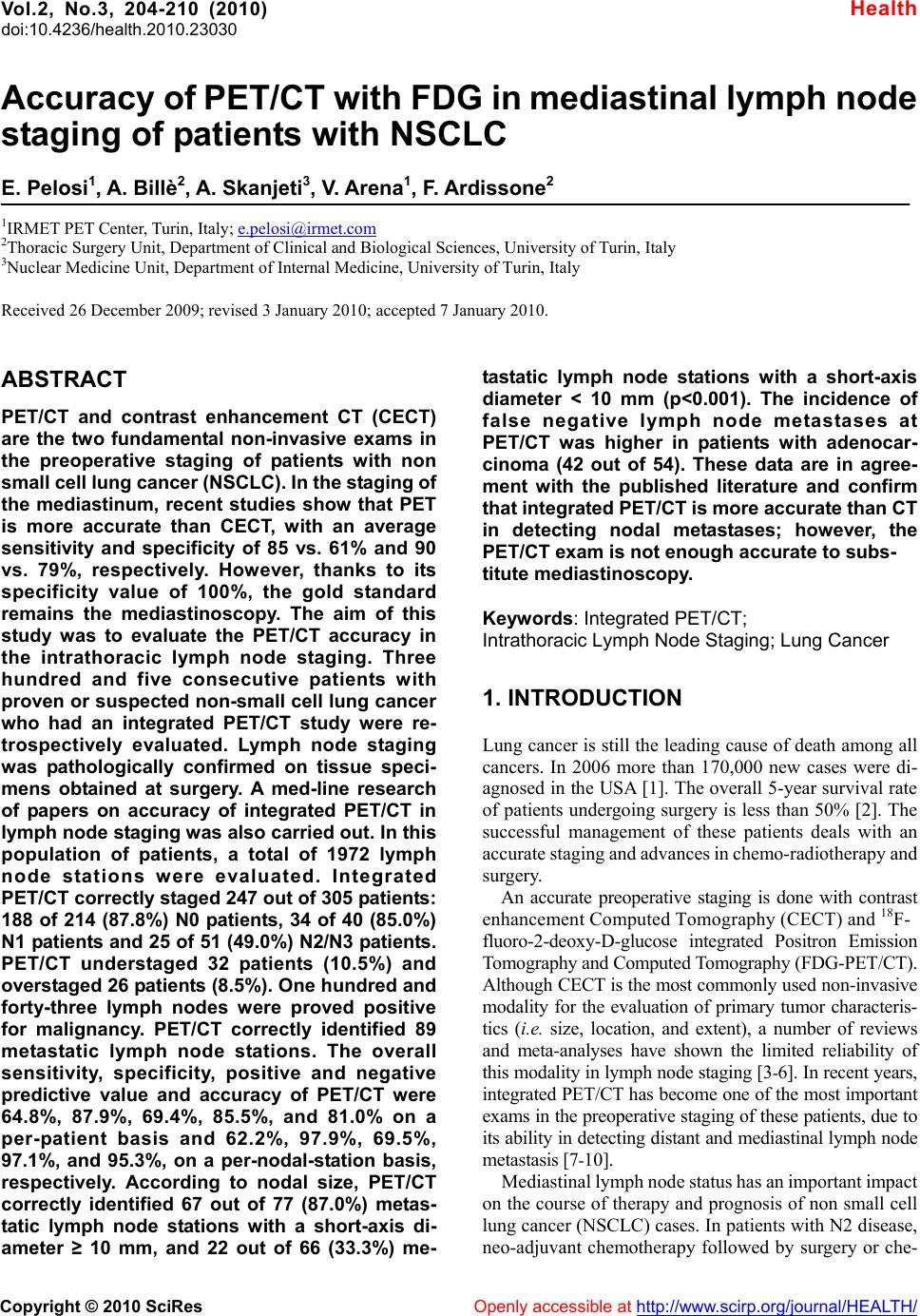
 Vol.2, No.3, 204-210 (2010) doi:10.4236/health.2010.23030 Copyright © 2010 SciRes Openly accessible at http://www.scirp.org/journal/HEALTH/ Health Accuracy of PET/CT with FDG in mediastinal lymph node staging of patients with NSCLC E. Pelosi1, A. Billè2, A. Skanjeti3, V. Arena1, F. Ardissone2 1IRMET PET Center, Turin, Italy; e.pelosi@irmet.com 2Thoracic Surgery Unit, Department of Clinical and Biological Sciences, University of Turin, Italy 3Nuclear Medicine Unit, Department of Internal Medicine, University of Turin, Italy Received 26 December 2009; revised 3 January 2010; accepted 7 January 2010. ABSTRACT PET/CT and contrast enhancement CT (CECT) are the two fundamental non-invasive exams in the preoperative staging of patients with non small cell lung cancer (NSCLC). In the staging of the mediastinum, recent studies show that PET is more accurate than CECT, with an average sensitivity and specificity of 85 vs. 61% and 90 vs. 79%, respectively. However, thanks to its specificity value of 100%, the gold standard remains the mediastinoscopy. The aim of this study was to evaluate the PET/CT accuracy in the intrathoracic lymph node staging. Three hundred and five consecutive patients with proven or suspected non-small cell lung cancer who had an integrated PET/CT study were re- trospectively evaluated. Lymph node staging was pathologically confirmed on tissue speci- mens obtained at surgery. A med-line research of papers on accuracy of integrated PET/CT in lymph node staging was also carried out. In this population of patients, a total of 1972 lymph node stations were evaluated. Integrated PET/CT correctly staged 247 out of 305 patients: 188 of 214 (87.8%) N0 patients, 34 of 40 (85.0%) N1 patients and 25 of 51 (49.0%) N2/N3 patients. PET/CT understaged 32 patients (10.5%) and overstaged 26 patients (8.5%). One hundred and forty-three lymph nodes were proved positive for malignancy. PET/CT correctly identified 89 metastatic lymph node stations. The overall sensitivity, specificity, positive and negative predictive value and accuracy of PET/CT were 64.8%, 87.9%, 69.4%, 85.5%, and 81.0% on a per-patient basis and 62.2%, 97.9%, 69.5%, 97.1%, and 95.3%, on a per-nodal-station basis, respectively. According to nodal size, PET/CT correctly identified 67 out of 77 (87.0%) metas- tatic lymph node stations with a short-axis di- ameter ≥ 10 mm, and 22 out of 66 (33.3%) me- tastatic lymph node stations with a short-axis diameter < 10 mm (p<0.001). The incidence of false negative lymph node metastases at PET/CT was higher in patients with adenocar- cinoma (42 out of 54). These data are in agree- ment with the published literature and confirm that integrated PET/CT is more accurate than CT in detecting nodal metastases; however, the PET/CT exam is not enough accurate to subs- titute mediastinoscopy. Keywords: Integrated PET/CT; Intrathoracic Lymph Node Staging; Lung Cancer 1. INTRODUCTION Lung cancer is still the leading cause of death among all cancers. In 2006 more than 170,000 new cases were di- agnosed in the USA [1]. The overall 5-year survival rate of patients undergoing surgery is less than 50% [2]. The successful management of these patients deals with an accurate staging and advances in chemo-radiotherapy and surgery. An accurate preoperative staging is done with contrast enhancement Computed Tomography (CECT) and 18F- fluoro-2-deoxy-D-glucose integrated Positron Emission Tomography and Computed Tomography (FDG-PET/CT). Although CECT is the most commonly used non-invasive modality for the evaluation of primary tumor characteris- tics (i.e. size, location, and extent), a number of reviews and meta-analyses have shown the limited reliability of this modality in lymph node staging [3-6]. In recent years, integrated PET/CT has become one of the most important exams in the preoperative staging of these patients, due to its ability in detecting distant and mediastinal lymph node metastasis [7-10]. Mediastinal lymph node status has an important impact on the course of therapy and prognosis of non small cell lung cancer (NSCLC) cases. In patients with N2 disease, neo-adjuvant chemotherapy followed by surgery or che-  E. Pelosi et al. / HEALTH 2 (2010) 204-210 Copyright © 2010 SciRes Openly accessible at http://www.scirp.org/journal/HEALTH/ 205 mo-radiation therapy with curative intent are the accepted treatments [11]. However, in mediastinal staging false positive PET/CT results have been reported in patients with coexistent inflammatory or infectious diseases, while, due to a still suboptimal spatial resolution, PET/CT study may be unable to identify metastatic deposits in normal-sized lymph nodes [12-17]. Mediastinoscopy, thanks to its 100% of specificity, remains the gold stan- dard exam in mediastinal nodal staging; however, it has several shortcomings including risk of morbidity and mortality and costs [18]. Due to these reasons, the medi- astinic staging algorithm combining integrated PET/ CT and invasive procedures is still under debate. The aim of this paper is to present our results about PET/CT accuracy in the mediastinal nodal staging of patients with NSCLC. 2. METHODS 2.1. Patient Characteristics and Inclusion Criteria From August 2004 to March 2009, 890 consecutive pa- tients underwent surgery (mediastinoscopy, anterior me- diastinotomy and/or thoracotomy) for suspected or pathologically proven, clinically resectable NSCLC, in our Thoracic Surgery Unit. Out of them, 305 patients (34.3%) before undergoing surgery had an integrated PET/CT. All PET studies were acquired in the same PET center using a Discovery ST scanner (GE Medical sys- tem), within 3 weeks from the surgical operation. Patients who underwent preoperative chemo or radiotherapy or who had a PET/CT negative primary tumor or who had a PET/CT in other centers were excluded. Patient charac- teristics are summarized in Table 1. All the patients of the study population had a history and physical examination, laboratory tests, spirometry, chest X ray, contrast enhanced brain, chest and upper abdomen CT and bronchoscopy to complete the pre- operative diagnostic work up. 2.2. Integrated PET/CT Before the exam, all patients provided informed written consent. Patients fasted for at least 6 h before the exam; the scanning was performed 60 min after the intravenous administration of FDG (4.5 to 5.5 MBq/kg). After de- termining the imaging field, a CT scan (140 kV, tube current 60 mA/S) was performed and it was used for both anatomical localization and for calculation of attenuation correction. Then, the PET data were acquired in 3D mode from the skull base to the pelvic floor in 8 to 9 bed posi- tions. The acquisition time for PET was 3 minutes per bed position. Coronal, sagittal, and transverse data sets were reconstructed. Coregistered scans were displayed by using dedicated software (Advantage 4.2; GE Healthcare) Table 1. Characteristics of the study population (n=305). Variable No. % Gender Male 239 78.4 Female 66 21.6 Age (years) Mean ± SD 66.5 ± 8.4 Range 37 – 86 Site Right 176 57.7 Left 129 42.3 Location Central (inner 1/3 of lung field) 100 32.8 Peripheral 205 67.2 Tumor diameter (cm) Mean ± SD 3.3 ±1.8 Range 0.5 – 13 Histology Squamous cell 77 25.2 Adenocarcinoma 183 60.0 Bronchoalveolar 6 2.0 Carcinoid # 15 4.9 Other type non-small cell lung cancer 24 7.9 Grade of differentiation Good 41 13.4 Moderate 139 45.6 Poor 125 41.0 Presence of vascular invasion Yes 80 26.2 No 225 73.8 Presence of necrosis Absent 109 35.7 Focal 106 34.8 Extended 90 29.5 Tumor SUVmax Mean ± SD 10.1 ± 9.5 Range 1.7 – 54 SD: standard deviation; SUVmax : maximum standardized uptake value # Typical n=11; Atypical n=4  E. Pelosi et al. / HEALTH 2 (2010) 204-210 Copyright © 2010 SciRes Openly accessible at http://www.scirp.org/journal/HEALTH/ 206 and integrated PET/CT data sets were prospectively evaluated in consensus by two nuclear medicine physi- cians (E.P. and V.A.) who were aware of clinical and stand-alone contrast-enhanced CT results, but blinded to the histologic findings. The maximum standardized up- take value (SUVmax) of the primary tumor was measured with a region-of-interest technique and calculated by the software according to standard formulas. Pulmonary and mediastinal lymph node stations, localised according to the classification scheme of Mountain and Dresler [19], were considered positive for metastatic spread if they showed focally increased FDG uptake (ie, uptake higher than the normal mediastinal activity). 2.3. Surgery and Histopathology All 305 patients underwent surgical staging. Thirty five patients underwent invasive mediastinal staging accord- ing with the positive results of the integrated PET/CT for N2/N3 disease. Cervical mediastinoscopy was used to sample stations 2R, 4R, 2L, 4L, and 7, and anterior me- diastinotomy was used to sample stations 5 and 6. Seven patients were excluded from subsequent surgery due to multi-station N2 disease (n=6) or N3 disease (n=1). The other 28 patients underwent invasive mediastinal staging procedure followed by thoracotomy during the same surgical session due to non metastatic mediastinal lymph nodes (n=8) or N2 minimal disease(n=20), defined as single-station, intranodal metastatic deposit. The 270 remaining patients, considered N2 lymph node negative by PET/CT, underwent thoracotomy, pulmonary resec- tion, and complete thoracic lymphadenectomy. Overall, pulmonary resections included pneumonectomy (n=19), bilobectomy (n=9), lobectomy (n=252), and segmentec- tomy (n=18). At thoracotomy, complete thoracic lym- phadenectomy was routinely performed; it consisted of en-bloc resection of all lymph nodes that were accessible in the mediastinum and hilum. Intrapulmonary lymph nodes (stations 11 and 12) were included in the resected lung specimen. At the subcarinal level, the contralateral mediastinal lymph nodes, lying on the opposite main stem bronchus, were removed in 41 patients. The pathologic review (primary tumor characteristics and lymph node status) was performed by standard tech- niques while immunohistochemistry was used when appropriate. Pathologic TNM staging was performed and disease was classified as stage IA in 89 patients (29.2%), stage IB in 91 (29.8%), stage IIA in 10 (3.3%), stage IIB in 43 (14.1%), stage IIIA in 49 (19.5%), stage IIIB in 14 and stage IV in 9 patients. 2.4. Data Analysis The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of integrated PET/CT in the assessment of intrathoracic lymph node involvement were determined by using histologic results as reference standard. Diagnostic characteristics of inte- grated PET/CT were assessed on a per-patient basis and on a per-nodal-station basis. A probability value of < 0.05 was considered statistically significant. Statistical analysis was carried out with StatSoft version 6.1 soft- ware. Finally, the results of our experience were compared with that of the literature. With the help of the Medline search engine PubMed, we reviewed the literature be- tween 2000 and 2009. The search was performed using keywords such as positron emission tomography, patho- logical staging and lung cancer. The inclusion criteria were the following: English language, full text articles, original articles (retrospective or prospective), meta- analysis. We considered studies that evaluated FDG-PET imaging for mediastinal lymph node staging and provided enough data to calculate sensitivity and specificity on a per patient analysis and on a per nodal station analysis. We analyzed the number of patients and the number of lymph node stations sampled, sensitivity, specificity, positive and negative predictive value and accuracy of PET. The articles on the accuracy of PET(/CT) in the restaging after induction radio or chemotherapy were excluded. 3. RESULTS A total of 1972 nodal stations were sampled in 305 pa- tients (6.5 stations per patient): 1421 mediastinal, 287 hilar and 264 intrapulmonary nodal stations; the mean number of lymph node dissected was 30 ± 13 per patient. At the pathological analysis 214 patients had no lymph node metastases, 40 patients showed an N1 disease, 50 an N2 disease and only one an N3 disease. Integrated PET/CT correctly staged 247 out of 305 patients; N1 disease was correctly detected by PET/CT in 34 of 40 patients (85.0%) with pathologically proven disease. N2/N3 disease was correctly determined by PET/CT in 25 of 51 patients (49.0%) with positive results on his- tologic analysis. PET/CT understaged 32 patients (10.5%). The causative factors for understaging were subcentimeter metastatic deposits in 22 patients and PET/CT inability to distinguish between large central tumors and adjacent mediastinal or pulmonary lymph nodes in 10 patients. PET/CT overstaged 26 patients (8.5%). Overstaging was due to inflammatory conditions (n=16) and silicoanthracosis (n=10). Integrated PET/CT showed an overall sensitivity of 64.8%, a specificity of 87.9%, a positive predictive value of 69.4%, a negative predictive value of 85.5%, and an accuracy of 81.0% for the detection of intrathoracic nodal metastases on a per- patient basis (Table 2). Out of 1.972 nodal stations histologically evaluated, 143 proved to be positive for malignancy. PET/CT cor- rectly identified 89 metastatic lymph node stations. 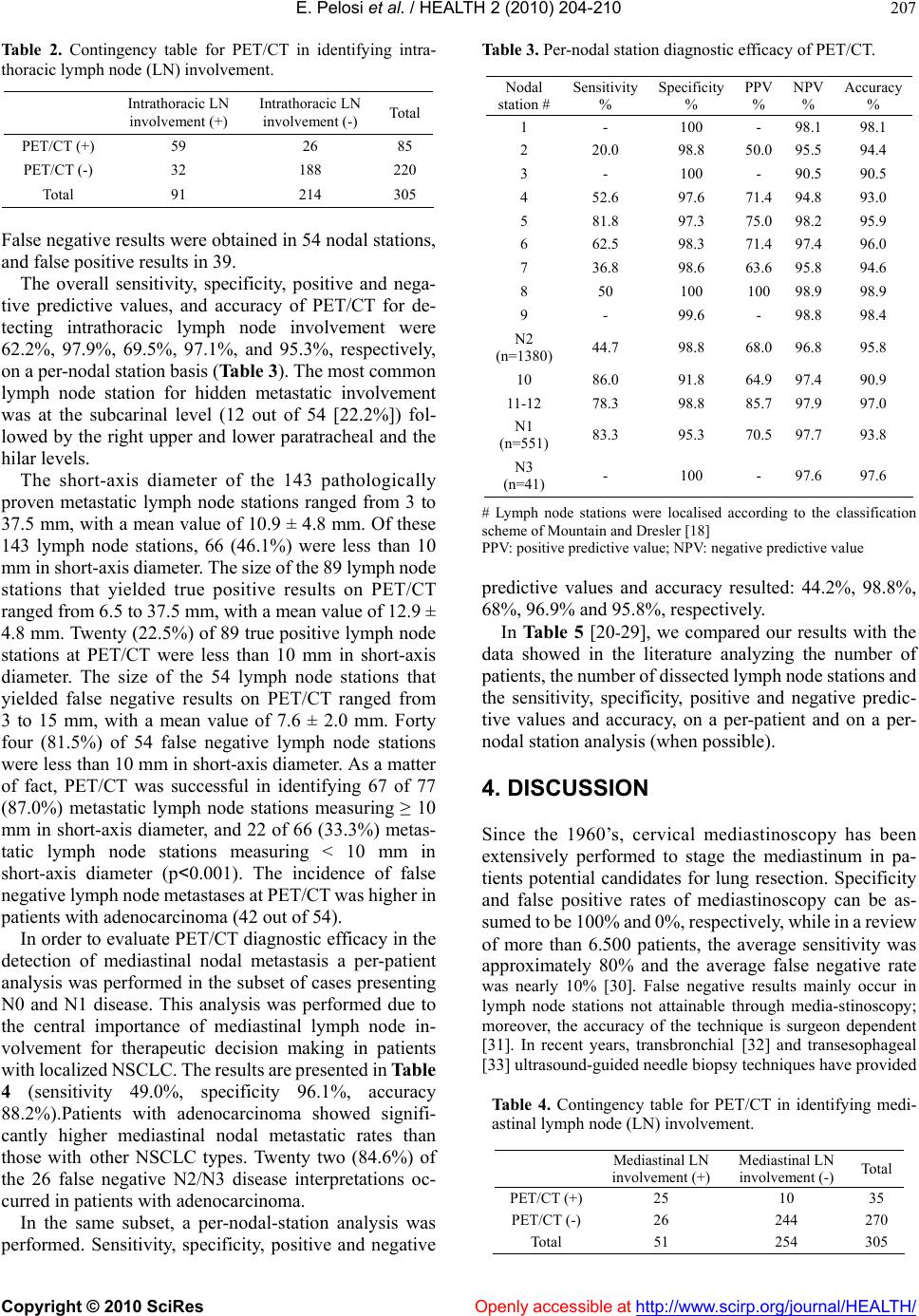 E. Pelosi et al. / HEALTH 2 (2010) 204-210 Copyright © 2010 SciRes Openly accessible at http://www.scirp.org/journal/HEALTH/ 207 Ta ble 2. Contingency table for PET/CT in identifying intra- thoracic lymph node (LN) involvement. Intrathoracic LN involvement (+) Intrathoracic LN involvement (-) Tot al PET/CT (+) 59 26 85 PET/CT (-) 32 188 220 Total 91 214 305 False negative results were obtained in 54 nodal stations, and false positive results in 39. The overall sensitivity, specificity, positive and nega- tive predictive values, and accuracy of PET/CT for de- tecting intrathoracic lymph node involvement were 62.2%, 97.9%, 69.5%, 97.1%, and 95.3%, respectively, on a per-nodal station basis (Table 3). The most common lymph node station for hidden metastatic involvement was at the subcarinal level (12 out of 54 [22.2%]) fol- lowed by the right upper and lower paratracheal and the hilar levels. The short-axis diameter of the 143 pathologically proven metastatic lymph node stations ranged from 3 to 37.5 mm, with a mean value of 10.9 ± 4.8 mm. Of these 143 lymph node stations, 66 (46.1%) were less than 10 mm in short-axis diameter. The size of the 89 lymph node stations that yielded true positive results on PET/CT ranged from 6.5 to 37.5 mm, with a mean value of 12.9 ± 4.8 mm. Twenty (22.5%) of 89 true positive lymph node stations at PET/CT were less than 10 mm in short-axis diameter. The size of the 54 lymph node stations that yielded false negative results on PET/CT ranged from 3 to 15 mm, with a mean value of 7.6 ± 2.0 mm. Forty four (81.5%) of 54 false negative lymph node stations were less than 10 mm in short-axis diameter. As a matter of fact, PET/CT was successful in identifying 67 of 77 (87.0%) metastatic lymph node stations measuring ≥ 10 mm in short-axis diameter, and 22 of 66 (33.3%) metas- tatic lymph node stations measuring < 10 mm in short-axis diameter (p<0.001). The incidence of false negative lymph node metastases at PET/CT was higher in patients with adenocarcinoma (42 out of 54). In order to evaluate PET/CT diagnostic efficacy in the detection of mediastinal nodal metastasis a per-patient analysis was performed in the subset of cases presenting N0 and N1 disease. This analysis was performed due to the central importance of mediastinal lymph node in- volvement for therapeutic decision making in patients with localized NSCLC. The results are presented in Table 4 (sensitivity 49.0%, specificity 96.1%, accuracy 88.2%).Patients with adenocarcinoma showed signifi- cantly higher mediastinal nodal metastatic rates than those with other NSCLC types. Twenty two (84.6%) of the 26 false negative N2/N3 disease interpretations oc- curred in patients with adenocarcinoma. In the same subset, a per-nodal-station analysis was performed. Sensitivity, specificity, positive and negative Table 3. Per-nodal station diagnostic efficacy of PET/CT. Nodal station # Sensitivity % Specificity % PPV % NPV % Accuracy % 1 - 100 - 98.1 98.1 2 20.0 98.8 50.0 95.5 94.4 3 - 100 - 90.5 90.5 4 52.6 97.6 71.4 94.8 93.0 5 81.8 97.3 75.0 98.2 95.9 6 62.5 98.3 71.4 97.4 96.0 7 36.8 98.6 63.6 95.8 94.6 8 50 100 100 98.9 98.9 9 - 99.6 - 98.8 98.4 N2 (n=1380) 44.7 98.8 68.0 96.8 95.8 10 86.0 91.8 64.9 97.4 90.9 11-12 78.3 98.8 85.7 97.9 97.0 N1 (n=551) 83.3 95.3 70.5 97.7 93.8 N3 (n=41) - 100 - 97.6 97.6 # Lymph node stations were localised according to the classification scheme of Mountain and Dresler [18] PPV: positive predictive value; NPV: negative predictive value predictive values and accuracy resulted: 44.2%, 98.8%, 68%, 96.9% and 95.8%, respectively. In Table 5 [20-29], we compared our results with the data showed in the literature analyzing the number of patients, the number of dissected lymph node stations and the sensitivity, specificity, positive and negative predic- tive values and accuracy, on a per-patient and on a per- nodal station analysis (when possible). 4. DISCUSSION Since the 1960’s, cervical mediastinoscopy has been extensively performed to stage the mediastinum in pa- tients potential candidates for lung resection. Specificity and false positive rates of mediastinoscopy can be as- sumed to be 100% and 0%, respectively, while in a review of more than 6.500 patients, the average sensitivity was approximately 80% and the average false negative rate was nearly 10% [30]. False negative results mainly occur in lymph node stations not attainable through media-stinoscopy; moreover, the accuracy of the technique is surgeon dependent [31]. In recent years, transbronchial [32] and transesophageal [33] ultrasound-guided needle biopsy techniques have provided Table 4. Contingency table for PET/CT in identifying medi- astinal lymph node (LN) involvement. Mediastinal LN involvement (+) Mediastinal LN involvement (-) Tot al PET/CT (+) 25 10 35 PET/CT (-) 26 244 270 Total 51 254 305  E. Pelosi et al. / HEALTH 2 (2010) 204-210 Copyright © 2010 SciRes http://www.scirp.org/journal/HEALTH/Openly accessible at 208 a valuable adjunct for the evaluation of mediastinoscopic “blind spots”. Apart from the fact that mediastinoscopy is unable to completely stage the mediastinum, it also pre- sents several shortcomings which include invasiveness, risk of morbidity and mortality, and costs. As a conse- quence, different imaging techniques have been proposed as a guide to enable the most efficient use of medi- astinoscopy. Several studies clearly demonstrate the key role of PET with FDG in the preoperative staging of patients with NSCLC, due to its ability in detecting local and distant metastases. In a recent meta-analysis FDG-PET resulted more accurate than CECT in identifying mediastinal nodal metastases [29]. The average sensitivity and speci- ficity of CECT were 61% and 79%, respectively, while 85% and 90%, respectively for PET [34]. With the in- troduction of PET/CT, as shown for the first time by Lardinois et al., the accuracy in detecting local and dis- tant metastases has even increased [7,27]. However, fur- ther studies have not confirmed these preliminary results (see Table 5 [12-17,20]). Therefore at present the sensi- tivity and accuracy of PET/CT in the mediastinal lymph node staging are considered too low to avoid further invasive studies [28], and the role of PET and medi- astinoscopy is under discussion. Our study confirms the limited ability of integrated PET/CT in identifying the actual intrathoracic lymph node stage of patients with potentially resectable NSCLC. All the performance characteristics of integrated PET/CT turned out to be below the threshold of 95%, only where the test could replace invasive staging procedures [17]. In fact, we had 10.5% of false negative and 8.5% of false positive cases. A high rate of false negative patients for N2 disease in the adenocarcinoma group was identified, as with other authors [35]. Observing the available literature, we can notice a certain heterogeneity in the methods: some authors did not perform a per patient and a per nodal station analysis, and/or did not report the number of the sampled stations, and/or the average number of the dissected lymph nodes. Anthoc et al. reported that integrated PET/CT was more accurate than CECT in the overall tumor staging but also in identifying nodal metastases of patients with non-small lung cancer [8]. The sensitivity, specificity and accuracy were 89%, 94% and 93%, respectively. The authors explain that the advantage of integrated PET/CT is due to the exact spatial localization of the abnormal uptakes in the mediastinum and suggest that a mediasti- num negative for nodal metastasis at the PET/CT study doesn’t require any further diagnostic surgical procedure such as mediastinoscopy. On the contrary, Yi et al. in their study analyzed 453 mediastinal nodal stations and demonstrated that the PET/CT sensitivity is not high enough in identifying metastases. These authors stressed the need to continue to perform mediastinoscopy also in stage T1, N0 patients, despite its high cost and associated morbidity and mor- tality. Curiously, in this study PET/CT showed very high specificity levels leading the authors to conclude that mediastinoscopy should not be performed in patients with a positive PET/CT [15]. Turkmen in 2007 reported the higher accuracy of PET/CT over CT and PET alone in detecting mediastinal nodal metastases, but the accuracy was not enough to replace the mediastinoscopy as the gold standard: on 59 patients he reported a sensitivity of 76% and an accuracy of 80%. He pointed out that the causes of PET false negative cases were micro-metastases, necrosis and PET limited spatial resolution [36]. De Langen showed that in PET negative lymph nodes of 10 to 15 mm the probability of discovering nodal me- tastases is too low to justify mediastinoscopy. In con- clusion he stressed the necessity to identify the subset of patients with a negative PET/CT, that could benefit from a mediastinoscopy [25-37]. Lee et al. reported that PET/CT did not improve the overall accuracy of mediastinal staging due to the fact that, the improvement in technology, reduced the number Table 5. Integrated PET/CT sensibility and specificity. Characteristic Patients (No.) LN stations (No.)Sensibility (%)Specificity (%)PPV (%) NPV (%) Accuracy (%) Our series 305 6.5 64.8 87.9 69.4 85.5 81 Melek et al. [20] 170 4.04 74 73 55 87 74 Perigaud et al. [21] 51 3.8 40 85 40 85 - Port et al. [22] 64 - 45 89 - - - Nomori et al. [23] 80 - 78 98 74 98 97 Cerfolio et al. [9]* 129 N/A 69 94 49 99 96 Cerfolio et al. [24] 400 - 71 77 44 91 76 Gupta et al. [25] 77 - 87 91 72 97 82 Poncelet et al. [26] 64 - 67 85 43 94 82 Pieterman et al.* [27] 102 - 91 86 95 74 87 Kim et al. [28] 150 3.8 47 100 100 87 88 Yi et al. [29] 143 3.2 56 100 100 88 90 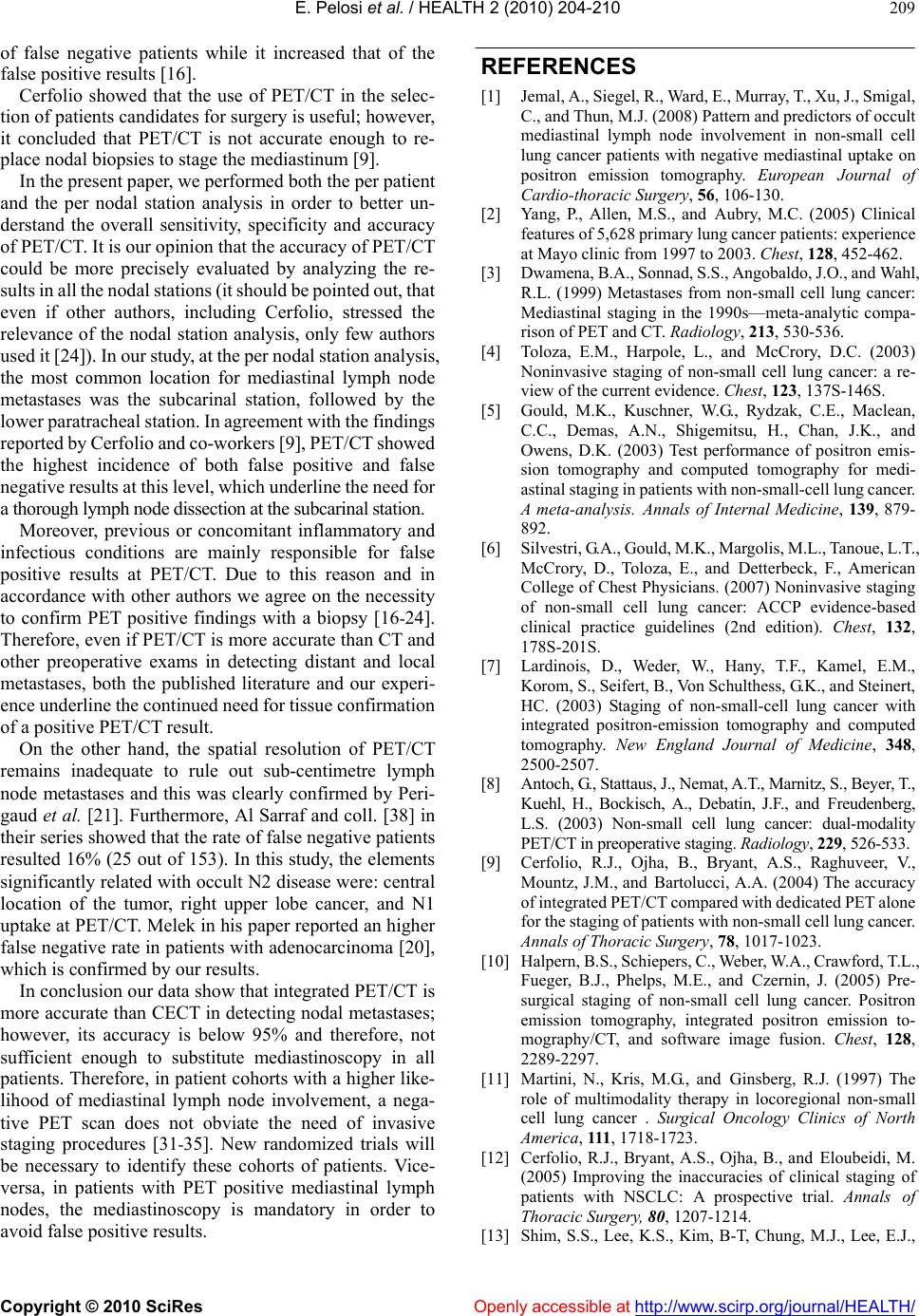 E. Pelosi et al. / HEALTH 2 (2010) 204-210 Copyright © 2010 SciRes Openly accessible at http://www.scirp.org/journal/HEALTH/ 209 of false negative patients while it increased that of the false positive results [16]. Cerfolio showed that the use of PET/CT in the selec- tion of patients candidates for surgery is useful; however, it concluded that PET/CT is not accurate enough to re- place nodal biopsies to stage the mediastinum [9]. In the present paper, we performed both the per patient and the per nodal station analysis in order to better un- derstand the overall sensitivity, specificity and accuracy of PET/CT. It is our opinion that the accuracy of PET/CT could be more precisely evaluated by analyzing the re- sults in all the nodal stations (it should be pointed out, that even if other authors, including Cerfolio, stressed the relevance of the nodal station analysis, only few authors used it [24]). In our study, at the per nodal station analysis, the most common location for mediastinal lymph node metastases was the subcarinal station, followed by the lower paratracheal station. In agreement with the findings reported by Cerfolio and co-workers [9], PET/CT showed the highest incidence of both false positive and false negative results at this level, which underline the need for a thorough lymph node dissection at the subcarinal station. Moreover, previous or concomitant inflammatory and infectious conditions are mainly responsible for false positive results at PET/CT. Due to this reason and in accordance with other authors we agree on the necessity to confirm PET positive findings with a biopsy [16-24]. Therefore, even if PET/CT is more accurate than CT and other preoperative exams in detecting distant and local metastases, both the published literature and our experi- ence underline the continued need for tissue confirmation of a positive PET/CT result. On the other hand, the spatial resolution of PET/CT remains inadequate to rule out sub-centimetre lymph node metastases and this was clearly confirmed by Peri- gaud et al. [21]. Furthermore, Al Sarraf and coll. [38] in their series showed that the rate of false negative patients resulted 16% (25 out of 153). In this study, the elements significantly related with occult N2 disease were: central location of the tumor, right upper lobe cancer, and N1 uptake at PET/CT. Melek in his paper reported an higher false negative rate in patients with adenocarcinoma [20], which is confirmed by our results. In conclusion our data show that integrated PET/CT is more accurate than CECT in detecting nodal metastases; however, its accuracy is below 95% and therefore, not sufficient enough to substitute mediastinoscopy in all patients. Therefore, in patient cohorts with a higher like- lihood of mediastinal lymph node involvement, a nega- tive PET scan does not obviate the need of invasive staging procedures [31-35]. New randomized trials will be necessary to identify these cohorts of patients. Vice- versa, in patients with PET positive mediastinal lymph nodes, the mediastinoscopy is mandatory in order to avoid false positive results. REFERENCES [1] Jemal, A., Siegel, R., Ward, E., Murray, T., Xu, J., Smigal, C., and Thun, M.J. (2008) Pattern and predictors of occult mediastinal lymph node involvement in non-small cell lung cancer patients with negative mediastinal uptake on positron emission tomography. European Journal of Cardio-thoracic Surgery, 56, 106-130. [2] Yang, P., Allen, M.S., and Aubry, M.C. (2005) Clinical features of 5,628 primary lung cancer patients: experience at Mayo clinic from 1997 to 2003. Chest, 128, 452-462. [3] Dwamena, B.A., Sonnad, S.S., Angobaldo, J.O., and Wahl, R.L. (1999) Metastases from non-small cell lung cancer: Mediastinal staging in the 1990s—meta-analytic compa- rison of PET and CT. Radiology, 213, 530-536. [4] Toloza, E.M., Harpole, L., and McCrory, D.C. (2003) Noninvasive staging of non-small cell lung cancer: a re- view of the current evidence. Chest, 123, 137S-146S. [5] Gould, M.K., Kuschner, W.G., Rydzak, C.E., Maclean, C.C., Demas, A.N., Shigemitsu, H., Chan, J.K., and Owens, D.K. (2003) Test performance of positron emis- sion tomography and computed tomography for medi- astinal staging in patients with non-small-cell lung cancer. A meta-analysis. Annals of Internal Medicine, 139, 879- 892. [6] Silvestri, G.A., Gould, M.K., Margolis, M.L., Tanoue, L.T., McCrory, D., Toloza, E., and Detterbeck, F., American College of Chest Physicians. (2007) Noninvasive staging of non-small cell lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest, 132, 178S-201S. [7] Lardinois, D., Weder, W., Hany, T.F., Kamel, E.M., Korom, S., Seifert, B., Von Schulthess, G.K., and Steinert, HC. (2003) Staging of non-small-cell lung cancer with integrated positron-emission tomography and computed tomography. New England Journal of Medicine, 348, 2500-2507. [8] Antoch, G., Stattaus, J., Nemat, A.T., Marnitz, S., Beyer, T., Kuehl, H., Bockisch, A., Debatin, J.F., and Freudenberg, L.S. (2003) Non-small cell lung cancer: dual-modality PET/CT in preoperative staging. Radiology, 229, 526-533. [9] Cerfolio, R.J., Ojha, B., Bryant, A.S., Raghuveer, V., Mountz, J.M., and Bartolucci, A.A. (2004) The accuracy of integrated PET/CT compared with dedicated PET alone for the staging of patients with non-small cell lung cancer. Annals of Thoracic Surgery, 78, 1017-1023. [10] Halpern, B.S., Schiepers, C., Weber, W.A., Crawford, T.L., Fueger, B.J., Phelps, M.E., and Czernin, J. (2005) Pre- surgical staging of non-small cell lung cancer. Positron emission tomography, integrated positron emission to- mography/CT, and software image fusion. Chest, 128, 2289-2297. [11] Martini, N., Kris, M.G., and Ginsberg, R.J. (1997) The role of multimodality therapy in locoregional non-small cell lung cancer . Surgical Oncology Clinics of North America, 111, 1718-1723. [12] Cerfolio, R.J., Bryant, A.S., Ojha, B., and Eloubeidi, M. (2005) Improving the inaccuracies of clinical staging of patients with NSCLC: A prospective trial. Annals of Thoracic Surgery, 80, 1207-1214. [13] Shim, S.S., Lee, K.S., Kim, B-T, Chung, M.J., Lee, E.J.,  E. Pelosi et al. / HEALTH 2 (2010) 204-210 Copyright © 2010 SciRes Openly accessible at http://www.scirp.org/journal/HEALTH/ 210 Han, J., Choi, J.Y., Kwon, O.J., Shim, Y.M., and Kim, S. (2005) Non-small cell lung cancer: prospective compari- son of integrated FDG PET/CT and CT alone for preop- erative staging. Radiology, 236, 1011-1019. [14] Kim, B-T, Lee, K.S., Shim, S.S., Choi, J.Y., Kwon, O.J., Kim, H., Shim, Y.M., Kim, J., and Kim, S. (2006) Stage T1 non-small cell lung cancer: preoperative mediastinal nodal staging with integrated FDG PET/CT — a pro- spective study. Radiology, 241, 501-509. [15] Yi, C.A., Lee, K.S., Kim, B-T, Shim, S.S., Chung, M.J., Sung, Y.M., and Jeong, S.Y. (2007) Efficacy of helical dynamic CT versus integrated PET/CT for detection of mediastinal nodal metastasis in non-small cell lung cancer. Australian Journalism Review, 188, 318-325. [16] Lee, B.E., Von Haag, D., Lown, T., Lau, D., Calhoun, R., and Follette, D. (2007) Advances in positron emission tomography technology have increased the need for sur- gical staging in non-small cell lung cancer. Journal of Thoracic and Cardiovascular Surgery, 133, 746-752. [17] Tournoy, K.G., Maddens, S., Gosselin, R., Van Maele, G., Van Meerbeeck, J.P., and Kelles, A. (2007) Integrated FDG-PET/CT does not make invasive staging of the in- trathoracic lymph nodes in non-small cell lung cancer redundant: a prospective study. Thorax, 62, 696-701. [18] Hammound, Z.T., Anderson, R.C., Meyers, B.F., Guthrie, T.J., Roper, C.L., Cooper, J.D., and Patterson, G.A. (1999) The current role of mediastinoscopy in the evaluation of thoracic disease. Journal of Thoracic and Cardiovascular Surgery, 118, 894-899. [19] Mountain, C.F., and Dresler, C.M. (1997) Regional lymph node classification for lung cancer staging. Chest, 111, 1718-1723. [20] Melek, H., Gunluoglu, M.Z., Demir, A., Akin, H., Olcmen, A., and Dincer, S.I. (2008) Role of positron emission to- mography in mediastinal lymphatic staging of non-small cell lung cancer. European Journal of Cartiothoracic Surgery, 33, 294-299. [21] Perigaud, C., Bridji, B., Roussel, J.C., Sagan, C., Mugniot, A., Duveau, D., Baron, O., and Despins, P. (2009) Pro- spective preoperative mediastinal lymph node staging by positron emission tomography computerized tomography in patients with non-small-cell lung cancer. European Journal of Cartiothoracic Surgery, 36,731-736. [22] Port, J.L. (2005) Positron emission tomographic scanning in the diagnosis and staging of non-small cell lung cancer 2 cm in size or less. Journal of Thoracic and Cardiovas- cular Surgery, 130, 611-615 [23] Nomori, H., Watanabe, K., Ohtsuka, T., Naruke, T., Sue- masu, K., Kobayashi, T., and Uno, K. (2004) Fluorine 18-tagged fluorodeoxyglucose positron emission tomo- graphy scanning to predict lymph node metastasis, inva- siviness, or both in clinical T1 N0 M0 lung adenocarci- noma. Journal of Thoracic and Cardiovascular Surgery, 128, 396-401. [24] Cerfolio, R.J., Ojha, B., Briant, A.S., Brass, C.S., Barta- lucci, A.A., and Mountz, J.M. (2003) The role of FDG- PET scan in staging patients with non small cell carci- noma. Annals of Thoracic Surgery, 76, 861-866 [25] Gupta, N.C. (2001) Mediastinal lymph node sampling following positron emission tomography with fluoride- oxyglucose imagin gin lung cancer staging. Chest, 120, 521-527. [26] Poncelet, A.J., Lonneux, M., Coche, E., Weynand, B., and Moirhomme, Ph. (2001) FDG-PET scan enhances but does not replace surgical staging in non-small cell lung carcinoma. European Journal of Cartiothoracic Surgery, 20, 468-475. [27] Pieterman, R.M. (2000) Preoperative staging of non-small cell lung cancer with positron-emission tomography. New England Journal of Medicine, 343, 254-261. [28] Kim, B-T, Lee, K.S., Shim, S.S., Choi, J.Y., Kwon, O.J., Kim, H., Shim, Y.M., Kim, J., and Kim, S. (2006) Stage T1 non-small cell lung cancer: preoperative mediastinal nodal staging with integrated FDG PET/CT —a prospec- tive study. Radiology, 241, 501-509. [29] Yi, C.A., Lee, K.S., Kim, B-T, Shim, S.S., Chung, M.J., Sung, Y.M., and Jeong, S.Y. (2007) Efficacy of helical dynamic CT versus integrated PET/CT for detection of mediastinal nodal metastasis in non-small cell lung cancer. Australian Journalism Review, 188, 318-325. [30] Detterbeck, F.C., Jantz, M.A., Wallace, M., Vansteenkiste, J., Silvestri, G.A. (2007) Invasive mediastinal staging of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest, 132, 202S-220S. [31] Smulders, S.A., Smeenk, FWJW, Janssen-Heijnen, MLG, Wielders, PLML, de Munck, DRAJ, and Postmus, P.E. (2005) Surgical mediastinal staging in daily practice. Lung Cancer, 47, 243-251. [32] Herth, F.J., Eberhardt, R., Vilmann, P., Krasnik, M., and Ernst, A. (2006) Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling me- diastinal lymph nodes. Thorax, 61, 795-798. [33] Annema, J.T., Versteegh, M.I., Veseliç, M., Welker, L., Mauad, T., Sont, J.K., Willems, L.N., and Rabe, K.F. (2005) Endoscopic ultrasound added to mediastinoscopy for preoperative staging of patients with lung cancer. Journal of Clinical Investigation, 294, 931-936. [34] Behzadi, A., Ung, Y., Lowe, V., and Deschamps, C. (2008) The role of positron emission tomography in the man- agement of non-small cell lung cancer. Canadian Journal of Cardiology, 3, 235-242. [35] Al-Sarraf, N., Aziz, R., Doddakula, K., Gately, K., Wilson, L., McGovern, E., and Young, V. (2006) Factors causing inaccurate staging of mediastinal nodal involvement in non-small cell lung cancer patients staged by positron emission tomography. Interactive CardioVascular and Thoracic Surgery. [36] Turkman, C., Sommezoglu, K., and Toker, A. (2007) The additional value of FDG PET imaging for distinguishing N0 or N1 from N2 stage in preoperative staging of non-small cell lung cancer in region where the prevalence of inflam- matory lung disease is high. Nuclear Medicine, 32, 607-612. [37] De Langen, A.J., Raijmakers, P., and Riphagen, I. (2006) The size of mediastinal lymph nodes and its relation with metastatic involvement: A meta-analysis. European Jour- nal of Cartiothoracic Surgery, 29, 26-29. [38] Al-Sarraf, N., Aziz, R., Gately, K., Lucey, J., Wilson, L., McGovern, E., and Young, V. (2008) Pattern and predic- tors of occult mediastinal lymph node involvement in non-small cell lung cancer patients with negative medi- astinal uptake on positron emission tomography. Euro- pean Journal of Cartiothoracic Surgery, 33,104-109.
|