Journal of Behavioral and Brain Science
Vol. 2 No. 1 (2012) , Article ID: 17737 , 4 pages DOI:10.4236/jbbs.2012.21014
Efficacy of Multimodal Intervention for Children with Attention Deficit Hyperactivity Disorder (ADHD)—An Indian Study
1School of Psychology and Social Work, University Malaysia Sabah, Kota Kinabalu, Malaysia
2Department of Clinical Psychology, National Institute of Mental Health and Neuro Sciences (NIMHANS), Bangalore, India
3Department of Psychiatry, National Institute of Mental Health and Neuro Sciences (NIMHANS), Bangalore, India
Email: rejanigopal@yahoo.co.in
Received August 11, 2011; revised October 13, 2011; accepted October 24, 2011
Keywords: Multimodal Intervention; ADHD; Attention Enhancement Training; Parent Training
ABSTRACT
Background: To find the efficacy of multimodal intervention on attention deficit and hyperactivity, behavioral problems in home and school situations and on academic achievement of children with ADHD and the impact of family stress and coping on the outcome of multi-modal intervention. Method: A sample (N = 40) of children aged 5 - 10 years registered in the Child and Adolescent Mental Health Unit (CAMHU) with a diagnosis of ADHD (on the ICD-10) with or without comorbidity were randomly allocated to one of two groups: Group I (medical management with parent counseling, N = 20) or Group II (multimodal intervention (routine medical management, parent training and attention enhancement training), N = 20). Assessments (pre-assessment, re-assessment at one month and post assessment after 10 weeks) were carried out by investigator, parent, teacher and blind rater. Results: Significant improvement was noticed for both groups but multimodal intervention was superior to routine medical management and parent counselling in reducing ADHD symptoms, behavioural problems at home and school, and in improving academic performance. Effect size estimates and the rates of clinically significant change also supported this finding. Parental stress did not predict the outcome of intervention. Conclusions: Multimodal intervention was found to be promising in the treatment of ADHD.
1. Introduction
Though a wide variety of treatments have been used for ADHD, It is generally agreed in the empirical literature that only three treatments have been validated as effecttive short-term treatments for ADHD: behaviour modifycation, central nervous system stimulants and the combination of these. In general, multimodal treatment is recommended [1,2].
Studies focused on the efficacy of stimulant treatment, psychosocial treatments, combination of medication and psychosocial treatments, and the multimodal studies showed conflicting results. Some studies found superiority of pharmacological treatment over psychosocial treatment/ multimodal intervention in reducing core symptoms of ADHD, behavioural problems, academic performance and social skills [3-6] while others found vice versa [7-9].
Parents of children with ADHD very often experience considerable stress in their parenting roles. The severity of parental stress affects the perception of their child’s problem [10] and affects the adherence to treatment [11]. The association between parental stress and coping on outcome of intervention is not fully known.
In recognition of these facts, the present study examines the efficacy of multi-modal and pharmacological interventions on attention deficit and hyperactivity, behaveioural problems in home and school situations and on academic achievement. It was also aimed to study the impact of family stress and coping on the outcome of multimodal intervention.
2. Method
The study has conducted in two phases: Pilot study and the main study. Pilot study was conducted to find out the suitability of tools and the feasibility of intervention package.The procedure for the main study was as follows: After the routine screening and detailed work up in the CAMHU, those who met the ICD-10 criteria for ADHD, with or without comorbidity and fulfilled the inclusion (children aged—10 years, school going children and off medication for at least one year if they had epilepsy) and exclusion( presence of significant head injury, evidence of neuro infections, presence of pervasive developmental disorder and presence of psychosis) criteria of the present study were screened on Conners Abbreviated Rating Scale (CARS) and those who scored above the cutoff point (15 and above) were tested on Binet-Kamat Test of intelligence (BKT). Those who got an IQ of 70 or above were given the consent form and explained about the therapeutic procedure.
Totally 180 children were screened and 79 cases were found suiting the criteria and from that 27 cases were excluded from the study after the pre-intervention screening procedures. They were (N = 52) further rated on Assessment of Genetics Interview for Children-Parent version (MAGIC-P), Detailed Evaluation Schedule for Children and Adolescents-1 (DESCA-1), ADHD Rating Scale and Colour Cancellation Test (CCT). Following parent’s rating on ADHD Rating Scale (HSQ) and class teacher’s ratings on ADHD Rating Scale, Barkley’s School Situations Questionnaire (SSQ) and Academic Performance Rating Scale (APRS).They were randomly allotted to Group I (Multimodal intervention) and Group II (Medical management with parent counseling). Re-assessment was carried out at the end of end month of intervention by the investigator with ADHD Rating Scale and CCT, parent was interviewed with ADHD Rating Scale and HSQ, and teacher used ADHD Rating Scale, SSQ and APRS. Post assessment was done at the end of two and half months by the investigator, blind rater, parent and teacher with the pre-assessment tools.12 children were removed/dropped out from the study during the intervention period and thus 20 cases were completed in each group.
2.1. Details of the Tools Used for Screening, Pre-Assessment, Re-Assessment and Post-Assessment
Screening measures:
1) Conners Abbreviated Rating Scale (CARS) [12]: consists of ten items which are rated on a four point scale.
2) Binet Kamat Test of Intelligence [13] was used for the assessment of intellectual functions which is an Indian adaptation of the Standford Binet scale of intelligence.
Pre-intervention diagnostic interview: Missouri Assessment of Genetics Interview for Children-Parent version (MAGIC-P) [14] was used for making formal diagnosis and assessing comorbidity. It is a semi-structured psychiatric interview schedule for parents that assess the presence, absence and duration of child symptoms based on the Diagnostic and Statistical Manual of Mental Disorders-3rd and 4th edition (DSM III-R and DSM-IV).
Tool for assessing demographic details: Detailed Evaluation Schedule for Children and Adolescents-1 (DESCA-1) [15]: It obtains information on socio-demographic factors. Most of the questions were coded in Yes (1)/No (2)/or Not known (3) format.
2.2. Outcome Evaluation
Color Cancellation Test [16]: The tool was used for assessing attention, concentration and impulsivity of the children. It also assesses sustained and focused attention. Both single and double color cancellations were used.
ADHD Rating Scale [17]: It consists of 14 items assessing the core symptoms of ADHD which are rated on a four-point scale from 0 to 3 (0 = not at all, 1 = just a little, 2 = pretty much, 3 = very much). It has separate scoring keys for both parent and teacher ratings. Subscales include Inattention-Hyperactivity and Impulsivity -Hyperactivity. In the present study the investigator along with parent and teacher used the scale to measure the severity of ADHD and used the parent-rating key for the investigators rating. For parent rating, r = 0.94 for total score and that for teacher rating was 0.96 [17].
Academic Performance Rating Scale [18]: It is a teacher rating scale to assess the child’s academic performance in the following areas: learning ability, impulse control, academic performance and social withdrawal. It has 19 items which were rated on a five-point scale ranging from 1 to 5. It gives a total score of academic performance and four subscale scores. The internal consistency for the total scale was found to be 0.95 and test retest reliabilities was 0.95 [18].
Barkley’s School Situations Questionnaire (SSQ) [19]: It assesses situational variation in child behaviour within the school setting. The child’s misbehaviour in 11 specific situations are rated by the teacher on a 9 point scale where one indicates mild and nine indicates an extreme degree of problem. Two measures are obtained: the number of problem settings and their mean severity rating. Reported SSQ stability estimates range from 0.64 to 0.82 with a median value of 0.77, alpha co-efficients range from 0.84 to 0.91 with a median value of 0.85 [20].
Barkley’s Home Situations Questionnaire (HSQ) [19]: This is a 16-item parent completed rating scale designed to assess situational variation in child behaviour within the home setting. Presence of misbehaviour in 16 specific situations is rated on a 9-point scale (mild = 1; 9 = severe). Alpha co-efficients of this scale were ranged from 0.82 to 0.87 with a median value of 0.88 [20]. Two scores are obtained: number of problem situations and the mean severity rating of these problems.
Family Assessment Schedule [21]: It is a semi-structured interview schedule, which assesses the stress, experienced (perceived) by families caring for a child with mental retardation and coping resources available for the family, which are likely to modify the perceived stress (mediators). Certain items were modified to suit ADHD in the present study. The coefficients of measures of reliability of the tool range from 0.36 to 0.9 and co-efficient of validity measures are 0.51 to 0.63 [22].
2.3. Details of the Intervention Package
Medication management: Medication used was Methylphenidate (MPH) or Clonidine as decided by the Psychiatry Consultant. The dosage and side effects were monitored by the senior residents of the CAMH unit at the end of 2nd week, 4th week, and 10th week and on follow-ups. The frequency of consultation for monitoring medication was similar for both groups.
Parent counseling consisted of psycho-education regarding ADHD, which included nature of illness, etiology, prognosis and the side effects of medication. Parents were asked about their understanding about the illness and the therapist clarified their doubts related to the illness. Support and encouragement were given during their medication maintenance visits.
Attention enhancement training: Following tasks were included in the attention enhancement package: colouring, grain sorting, clay modelling, mazes, beading and matching figures based on empirical evidence in improving attention deficit and impulsivity [23-27]. All these tasks were arranged on the level of difficulty levels. The tasks were introduced in weekly sessions.
Parent training was conducted by using the manual: Defiant children-A clinician’s manual for parent training [28]. It is a ten step programme consisting of explanation of causes of ADHD, teaching principles of behavioural management, tasks for enhancing parental attending skills, establishing home token systems, using response cost, improving school behaviour, managing child’s behaviour in public places and handling future behaviour problems. It spread over ten weekly sessions of one-hour duration.
3. Results
3.1. Analysis
The quantitative analysis of data was done using Statistical Package for Social Sciences 11.5 version for windows (SPPS 11.5). t-tests were used to compare the means of the Group I and Group II for the significance of the difference at pre-assessment, re-assessment and post-assessment on variables such as inattention and hyperactiveity, behavioural problems at home and school, academic performance and stress and coping. Totally three paired comparisons were made (pre-to re-assessment, re-to postassessment and pre-to post-assessment) and a Bonferroni correction for the level of significance was used to reduce the likelihood of a type I error. The level of signifycance (0.05) was divided by 3 (no. of paired comparisons) which yielded an alpha level p £ 0.016 and this value is used to interpret the results.
Repeated measures analysis was carried out to assess the time into the group interaction across the assessments within the group and between two treatment conditions. Effect sizes were calculated to find out the magnitude of change in two treatment conditions on various outcome variables. Both with-in group and between group effect sizes were calculated. Within-group effect sizes for each outcome measure were calculated using formula by Cohen [29]. Unbiased estimates of effect sizes were calculated to correct for the small sample size [30]. The effect size is considered as small (0.2 ≤ ES < 0.5), medium (0.5 ≤ ES < 0.8), large (≥0.8). Effect size could be very large if variability within the measured groups is low, even if there was little change brought by therapy [31]. So an additional method called clinical significance is used to evaluate the treatment by using specific formula [31-33].
Simple linear regression analysis was done to find the predictive factors of outcome. Total score of parental stress and mediators of stress (coping strategies) at preassessment were entered as independent variables, and total and subscale scores on ADHD Rating Scale and total scores on HSQ (both scales rated by parent) at re and post-assessment as dependant variables.
3.2. Demographic and Clinical Details
There was no significant difference on variables such as age (t = 1.557, p = 0.128) sex (p = 1.000), education (t = 1.038, p = 0.306), religion and rural/urban background (p = 1.000). On DESCA-1, 25% of the sample was found to have pure ADHD, 40% in each group had comorbidity with ODD, 50% in each group had SLD, 55% of the sample had dull normal borderline intelligence and 77.5% of the sample had psychosocial adversities. Psychiatric problems were present among fathers (15%) and mothers (12.5%). There were no statistically significant difference was found between the groups on clinical variables at baseline.
3.3. The Effectiveness of Intervention
3.3.1. Severity of ADHD
Statistically significant difference was found in both within & between group comparison of ratings by investigator, parent & teacher on repeated measures analysis of variance for both groups and more changes were noticed for GI (Tables 1 and 5). Blind rater rating was highly correlated with investigator and parent rating for total and subscale scores but not with teacher rating in both groups.
Large effect size was noticed for total and subscale scores on the ratings of investigator, parent and teacher for GI (Table 3). Clinical Significance change also showed 100% clinically significant change (on total Score) for GI by investigator and parent (Table 4).
3.3.2. Attention Deficit
Repeated measures of variance (0.000 for GI & 0.609 for GII), Wilcoxon Signed-rank test and effect size (0.49) indicated that GI showed more improvement in double colour cancellation (Table 1). High correlation with blind rater (r = 1.00) increases the validity of the result.
3.3.3. Behavioral Problems at Home
Repeated measures of variance (0.000 for GI & 0.628 GII and 0.000 for between Group comparison), independent and paired sample test shows statistically significant changes for both groups (p = 0.000 for between and within comparison) (Table 2). Magnitude of clinical change was more for GI (ES was 1.41 for GI and 0.10 for GII) (Table 3) and clinical significant change also showed more improvement for GI (Table 4). High correlation was found with blind rater rating (0.96 for GI & 0.99 for GII).
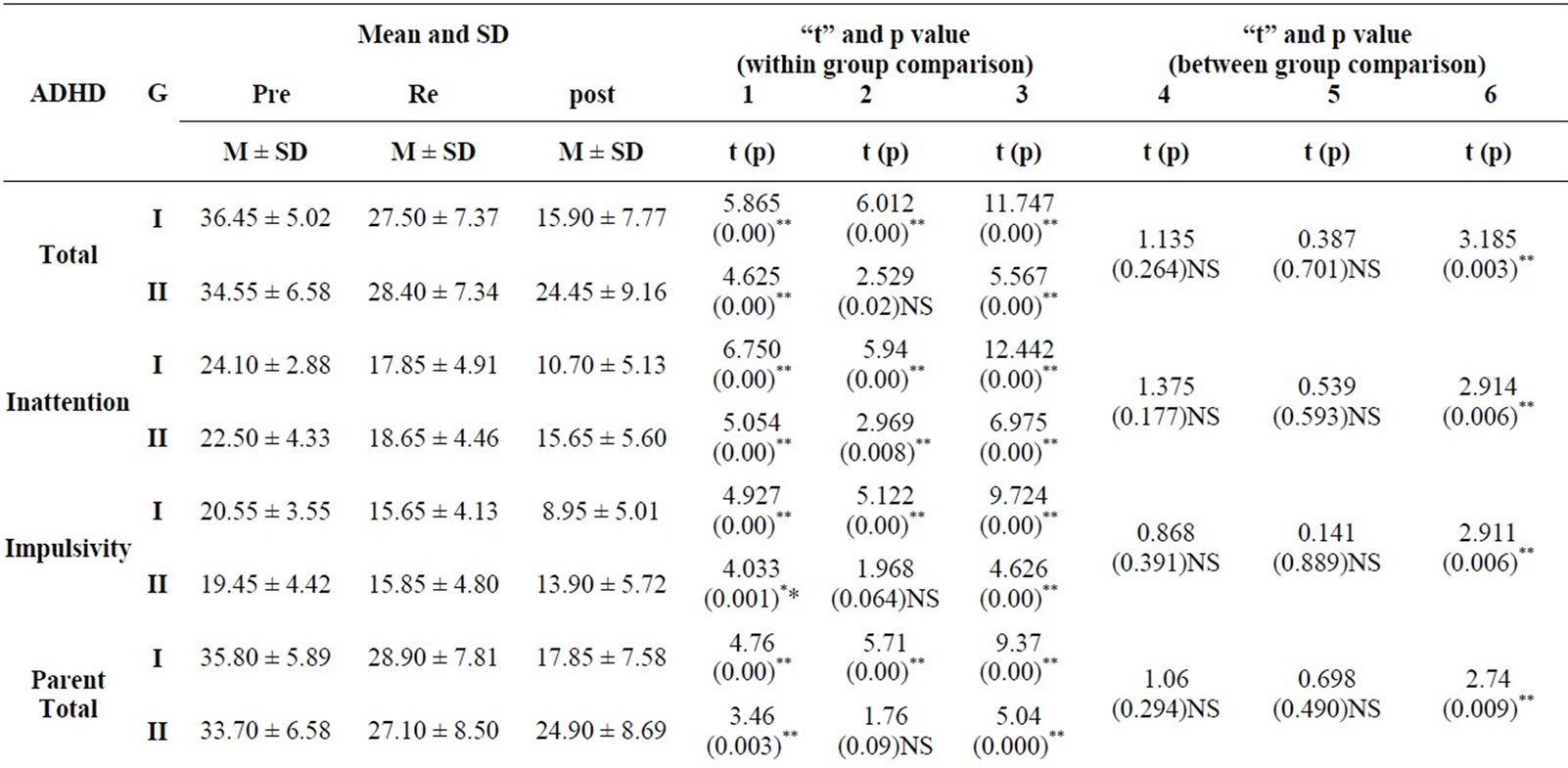
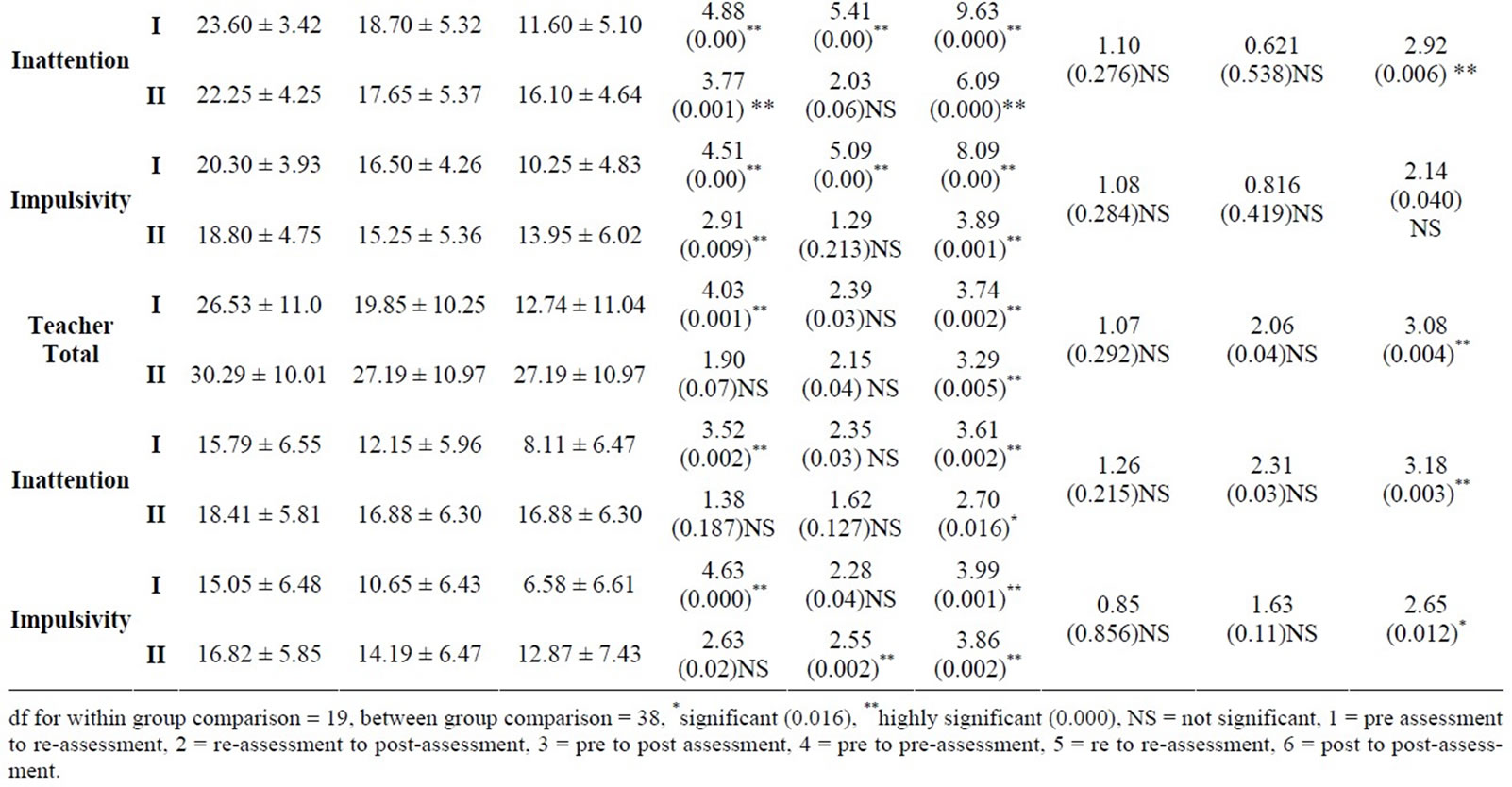
Table 1. Means, SDs, and t-values between and within two groups on ADHD Rating Scale (Rated by the Investigator, parent and teacher).
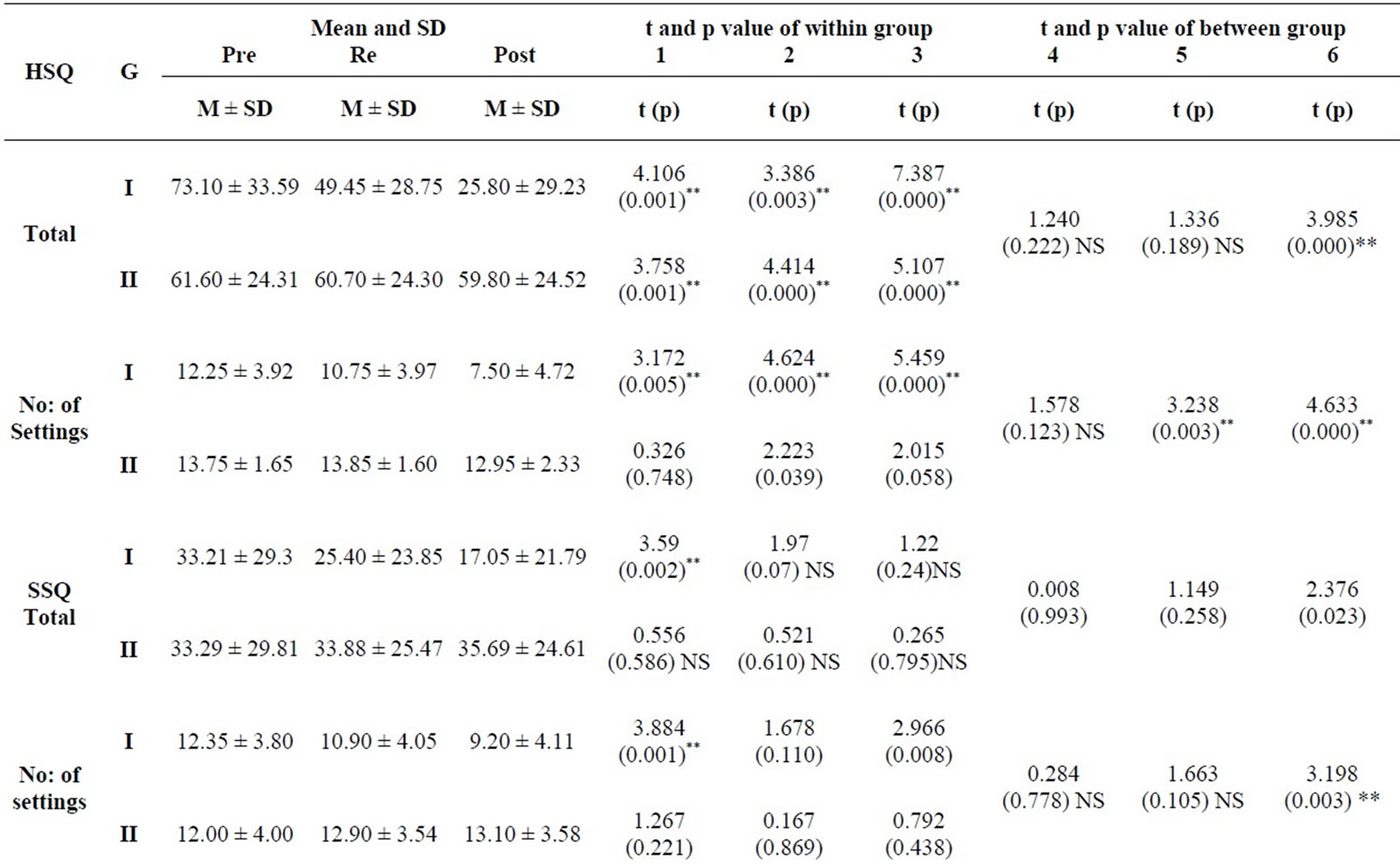
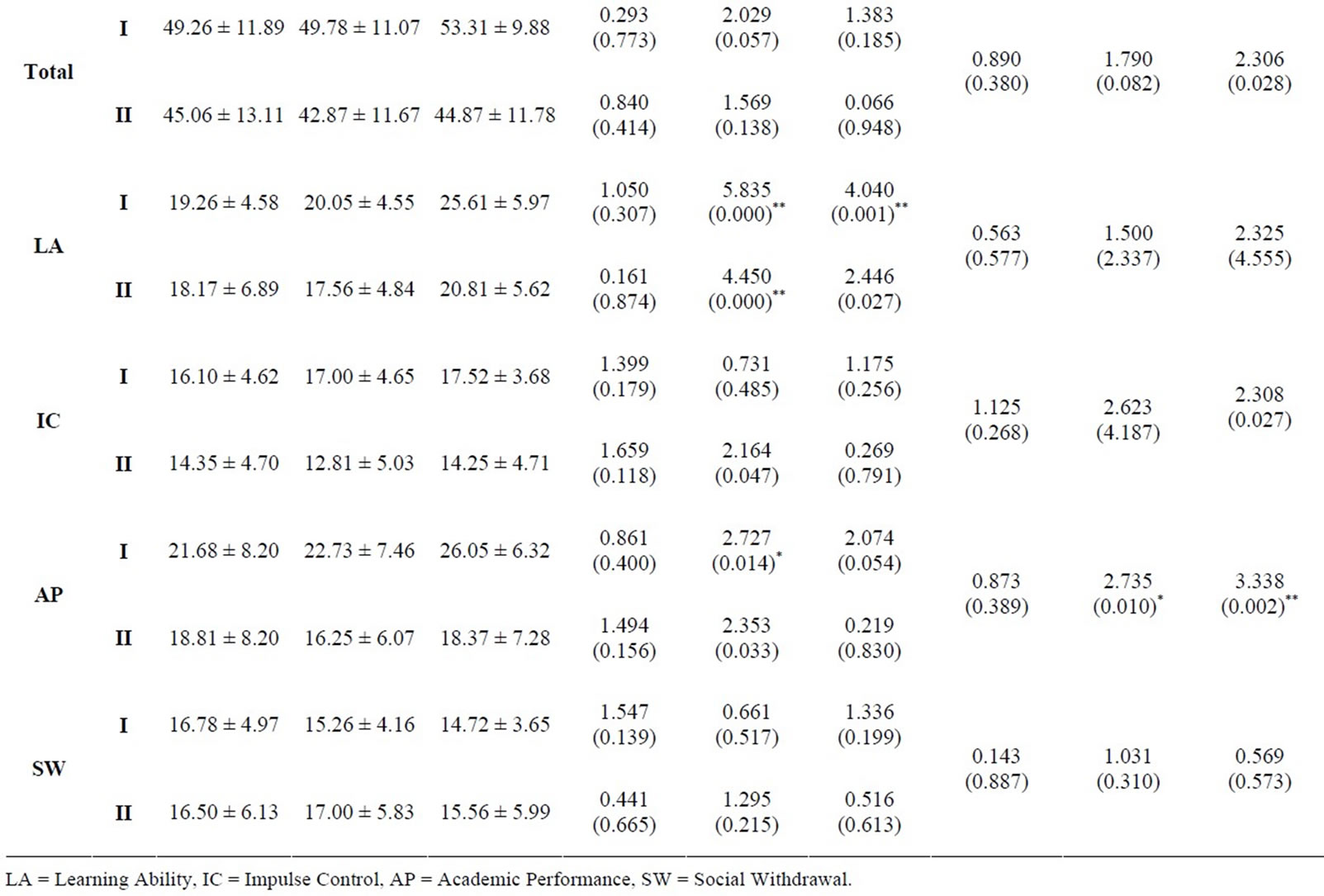
Table 2. Means, SDs, and t-values between and within two groups on HSQ, SSQ and APRS.
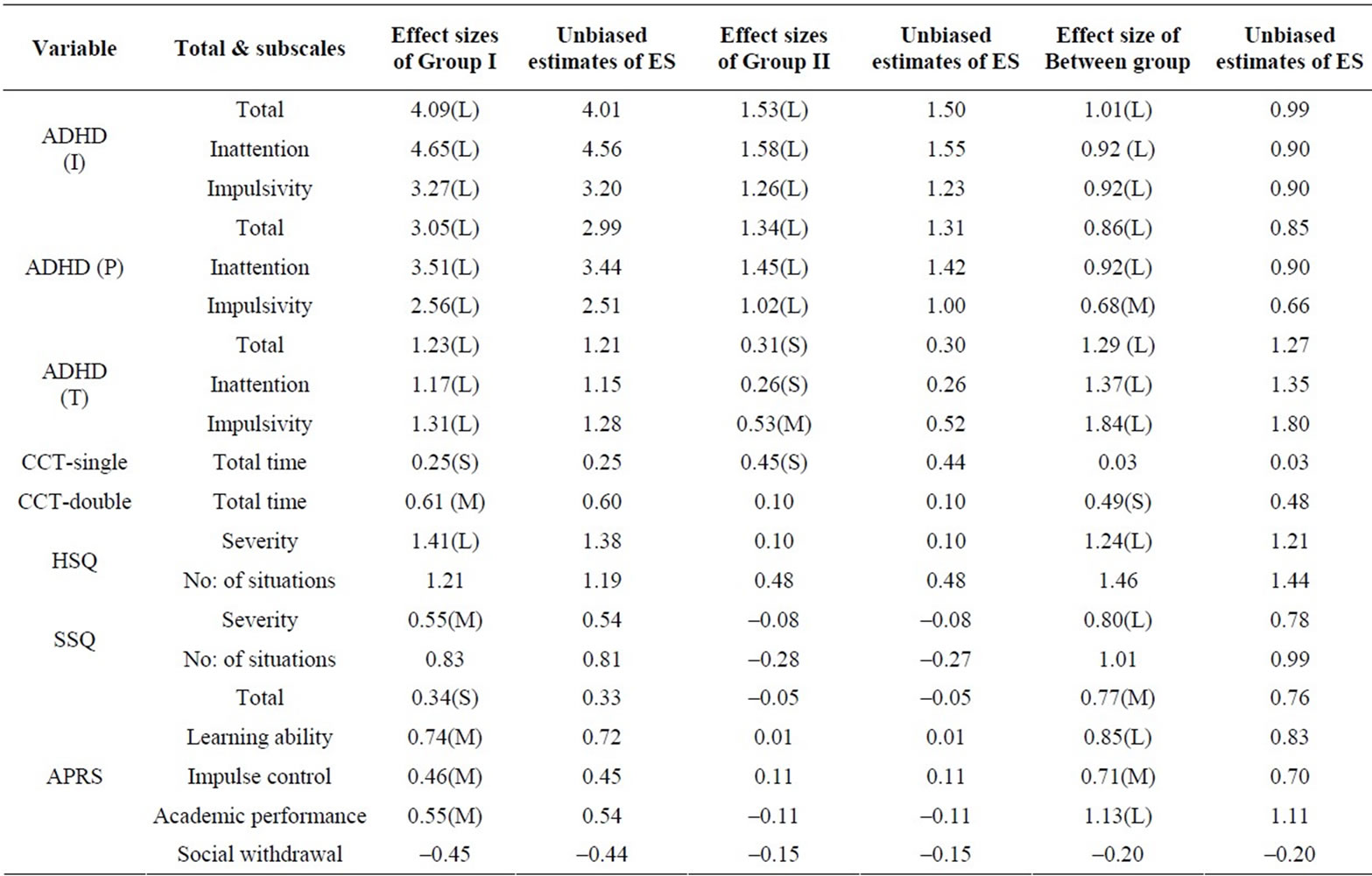
Table 3. Within and between effect sizes on the outcome variables across the groups.
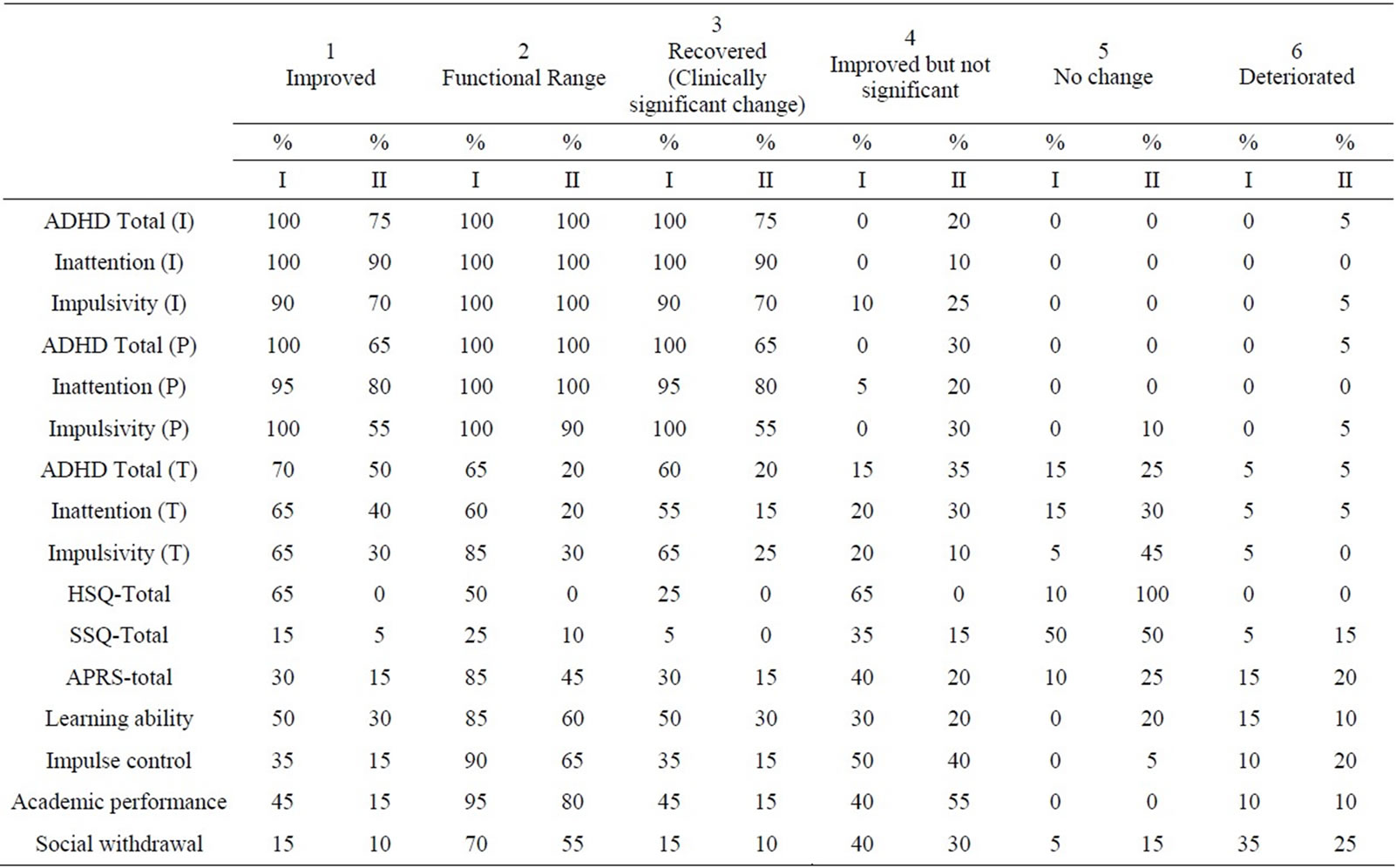
Table 4. Percentage of children showing clinically significant change on the outcome measures in the two groups.
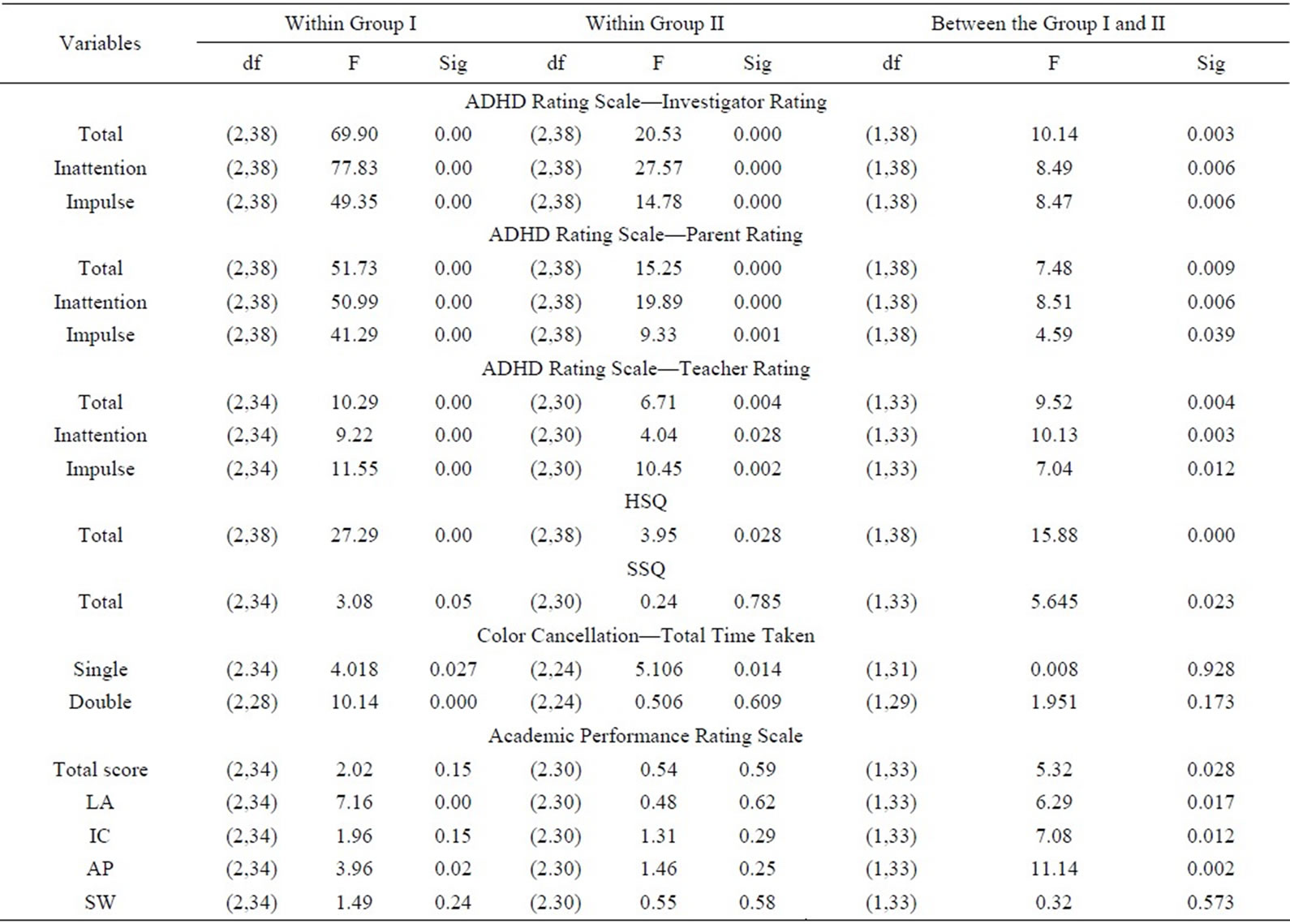
Table 5. F-values of repeated measures analysis of variance on the outcome variables across the groups.
3.3.4. Behavioural Problems at School
Repeated measures analysis of variance, “t” tests, effect size and clinically significant change showed superiority of multimodal intervention (Table 2). Effect size was 0.55 (M) for GI and 0.08 for GII (Table 3). 5% recovered, 15% improved in GI: 15% deteriorated and none showed clinically significant change in GII (Table 4).
3.3.5. Academic Performance
Repeated measures of analysis of variance, “t” tests, effect size and clinical significance showed superiority of multimodal intervention on learning ability, impulse control, academic performance and social withdrawal (Independent sample test: p = 0.002 for academic performance; paired sample test: p = 0.001 for GI & 0.027 for learning ability) (Table 2).
3.3.6. Impact of Family Stress and Coping on Outcome
Predictive factors of outcome were analyzed by linear regression and the independent variables considered were total score of stress and mediators obtained on FAS at pre-assessment. It was found that the pre-treatment parental stress did not predict severity of ADHD symptoms and behavioural problems at post assessment for both groups.
4. Discussion
Analysis showed statistically significant changes in both Groups on ADHD symptoms but multimodal intervenetion was superior (Group I). Literature shows the evidence of improved efficacy of multimodal/combined intervention over medical management alone for reducing the core symptoms of ADHD [9,34-36]. The improvement shown by Group II goes well with existing literature that short-term trials of psycho stimulants are effective in reducing the core symptoms of ADHD [37,38]. Clonidine is also proven effective in treating children with ADHD [39]. In the present study, 12 children were on MPH and 8 children on clonidine, from each group. More improvement in Group I could be due to the inclusion of attention enhancement package which was found effective in improvement of core symptoms of ADHD especially inattention. On attention measure, improvement in committing errors of omission and commission in colour cancellation was also noticed for Group I. It could be due to the improvement that occurred in sustained attention, visual scanning and impulsivity which are impaired in children with ADHD. The attention enhancement training given to Group I might have improved these deficits as the tasks in the attention package were targeted to improve same. The impact of medical management combined with parent training in improving attention and impulsivity are also well documented in literature [25]. However, the present study could not assess the contribution of each treatment component in improveing these deficits due to methodological limitations On ADHD rating scale, ratings of investigator and parent were correlates well with the blind rater at post assessment while it is not correlating with the teacher rating. This may be partially explained by the difference in the scoring keys used. The scoring key used for parent and investigator rating were same where as it was different for the teachers rating. The differences in the outcome reported by different informants with different parameters were reported in many studies. It was suggested that outcome measures completed by parents may be tapping a source of information regarding therapy effecttiveness different from the one sampled by data collected by independent observers [40]. Low correlation between informants may indicate that the target variables differ from one situation to another, rather than that informants’ reports are invalid or unreliable [41].
The result of improvement in behavioral problems at home goes well with the literature that parent training reduces behavioural problems at home [28,42-44]. The above studies reported that parent training is effective for reducing behavioural problems in ADHD as well as behavioural problems associated with conduct disorder, oppositional defiant disorder and such comorbid conditions that were present in the sample. Studies also report that pharmacological intervention especially with psycho stimulants is effective in reducing behavioural problems in ADHD and its comorbid conditions [4,45,46]. So the improvement shown by Group I in the behavioral problems of the children in home situations also could be due to pharmacological intervention, as they have undergone psycho stimulant treatment in addition to parent training. This might have added to the benefits of parent training.
Result also showed improvement of behavioral problems at school for Group I. This could be due to the monitoring of the behavioral problems by the teacher and the implementation of contingency management by the parent based on the daily report card sent by the teacher. This was done as a part of parent training which was included in the multimodal intervention. Literature has shown that behavior modification improves oppositional behaveior, positive and social behavior and peer conflicts in the classroom [3,4,47].
When compared to improvements in behavioural problems in the home situation, improvements that occurred in school situations were less. This could be due to the active participation in intervention and close monitoring of behavioural problems by the parents compared to less participation by the teachers.
Improvement in academic performance in Group I is consistent with a wealth of research that multimodal intervention is effective in improving academic functions [9]. The uses of psycho stimulants in improving academic functions of ADHD children were also well documented [48,49]. Improvement in academics and social behavior was reported in studies used attention enhancement tasks [25,24]. So it is not possible to pin point which treatment component yielded more improvement.
Though parental stress did not predict the outcome, the present study reported that parental stress predicted increased severity level of ADHD (r2 = 0.124, p = 0.026*) and behaviour of problems (r2 = 0.397, p = 0.000*) at pre-intervention stage. It is well documented in literature that high level of parental stress is associated with severe ADHD symptoms, defiant behaviour, difficult temperament and problematic interaction on ADHD children with their siblings [50,51].
5. Conclusions
Multimodal intervention was found to be promising in the treatment of ADHD. It was found to be effective in reducing ADHD symptoms, behavioural problems at home and school and in improving academic performance. Parental stress did not predict the outcome.
5.1. Strengths of the Study
The study used fresh cases, random allocation, and parallel design, ratings were done by multiple informants and therapeutic inputs were given by clinician, parents and school personnel in multimodal treatment. Developmentally appropriate and most frequently and commonly used tools in the area of ADHD research were used for this study. The use of MAGIC-P enhanced the diagnostic validity and rating by blind rater at post-assessment increased the validity of the results. Manual based parent training and structured attention enhancement package were ensured uniformity in treatment. On ethicalback ground, all children in medical management group were provided with parent training and attention enhancement training after the intervention period of the study.
5.2. Limitations of the Study
The study has small sample size. Color Cancellation Test taps a particular aspect of the attention deficit and the use of tools to assess different dimensions of attention would have been more informative, especially the kind of change that occurred in attention after the intervention.
5.3. Implications of the Study
Multimodal intervention was found superior in the treatment of ADHD. The use of attention enhancement tasks for improving attention and reducing impulsivity and hyperactivity was promising. Though the exact nature of neuropsychological mechanism is not known, the package was found useful. This study highlights the importance of using different modalities in the treatment of ADHD while considering its high comorbid condition.
REFERENCES
- B. J. Coffey, “Attention Deficit Disorder,” In: J. D. Noshpitz, P. F. Kernberg and J. R. Bemporad, Eds., Handbook of Child and Adolescent Psychiatry, John Wiley and Sons, Inc., New York, 1997.
- National Institute of Health Consensus Development Conference Statement, “Diagnosis and Treatment of Attention Deficit Hyperactivity Disorder (ADHD),” Journal of American Academy of Child and Adolescent Psychiatry, Vol. 39, No. 2, 2000, pp. 182-193.
- W. E .Pelham, C. Carlson, S. E. Sams, V. G. Dixon and B. Hoza, “Separate and Combined Effects of Methylphenidate and Behaviour Modification on Boys with Attention Deficit Hyperactivity Disorder in the Classroom,” Journal of Consulting and Clinical Psychology, Vol. 61, No. 3, 1993, pp. 506-515. doi:10.1037/0022-006X.61.3.506
- D. J. Kolko, O. G. Bukstein and J. Barron, “Methylphenidate and Behaviour Modifications in Children with ADHD and Comorbid ODD or CD; Main and Incremental Effects across Settings,” Journal of the American Academy of Child and Adolescent Psychiatry, Vol. 38, No. 5, 1999, pp. 578-586. doi:10.1097/00004583-199905000-00020
- MTA Cooperative Group, “A 14-Month Randomized Clinical Trial of Treatment Strategies for Attention-Deficit/ Hyperactivity Disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD,” Archives of General Psychiatry, Vol. 56, No. 12, 1999, pp. 1073-1086.
- R. G. Klein, H. Abikoff, L. Hechtman and G. Weiss, “Design and Rationale of Controlled Study of Long-Term Methylphenidate and Multi-Modal Psychosocial Treatment in Children with ADHD,” Journal of the American Academy of Child and Adolescent Psychiatry, Vol. 43, No. 7, 2004, pp. 792-801. doi:10.1097/01.chi.0000128798.91601.fe
- M. D. Rapport, H. A. Murphy and J. S. Bailey, “Ritalin vs. Response Cost in the Control of Hyperactive Children: A Within-Subject Comparison,” In: P. E. Nathan and J. M. Gorman, Eds., A Guide to Treatments That Work, Oxford University Press, New York, 1982.
- W. F. Horn, N. S. Ialongo, J. M. Pascoe, G. A. Greenberg, T. Packard, M. Lopez, A. Wagner and L. Puttler, “Addictive Effects of Psychostimulants, Parent Training and SelfControl Therapy with ADHD Children,” Journal of the American Academy of Child and Adolescent Psychiatry, Vol. 30, No. 2, 1991, pp. 233-240. doi:10.1097/00004583-199103000-00011
- J. H. Satterfield, B. T. Satterfield and D. P. Cantwell, “Multimodality Treatment. A Two Year Evaluation of 61 Hyperactive Boys,” Archives of General Psychiatry, Vol. 37, No. 8, 1980, pp. 915-919. doi:10.1001/archpsyc.1980.01780210073007
- E. A. Schaughency and B. B. Lahey, “Mother’s and Father’s Perceptions of Child Deviance: Roles of Child Behavior, Parental Depression, and Marital Satisfaction,” Journal of Consulting and Clinical Psychology, Vol. 53, No. 5, 1985, pp. 718-723. doi:10.1037/0022-006X.53.5.718
- R. Calam, C. Bolton and J. Roberts, “Maternal Expressed Emotion, Attributions and Depression and Entry into Therapy for Children with Behavioural Problems,” British Journal of Clinical Psychology, Vol. 41, No. 2, 2002, pp. 213-216. doi:10.1348/014466502163985
- C. K. Conners, “Rating Scales for Use in Drug Studies with Children,” Psychopharmacology Bulletin (Special Issue on Children), Vol. 24, 1973, pp. 24-29.
- V. V. Kamat, “Measuring Intelligence of Indian Children,” Oxford University Press, London, 1967.
- W. Reich, P. M. Licht, H. Lehman, S. Sathyan and K. Unger, “Missouri Assessment of Genetics Interview for Children (MAGIC),” Washington University, Division of Child Psychiatry, St. Louis, 1997.
- S. Srinath, M. Kovacs, S. C. Girimaji, S. P. Seshadri, “Detailed Evaluation Schedule for Children and Adolescents,” 1991, Unpublished Manuscript.
- M. Kapur, “Measurement of Organic Brain Dysfunction,” Ph.D. Thesis, Bangalore University, Bangalore, 1974.
- G. J. Dupaul, “Parent and Teacher Ratings of ADHD Symptoms: Psychometric Properties in a Community Based Sample,” Journal of Clinical Child Psychology, Vol. 20, No. 3, 1991, pp. 245-253. doi:10.1207/s15374424jccp2003_3
- G. J. Dupaul, M. D. Rapport and L. M. Perviello, “Teacher Ratings of Academic Skills: The Development of the Academic Performance Rating Scale,” School Psychology Review, Vol. 20, No .2, 1991, pp. 284-300.
- R. A. Barkley, “Hyperactive Children: A Handbook for Diagnosis and Treatment,” Guilford Press, New York, 1981.
- T. S. Altepeter and M. J. Breen, “Situational Variation in Problem Behaviour at Home and School in Attention Deficit Disorder with Hyperactivity: A Factor Analytic Study,” Journal of Child Psychology and Psychiatry and Allied Disciplines, Vol. 33, No. 4, 1992, pp. 741-752. doi:10.1111/j.1469-7610.1992.tb00909.x
- S. C. Girimaji, “Counsellors Manual for Family Intervention in Mental Retardation,” Indian Council of Medical Research, New Delhi, 1996.
- S. C. Girimaji, S. Srinath, S. Seshadri and S. Krishna, “Family Interview for Stress and Coping in Mental Retardation (FISC-MR): A Tool to Study Stress and Coping in Families of Children with Mental Retardation,” Indian Journal of Psychiatry, Vol. 41, No. 4, 1999, pp. 341-349.
- N. Agarwal and S. L. Rao, “Neuropsychological Remediation in Hyperactive Children,” Indian Journal of Psychiatry, Vol. 39, No.4, 1997, pp. 309-312.
- H. V. Oberoi and M. Kapur, “Intervention with Hyperkinetic Boys in the School Setting,” NIMHANS Journal, Vol. 13, No. 1, 1995, pp. 123-131.
- S. Basu and A. Deb, “Parent Training in Children with Attention Deficit Hyperactivity Disorder: An Integrated Approach for Greater Effectiveness,” Indian Journal of Clinical Psychology, Vol. 23, No. 1, 1996, pp. 184-191.
- M. D. Lezak, “Neuro Psychological Assessment,” Oxford University Press, New York, 1995.
- G. Plourde, Y. Joanette and P. Fontaine, “The Two Forms of Visual Spatial Neglect,” Journal of Clinical and Experimental Neuropsychology, Vol. 10, No. 2, 1988, p. 317.
- R. A. Barkley, “Defiant Children: A Clinician’s Manual for Assessment and Parent Training,” Guilford Press, New York, 1997.
- J. Cohen, “Statistical Power Analysis for the Behavioural Sciences,” Erlbaum, New Jersey, 1988.
- H. V. Hedges and I. Olkin, “Statistical Methods for MetaAnalysis,” Academic Press, Orlando, 1985.
- N. S. Jacobson and P. Truax, “Clinical Significance: A Statistical Approach to Defining Meaningful Change in Psychotherapy Research,” Journal of Consulting and Clinical Psychology, Vol. 59, No. 1, 1991, pp. 12-19. doi:10.1037/0022-006X.59.1.12
- N. S. Jacobson, W. C. Follette, D. Revenstorf, D. H. Baucom, K. Hahlweg and G. Margolin, “Variability in Outcome and Clinical Significance of Behavioural Marital Therapy: A Reanalysis of Outcome Data,” Journal of Consulting and Clinical Psychology, Vol. 52, No. 4, 1984, pp. 497-504. doi:10.1037/0022-006X.52.4.497
- L. Christensen and J. L. Mendoza, “A Method of Assessing Change in a Single Subject: An Alteration of the RC Index,” Behaviour Therapy, Vol. 17, No. 3, 1986, pp. 305- 308. doi:10.1016/S0005-7894(86)80060-0
- S. P. Hinshaw, B. Henker and C. K. Whalen, “CognitiveBehavioural and Pharmacologic Interventions for Hyperactive Boys: Comparative and Combined Effects,” Journal of Consulting and Clinical Psychology, Vol. 52, No. 5, 1984, 739-749. doi:10.1037/0022-006X.52.5.739
- J. M. Langberg, L. E. Arnold, A. M. Flowers, J. N. Epstein, M. Altaye, S. P. Hinshaw, J. M. Swanson, R. Kotkin, S. Simpson, B. S. Molina, P. S. Jensen, H. Abikoff, W. E. Pelham Jr., B. Vitiello, K. C. Wells and L. Hechtman, “Parent-Reported Homework Problems in the MTA Study: Evidence for Sustained Improvement with Behavioral Treatment,” Journal of Clinical Child and Adolescent Psychology, Vol. 39, No. 2, 2010, pp. 220-233. doi:10.1080/15374410903532700
- E. H. Nieweg, “Does ADHD Medication Stop Working after 2 - 3 Years? On the Surprising, but Little-Known Follow-Up of the MTA Study,” Tijdschrift Voor Psychiatrie, Vo. 52, No. 4, 2010, pp. 245-254.
- J. P. Zrull, J. C. Westman, B. Arthur and D. Rice, “A Comparison of Diazepam, D-Amphetamine and Placebo in the Treatment of the Hyperkinetic Syndrome in Children,” American Journal of Psychiatry, Vol. 121, 1964, pp. 388- 389.
- C. K. Conners and E. Taylor, “Pemoline, Methylphenidate and Placebo in Children with Minimal Brain Dysfunction,” Archives of General Psychiatry, Vol. 37, No. 8, 1980, pp. 922-930. doi:10.1001/archpsyc.1980.01780210080009
- P. Choudhary, S. Girimaji, S. Srinath and S. P. Seshadri, “An Open Trial of Clonidine for Hyperkinesis in Children with Mental Retardation and Epilepsy,” Indian Journal of Psychological Medicine, Vol. 16, No. 1, 1993, pp. 41-44.
- B. M. Atkeson and R. Forehand, “Parent Behavioural Training for Problem Children: An Examination of Studies Using Multiple Outcome Measures,” Abnormal Child Psychology, Vol. 6, No. 4, 1978, pp. 449-460.
- T. M. Achenbach, S. H. McConaughy and C. T. Howell, “Child/Adolescent Behavioural and Emotional Problems: Implications of Cross-Informant Correlations for Situational Specificity,” Psychological Bulletin, Vol. 101, No. 2, 1987, pp. 213-232. doi:10.1037/0033-2909.101.2.213
- G. R. Patterson, “Interventions for Boys with Conduct Problems: Multiple Settings, Treatments, and Criteria,” Journal of Consulting and Clinical Psychology, Vol. 42, No. 4, 1974, pp. 471-481. doi:10.1037/h0036731
- A. B. Irvine, A. Biglan, K. Smlkowski, C. W. Metzler and D.V. Ary, “The Effectiveness of a Parenting Skills Programme for Parents of Middle School Students in Small Communities,” Journal of Consulting and Clinical Psychology, Vol. 67, No. 6, 1999, pp. 811-825. doi:10.1037/0022-006X.67.6.811
- D. W. Murray, “Treatment of Preschoolers with AttentionDeficit/Hyperactivity Disorder,” Current Psychiatry Report, Vol. 12, No. 5, 2010, pp. 374-381. doi:10.1007/s11920-010-0142-6
- L. L. Greenhill, J. Puig-Antich, H. Novacenko, M. Solomon, C. Anghern, J. Florea, R. Goetz, B. Fiscina and E. J. Suchar, “Prolactin, Growth Hormone and Growth Responses in Boys with Attention Deficit Disorder and Hyperactivity Treated with Methylphenidate,” Journal of American Academy of Child and Adolescent Psychiatry, Vol. 23, No. 1,1984, pp. 58-67. doi:10.1097/00004583-198401000-00008
- S. Russell, R. Tannock, C. Charles and C. Penny, “Behavioural, Situational and Temporal Effects of Treatment of ADHD with Methylphenidate,” Journal of American Academy of Child and Adolescent Psychiatry, Vol. 36, No. 6, 1997, pp. 754-763. doi:10.1097/00004583-199706000-00011
- C. B. Carlson, W. E. Pelham, R. Milich and J. Dixon, “Single and Combined Effects of Methylphenidate and Behaviour Therapy on the Classroom performance of Children with Attention Deficit Hyperactivity Disorder,” Journal of Abnormal Child Psychology, Vol. 20, No. 2, 1992, pp. 213-232. doi:10.1007/BF00916549
- H. Weingartner, M. H. Ebert, E. J. Mikkelsen, J. L. Rapoport, M. S. Buchsbaum, E. E. Bunney and E. D. Caine, “Cognitive Processes in Normal And Hyperactive Children and Their Response to Amphetamine Treatment,” Journal of Abnormal Psychology, Vol. 89, No. 1, 1980, pp. 25-37. doi:10.1037/0021-843X.89.1.25
- J. M. Halperin, K. Matier, G. Bedi, S. Sharma and J. H. Newcorn, “Specificity of Inattention, Impulsivity and Hyperactivity to the Diagnosis of Attention Deficit Disorder,” Journal of American Academy of Child and Adolescent Psychiatry, Vol. 31, No. 2, 1992, pp. 190-196. doi:10.1097/00004583-199203000-00002
- A. D. Anastopoulos, T. L. Shelton, G. J. Dupaul and D. C. Guerremont, “Parent Training for Attention Deficit Hyperactivity Disorder: Its Impact on Parent Functioning,” Journal of Abnormal Child Psychology, Vol. 21, No. 5, 1993, pp. 581-596.doi:10.1007/BF00916320
- B. A. McBride, S. J. Shoppe and T. R. Rane, “Child Characteristics, Parenting Stress and Parental Involvement: Fathers vs. Mothers,” Journal of Marriage and Family, Vol. 64, No. 4, 2002, pp. 998-1011. doi:10.1111/j.1741-3737.2002.00998.x

