlet obstruction when collated with secondary sexual characteristics. Absence of such along with suboptimal return of menstruation reflects pathophysiology which may be attributed to a coexistent disorder of the hypothalamus or higher central nervous system function.
1. INTRODUCTION
Primary amenorrhea is the lack of menses by age 15 with secondary sex characteristics, or at 13 with absence of secondary sex characteristics [1,2]. When evaluating a patient with primary amenorrhea, the pathophysiology can be attributed to numerous sources. Chromosomal abnormalities associated with gonadal dysgenesis are the most common, accounting for 40% of cases [3]. It is then followed by hypothalamic hypogonadism at 30%. A transverse vaginal septum/imperforate hymen represents only 3% - 5% of cases.
The physical exam is abnormal in 15% of cases [2,4]. Laboratory testing for follicle stimulating hormone (FSH), thyroid stimulating hormone (TSH), prolactin levels and a progestin challenge help determine the role of the endocrine system in the pathogenesis [2]. If there is evidence of gonadal failure, a karyotype should be performed. Persistently elevated prolactin could indicate a pituitary tumor. MRI is the most sensitive study to assess the pituitary gland [5]. A pelvic ultrasound would confirm the presence of a uterus and/or ovaries. Lack of adequate reproductive organ development requires specific surgical, medical, psychological and long-term follow-up.
In patients with a distal outlet obstruction, pelvic pain likely secondary to hematocolpos is a common complication. We describe a case of essentially absent hematocolpos in a patient with primary amenorrhea, appropriate secondary sex by Tanner staging and a transverse vaginal septum.
2. CASE
A 17-year-old nulligravid female presented to the adolescent gynecology clinic for primary amenorrhea. She underwent thelarche and pubarche at age 13 - 14, and was Tanner IV breast and pubic hair development. She denied abdominal pain, galactorrhea, headaches, visual disturbances, acne, or hirsutism. There were no changes in weight, or evidence for stress. Her growth chart was notable for a delayed growth spurt. She was an elite athlete, playing multiple sports. Thus, she exercised frequently. Her BMI was 20.51 kg/m2. However, she attested to healthy eating habits as well as regular exercise. Her prenatal course was uneventful. She delivered at term at 6 l b 13 oz.
On physical exam there was a small vaginal-introital opening, without obvious bulging of the hymen. A Q-tip could be inserted to one centimeter. At her evaluation, her laboratory testing showed normal FSH 6.7 mIU/ml and LH 1.7 mIU/ml. Prolactin, thyroid function studies, and serum androgens were also within normal limits. Her Estradiol level was 35 pg/ml.
Ultrasound revealed a normal midline uterus with an endometrial lining of 9 mm, and enclosed fluid in the cul-de-sac measuring 75 mm in length. There was a 39 × 36 × 31 mm heterogeneous right adnexal mass. There was no sonographic evidence of hematocolpos (Figure 1). Renal ultrasound revealed a junctional parenchymal defect within the right kidney without evidence of renal agenesis or duplication. Magnetic resonance imaging (MRI) confirmed a right adnexal lesion concerning for hemorrhagic ovarian cyst or hematosalpinx, and a dilated vaginal vault suggesting hematocolpos with a distal obstruction.
Laparoscopy was performed revealing a hemorrhagic ovarian cyst. Both fallopian tubes appeared normal and no endometriosis was visualized. Exam under anesthesia and needle aspiration of the vaginal vault revealed 0.1 ml “old blood” (hematocolpos). Although the MRI suggested hematocolpos, the laparoscopy findings were more aligned with the ultrasound, which demonstrated no evidence of hematocolpos. A transverse vaginal septum was resected. Six weeks postoperatively, a small Pederson speculum could be admitted with a depth of 7 cm. Eight weeks postoperatively, she had two episodes of vaginal spotting, each lasting 3 - 4 days, 28 days apart. She denied any premenstrual molimina. Additionally, she reported a clear, odorless vaginal discharge that was likely physiologic.
3. DISCUSSION
Distal obstruction(s) often result in the accumulation of menstrual fluid in the vagina or uterus described as hematocolpos or hematometra, respectively. Typically these patients present with cyclic pelvic pain and amenorrhea. As demonstrated by the literature review in Table 1, it is rare to present with a distal outlet obstruction, without abdominal pain and hematocolpos. Location of the sep-

Figure 1. Absence of hematocolpos demonstrated by collapsed vaginal cavity (white arrow) on ultrasound.
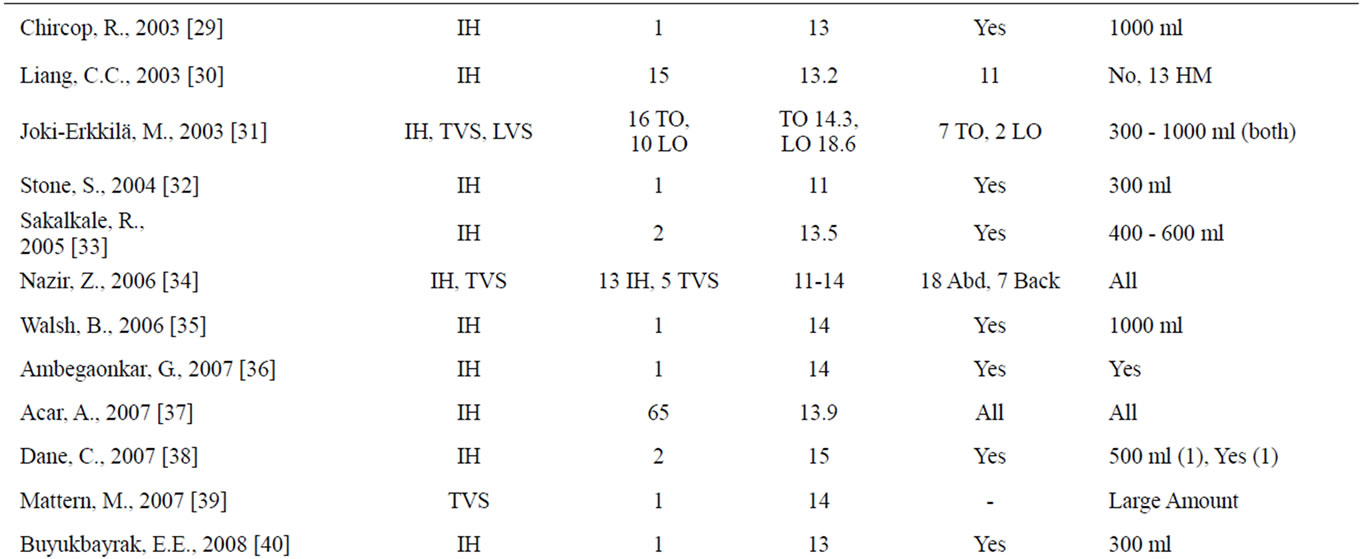
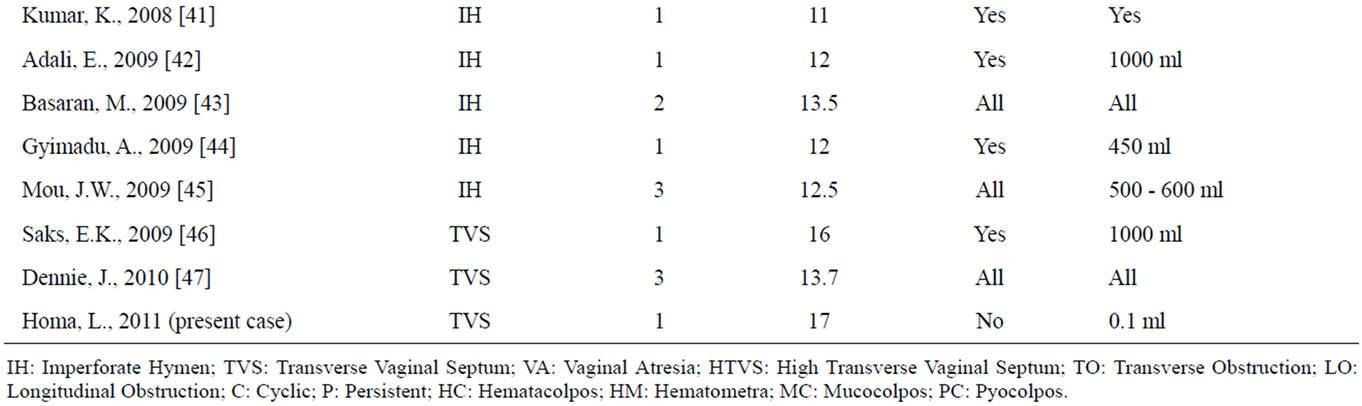
Table 1. Literature review of hematacolpos/hematametra in setting of genital tract outlet obstruction.
tum can affect the timing of presentation. Septa in the lower third of the vagina, such as in this case, occur less frequently (15%), allowing for greater vaginal distension and later presentations [6]. Given that this patient did not present with the typical hematocolpos or lower abdominal pain that is associated with outlet obstructions, and had a suboptimal return of menstruation, she was evaluated for a secondary cause of primary amenorrhea, such as hypothalamic dysfunction.
Hypothalamic amenorrhea is typically characterized by amenorrhea in the absence of anatomic, chromosomal or organic abnormalities. Often a diagnosis of exclusion, it is one of the most common causes of secondary amenorrhea [7]. Hypothalamic dysfunction is associated with abnormal GnRH secretion secondary to a physical/psychological life event or an idiopathic process. Patients are characterized by low-normal gonadotropins, normal prolactin levels, normal sella turnica imaging and failure to demonstrate withdrawal bleeding [8]. Studies indicate that leptin influences the regulation of hypothalamic function, and its administration can induce GnRH pulsatility and menstruation [9]. Because estrogen deficiency is often seen in these patients, the effect of this condition on peak bone mass in young women is concerning. Treatment strategies should aim to address weight gain, exercise reduction, psychosocial factors, bone loss prevention, and the treatment of infertility [10]. In this patient, recognizing some features of the “female athlete triad:” low energy availability, amenorrhea, and osteoporosis, helped establish hypothalamic dysfunction as a possible secondary diagnosis [11].
In conclusion, determining the source of amenorrhea in an adolescent population can be difficult. Transverse vaginal septum in this case was not associated with hematocolpos to the degree that would be in accord with Tanner staging. Clinicians must be aware of atypical presentations and potential multifactorial etiologies of amenorrhea. Ensuring a thorough evaluation is essential in order to mitigate long-term effects of a misdiagnosis.
REFERENCES
- Herman-Giddens, M.E., Slora, E.J., Wasserman, R.C., Bourdony, C.J., Bhapkar, M.V., Koch, G.G., et al. (1997) Secondary sexual characteristics and menses in young girls seen in office practice: A study from the pediatric research in office settings network. Pediatrics, 99, 505-512. doi:10.1542/peds.99.4.505
- Practice Committee of the American Society for Reproductive Medicine (2008) Current evaluation of amenorrhea. Fertility and Sterility, 90, 219-225. doi:10.1016/j.fertnstert.2008.08.038
- Reindollar, R.H., Byrd, J.R. and McDonough, P.G. (1981) Delayed sexual development: A study of 252 patients. American Journal of Obstetrics & Gynecology, 140, 371.
- Deligeoroglou, E., Athanasopoulos, N., Tsimaris, P., Dimopoulos, K.D., Vrachnis, N. and Cretsas, G. (2010) Evaluation and management of adolescent amenorrhea. Annals of the New York Academy of Sciences, 1205, 23-32. doi:10.1111/j.1749-6632.2010.05669.x
- Stein, A.L., Levenick, M.N. and Kletzky, O.A. (1989) Computed tomography versus magnetic resonance imaging for the evaluation of suspected pituitary adenomas. Obstetrics & Gynecology, 73, 996-999. doi:10.1097/00006250-198906000-00018
- Rock, J.A., Zacur, H.A., Dlugi, A.M., et al. (1982) Pregnancy success rates following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstetrics & Gynecology, 59, 448-451.
- Golden, N.H. and Carlson, J.L. (2008) The pathophysiology of amenorrhea in the adolescent. Annals of the New York Academy of Sciences, 1135, 163-178. doi:10.1196/annals.1429.014
- Speroff, L. and Fritz, M. (2005) Clinical gynecology, endocrinology and infertility. 7th Edition, Williams and Wilkins, Lippincott, 438-439.
- Welt, C.K., Chan, J.L., Bullen, J., et al. (2004) Recombinant human leptin in women with hypothalamic amenorrhea. The New England Journal of Medicine, 351, 987-997. doi:10.1056/NEJMoa040388
- Gordon, C. (2010) Functional hypothalamic amenorrhea. The New England Journal of Medicine, 363, 365-371. doi:10.1056/NEJMcp0912024
- Nattiv, A., Loucks, A.B., Manore, M.M., Sanborn, C.F., Sundgot-Borgen, J. and Warren, M.P. (2007) American college of sports medicine position stand: The female athlete triad. Medicine & Science in Sports & Exercise, 39, 1867-1882.
- Amortegui, A.J., Kanbour, A.I. and Silverstein, A. (1979) Diffuse vaginal adenosis associated with imperforate hymen. Obstetrics & Gynecology, 53, 760-762.
- Sailer, J.F. (1979) Hematometra and hematocolpos: Ultrasound findings. American Journal of Roentgenology, 132, 1010-1011.
- Wenof, M., Reyniak, J.V., Novendstern, J. and Castadot, M.J. (1979) Transverse vaginal septum. Obstetrics & Gynecology, 54, 60-64. doi:10.1097/00006250-197907000-00015
- Rock, J.A., Zacur, H.A., Dlugi, A.M., Jones, H.W. Jr. and TeLinde, R.W. (1982) Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstetrics & Gynecology, 59, 448-451.
- Shaw, L.M., Jones, W.A. and Brereton, R.J. (1983) Imperforate hymen and vaginal atresia and their associated anomalies. Journal of the Royal Society of Medicine, 76, 560-566.
- Letts, M. and Haasbeek, J. (1990) Hematocolpos as a cause of back pain in premenarchal adolescents. Journal of Pediatric Orthopaedics, 10, 731-732. doi:10.1097/01241398-199011000-00005
- McIvor, R.A. (1990) Haematocolpos once-in-a-lifetime cause of recurrent abdominal pain. Archives of Emergency Medicine, 7, 51-52.
- Catapano, M., Loscalzo, J. and Sama, A. (1995) Imperforate hymen with bilateral hydronephrosis: An unusual emergency department diagnosis. Journal of Emergency Medicine, 13, 337-339. doi:10.1016/0736-4679(95)00008-X
- Polasek, P.M., Erickson, L.D. and Stanhope, C.R. (1995) Transverse vaginal septum associated with tubal atresia. Mayo Clinic Proceedings, 70, 965-968. doi:10.4065/70.10.965
- Peterson-Sweeney, K.L. and Stevens, J. (1996) 13-yearold female with imperforate hymen. Nurse Practitioner, 21, 90-94. doi:10.1097/00006205-199608000-00008
- Kushnir, O., Garde, K. and Blankstein, J. (1997) Rectal sonography for diagnosing hematocolpometra. A case report. Journal of Reproductive Medicine, 42, 519-520.
- Ahmed, S., Morris, L.L. and Atkinson, E. (1999) Distal mucocolpos and proximal hematocolpos secondary to concurrent imperforate hymen and transverse vaginal septum. Journal of Pediatric Surgery, 34, 1555-1556. doi:10.1016/S0022-3468(99)90129-X
- Bakos, O. and Berglund, L. (1999) Imperforate hymen and ruptured hematosalpinx: A case report with a review of the literature. Journal of Adolescent Health, 24, 226-228. doi:10.1016/S1054-139X(98)00077-9
- Buick, R.G. and Chowdhary, S.K. (1999) Backache: A rare diagnosis and unusual complication. Pediatric Surgery International, 15, 586-587. doi:10.1007/s003830050680
- Hall, D.J. (1999) An unusual case of urinary retention due to imperforate hymen. Journal of Accident & Emergency Medicine, 16, 232-233. doi:10.1136/emj.16.3.232
- Rana, A., Manandhar, B., Amatya, A., Baral, J., Gurung, G., Giri, A. and Giri, K. (2002) Mucocolpos due to complete transverse septum in middle third of vagina in a 17-year-old girl. Journal of Obstetrics and Gynaecology Research, 28, 86-88. doi:10.1046/j.1341-8076.2002.00021.x
- Ali, A., Cetin, C., Nedim, C., Kazim, G. and Cemalettin, A. (2003) Treatment of imperforate hymen by application of Foley catheter. European Journal of Obstetrics & Gynecology and Reproductive Biology, 106, 72-75. doi:10.1016/S0301-2115(02)00214-2
- Chircop, R. (2003) A case of retention of urine and haematocolpometra. European Journal of Emergency Medicine, 10, 244-245. doi:10.1097/00063110-200309000-00019
- Liang, C.C., Chang, S.D. and Soong, Y.K. (2003) Longterm follow-up of women who underwent surgical correction for imperforate hymen. Archives of Gynecology and Obstetrics, 269, 5-8. doi:10.1007/s00404-002-0423-3
- Joki-Erkkilä, M.M. and Heinonen, P.K. (2003) Presenting and long-term clinical implications and fecundity in females with obstructing vaginal malformations. Journal of Pediatric and Adolescent Gynecology, 16, 307-312. doi:10.1016/S1083-3188(03)00157-8
- Stone, S.M. and Alexander, J.L. (2004) Images in clinical medicine. Imperforate hymen with hematocolpometra. The New England Journal of Medicine, 12, e6.
- Sakalkale, R. and Samarakkody, U. (2005) Familial occurrence of imperforate hymen. Journal of Pediatric and Adolescent Gynecology 18, 427-429. doi:10.1016/j.jpag.2005.06.008
- Nazir, Z., Rizvi, R.M., Qureshi, R.N., Khan, Z.S. and Khan, Z. (2006) Congenital vaginal obstructions: Varied presentation and outcome. Pediatric Surgery International, 22, 749-753. doi:10.1007/s00383-006-1730-8
- Walsh, B. and Shih, R. (2006) An unusual case of urinary retention in a competitive gymnast. Journal of Emergency Medicine, 31, 279-281. doi:10.1016/j.jemermed.2006.06.001
- Ambegaonkar, G. and Mulik, R. (2007) To pee or not to pee. Archives of Disease in Childhood, 92, 865. doi:10.1136/adc.2007.125203
- Acar, A., Balci, O., Karatayli, R., Capar, M. and Colakoglu, M.C. (2007) The treatment of 65 women with imperforate hymen by a central incision and application of Foley catheter. BJOG, 114, 1376-1379. doi:10.1111/j.1471-0528.2007.01446.x
- Dane, C., Dane, B., Erginbas, M. and Cetin, A. (2007) Imperforate hymen—A rare cause of abdominal pain: Two cases and review of the literature. Journal of Pediatric and Adolescent Gynecology, 20, 245-247. doi:10.1016/j.jpag.2006.12.003
- Mattern, M. and Staab, E. (2007) I-131 localization in hematocolpos: A differential diagnosis consideration for pelvic I-131 uptake. Clinical Nuclear Medicine, 32, 659-660. doi:10.1097/RLU.0b013e3180a1ad35
- Buyukbayrak, E.E., Ozyapi, A.G., et al. (2007) Imperforate hymen: A new benign reason for highly elevated serum CA 19.9 and CA 125 levels. Archives of Gynecology and Obstetrics, 277, 475-477. doi:10.1007/s00404-007-0493-3
- Kumar, K. and Waseem, M. (2008) An uncommon cause of abdominal pain in an adolescent. Southern Medical Journal, 101, 1065-1066. doi:10.1097/SMJ.0b013e31817fe318
- Adali, E., Kurdoglu, M., Yildizhan, R. and Kolusari, A. (2009) An overlooked cause of acute urinary retention in an adolescent girl: A case report. Archives of Gynecology and Obstetrics, 279, 701-703. doi:10.1007/s00404-008-0778-1
- Basaran, M., Usal, D. and Aydemir, C. (2009) Hymen sparing surgery for imperforate hymen: Case reports and review of literature. Journal of Pediatric and Adolescent Gynecology, 22, e61-e64. doi:10.1016/j.jpag.2008.03.009
- Gyimadu, A., Sayal, B., Guven, S. and Gunalp, G.S. (2009) Hematocolpos causing severe urinary retention in an adolescent girl with imperforate hymen: An uncommon presentation. Archives of Gynecology and Obstetrics, 280, 461-463. doi:10.1007/s00404-009-0931-5
- Tang, P.M., Chan, K.W., et al. (2009) Imperforate hymen: Cause of lower abdominal pain in teenage girls. Singapore Medical Journal, 50, e378-e379.
- Saks, E.K., Vakili, B. and Steinberg, A.C. (2009) Primary amenorrhea with an abdominal mass at the umbilicus. Journal of Pediatric and Adolescent Gynecology, 22, e1-e3. doi:10.1016/j.jpag.2008.07.016
- Dennie, J., Pillay, S., Watson, D. and Grover, S. (2010) Laparoscopic drainage of hematocolpos: A new treatment option for the acute management of a transverse vaginal septum. Fertility and Sterility, 94, 1853-1857. doi:10.1016/j.fertnstert.2009.09.041
NOTES
*Corresponding author.

