Case Reports in Clinical Medicine
Vol.3 No.3(2014), Article ID:43760,6 pages DOI:10.4236/crcm.2014.33039
Subcapsular Hepatic Hematoma after ERCP: A Case Report and Revision of Literature
Katerina Klímová*, Camilo Padilla Suárez, Cecilia González Asanza, Ana Matilla Peña, Enrique Cos Arregui, Ana Hernando Alonso
Department of Hepatogastroenterology and Endoscopy, Hospital General Universitario Gregorio Marañón, Madrid, Spain
Email: *katerina_klimova@yahoo.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 18 December 2013; revised 17 January 2014; accepted 16 February 2014
ABSTRACT
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive procedure for diagnosis and treatment of biliary and pancreatic diseases. Even in the best hands, complications may occur. Clinically significant hemorrhagic complications associated usually to previous papillotomy are uncommon. Subcapsular hepatic hematoma is excepcional, with only twenty cases described. We present a case of a 52-year-old man who developed a large subcapsular liver hematoma following a therapeutic ERCP. Due to serious anemization and hemodynamic instability, arterial embolization and finally urgent surgical evacuation of the hematoma were performed. In the postoperative period the patient presented infection of the collection, which indicated colocation of percutaneous drainage and broad-spectrum intravenous antibiotics, and gradually recovered.
Keywords:Subcapsular Hepatic Hematoma; Endoscopic Retrograde Cholangiopancreatography; Arterial Embolization; Percutaneous Drainage; Surgery

1. Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive procedure for diagnosis and treatment of biliary and pancreatic diseases. Even in the best hands, complications occur in 2% - 10% of cases [1] . Clinically significant hemorrhagic complications associated usually with previous papillotomy are uncommon, although endoscopically visible bleeding is quite frequent [2] .
On the other hand, subcapsular hepatic hematoma is exceptional, with fewer than twenty cases described worldwide since 2000, when the first case was published [3] .
In this report we describe a case of subcapsular hepatic hematoma following ERCP, analyze possible mechanisms of its production and present a revision of current literature.
2. Case Presentation
We present a case of a 52-year-old man with a past medical history of chronic pancreatitis requiring surgical necrosectomy who was admitted to our hospital due to a new exacerbation. Endoscopic ultrasonography demonstrated presence of lithiasis in the main pancreatic duct (Figure 1). Subsequently, ERCP with biliar sphincterotomy over a 0.035-inch diameter guidewire was performed, without difficulty. However, duodenal intubation was laborious due to repeated loop formation. Eventually, pancreatic tree canalization and pancreatic sphincterotomy were successfully realized. In spite of various attempts, it was impossible to extract the pancreatic stones.
Over the following six hours, the patient developed right-sided upper abdominal pain with no clear sign of abdominal tenderness. The hemoglobin level declined from 14 g/dL to 8 g/dL. An urgent abdominal computed tomography (CT) scan revealed subcapsular hematoma surrounding the whole right hepatic lobe, with dimensions of 19 × 17.8 × 6.9 cm (Figure 2). Due to new anemization, despite blood transfusions, and hemodynamic

Figure 1. Presence of two lithiasis in the main pancreatic duct (arrows) visualized by endoscopic ultrasonography.
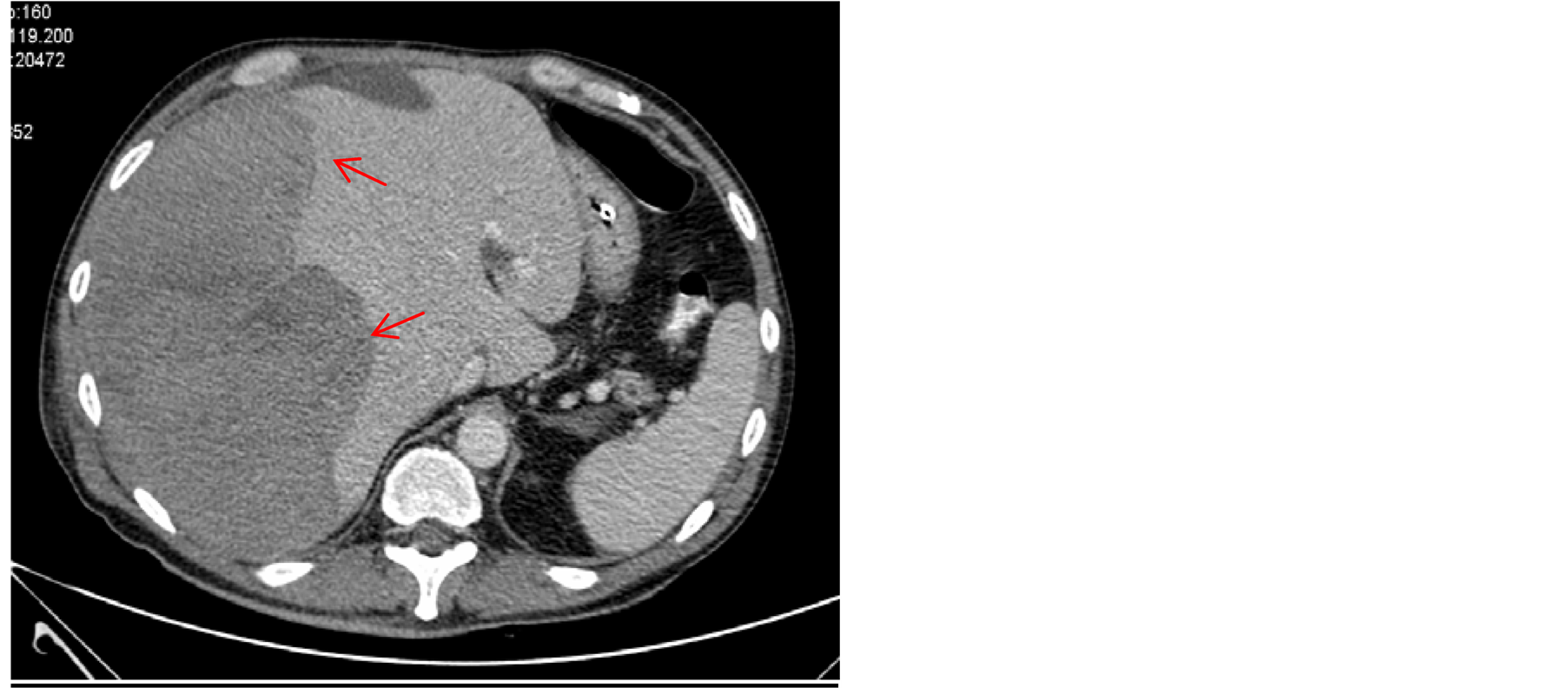
Figure 2. Abdominal CT scan reveals hepatic subcapsular hematoma with dimensions of 19 × 17.8 × 6.9 cm (red arrows).
instability, selective embolization of right hepatic artery was performed, without any clear radiological improvement. Owing to further clinical deterioration, urgent surgical evacuation of the hematoma had to be undertaken 72 hours after the ERCP. In the postoperative period the patient presented infection of the collection, which indicated colocation of percutaneous drainage (Figure 3), and broad-spectrum intravenous antibiotics were administered over a period of six weeks. The patient gradually recovered and complete resolution of hematoma was seen in control CT scan, it being thus possible to withdraw the drainage catheter (Figure 4). He was discharged two months after admission in good condition.
3. Discussion
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive proced ure for diagnosis and treatment of biliary and pancreatic diseases. Even in the best hands, complications may occur in 2% - 10% of the cases, pancreatitis, cholangitis, perforation, and bleeding from papillotomy being the most frequent ones [1] . The overall mortality rate after a diagnostic ERCP is approximately 0.5%, while death rates after therapeutic ERCP are twice as high, and may occur from any of the complications described previously [4] .
As a result, clinically significant hemorrhagic complications associated usually with previous papillotomy occur according to some series in 2% of all cases, although endoscopically visible bleeding is more frequent (between 10% and 30% of all papillotomies) [2] .
On the other hand, hemorrhage or hematoma associated with ERCP involving the liver, abdominal cavity, spleen and bowel wall are rare but potentially serious complications and should be recognized and treated rapidly [5] . Subcapsular hepatic hematoma is exceptional, with only twenty cases described worldwide (Table 1). It is a condition that can be life-threatening, although no death has been reported so far.

Figure 3. Colocation of percutaneous drainage guided by abdominal CT scan.
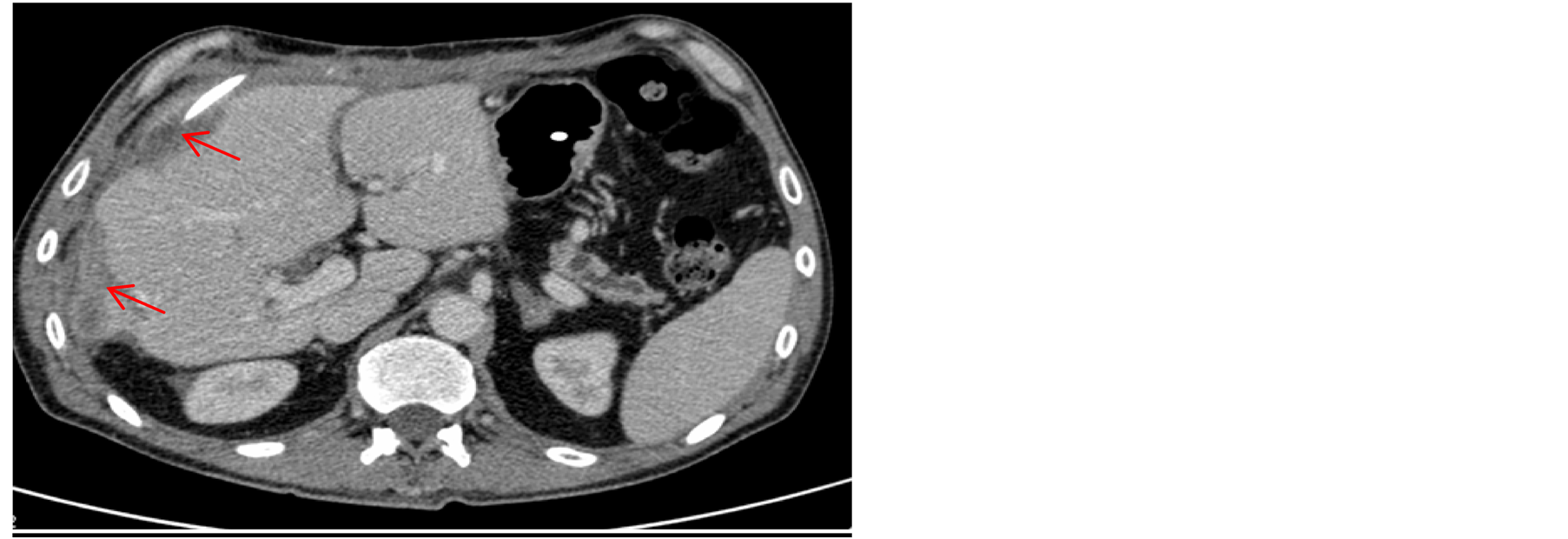
Figure 4. Resolution of voluminous hepatic hematoma observed on abdominal CT scan.
Table 1. Summary of cases of subcapsular hepatic hematoma after ERCP.
Abbreviations: Nr—number, M—male, F—female, NA—not available, hrs—hours, ATB—antibiotics, AT—arterial tension.
The etiology is not entirely clear. In most cases, however, hematoma occured as the result of a rupture of a small calibre intrahepatic vessel caused by a guide wire. This would also explain the presence of air inside the hematoma and frequent infections, as use of guide wire is not a sterile technique [6] . In one case, the hematoma was a consequence of a traction of the extracting balloon in order to withdraw it from the biliary tree [7] . After a careful analysis, we came to the conclusion, that in our case, the hematoma could also have developed due to loop formation in the duodenum, which may be related to his previous surgery, and its subsequent traction. A similar mechanism has already been proposed in cases of splenic hematomas after ERCP [5] .
As described by previous reports in the literature, the first symptom of most cases is abdominal pain, usually together with hypotension and fever. Thus, the presence of those should raise the suspicion of subcapsular hepatic hematoma [8] . However, according to some authors, the incidence of this complication might be underestimated, as many patients may not present any symptoms, and post-ERCP monitoring by imaging is not routinely done [9] .
Laboratory investigations are not helpful as major indicators of the development of subcapsular hepatic haematoma, except for low hematocrit. Imaging modalities (ultrasound, CT, and MRI) are the methods of choice for the diagnosis and control of this complication.
In most cases the management was conservative, as the hematoma can be contained by Glisson’s capsule. This should be the treatment of choice provided the patient remains hemodinamically stable [10] . However, based on the literature, we recommend that prophylactic antibiotics be administered, since there is a substantial risk of infection of the hematoma [11] , and in the majority of cases, patients were treated with antibiotics (Table 1).
Surgical treatment is reserved for patients with signs of hemodynamic instability or infection, or in cases of high risk of hematoma rupture or its growth [11] . It should consist of drainage of the hematoma, hemostasis if possible, and performing CT to monitor its evolution. Hepatic artery embolization [5] or percutaneous drainage [2] are valid alternatives to surgery. No long-term complications were described.
In the previously reported cases, three [7] [12] [13] were treated surgically and four [2] [8] [14] [15] were treated with percutaneous drainage.
In our case, the deterioration of general condition and hemodynamic instability forced us to indicate the surgical evacuation of the hematoma, since it was impossible to control the bleeding either by conservative treatment or by arterial embolization. Moreover, in spite of prophylactic antibiotics, the hematoma got infected, and percutaneous drainage had to be performed.
4. Conclusions
Subcapsular hepatic hematoma following ERCP is an infrequent complication, which, however, should be kept in mind in differential diagnosis of symptomatic cases after ERCP.
According to previous reports, it can appear as a result of manipulation with hydrophilic guide-wire and rupture of small intrahepatic vessels. In our patient with previous pancreatic surgery, we think it might have been a result of loop formation in the duodenum and its subsequent traction. The management is usually conservative. Treatment with embolization or surgery is usually reserved for more serious cases.
References
- Hart, R. and Classen, M. (1990) Complications of Diagnostic Gastrointestinal Endoscopy. Endoscopy, 22, 229-230. http://dx.doi.org/10.1055/s-2007-1010734
- Freeman, M.L., Neslon, D.B., Sherman, S., et al. (1996) Complications of Endoscopic Biliary Sphicterotomy. The New England Journal of Medicine, 335, 909-918. http://dx.doi.org/10.1056/NEJM199609263351301
- Ortega Deballon, P., Fernández Lobato, R., García Septern, J., Nieves Vázquez, M.A., Martínez Santos, C. and Moreno Azkoita, M. (2000) Liver Hematoma Following ERCP. Surgical Endoscopy, 14, 767.
- Loperfido, S., Angelini, G., Benedetti, G., et al. (1998) Major Early Complications from Diagnostic and Therapeutic ERCP: A Prospective Multicenter Study. Gastrointestinal Endoscopy, 48, 1-10. http://dx.doi.org/10.1016/S0016-5107(98)70121-X
- Wu, W.C. and Katon, R.M. (1993) Injury to the Liver and Spleen after Diagnostic ERCP. Gastrointestinal Endoscopy, 39, 824-827. http://dx.doi.org/10.1016/S0016-5107(93)70278-3
- Lynch, S.P. and Evans, J.A. (2010) Difficult Biliary Canulation. Current Gastroenterology Reports, 12, 135-140. http://dx.doi.org/10.1007/s11894-010-0089-0
- Baudet, J.-S., Arguiñarena, X., Redondo, I., Tadeo, E., Navazo, L., Mendiz, J. and Montiel, R. (2011) Subcapsular Hepatic Hematoma: An Uncommon Complication of Endoscopic Retrograde Cholangiopancreatography. Gastroenterología y Hepatología, 34, 79-82. http://dx.doi.org/10.1016/j.gastrohep.2010.11.002
- Fei, B.-Y. and Li, C.-H. (2013) Subcapsular Hepatic Haematoma after Endoscopic Retrograde CholangiopancreaTography: An Unusual Case. World Journal of Gastroenterology, 19, 1502-1504. http://dx.doi.org/10.3748/wjg.v19.i9.1502
- Horn, T.L. and Peña, L.R. (2004) Subcapsular Hepatic Hematoma after ERCP: Case Report and Review. Gastrointestinal Endoscopy, 59, 594-596. http://dx.doi.org/10.1016/S0016-5107(04)00013-6
- Cárdenas, A., Crespo, G. and Balderramo, D. (2008) Subcapsular Liver Hematoma after ERCP in a Liver Transplant Recipient. Annals of Hepatology, 7, 386-388.
- Del Pozo, D., Moral, I. and Poves, E. (2011) Subcapsular Hepatic Hematoma Following ERCP: Case Report and Review. Endoscopy, 43, UCTN: E164-E165.
- Priego, P., Rodríguez, G., Mena, A., Losa, N., et al. (2007) Subcapsular Liver Hematoma after ERCP. Revista Española de Enfermedades Digestivas, 99, 53-54. http://dx.doi.org/10.4321/S1130-01082007000100014
- Pérez-Legas, J., Santos, J., Ruiz-Tovar, J., Moya-Forcén, P., et al. (2011) Subcapsular Hepatic Hematoma after ERCP. Revista Española de Enfermedades Digestivas, 103, 550-551. http://dx.doi.org/10.4321/S1130-01082011001000011
- Petit-Laurent, F., Scalone, O., Penigaud, M. and Barbeys, J. (2007) Subcapsular Hepatic Hematoma after Endoscopic Retrograde Cholangiopancreatography: Case Report and Literature Review. Gastroentérologie Clinique et Biologique, 31, 750-752. http://dx.doi.org/10.1016/S0399-8320(07)91937-5
NOTES

*Corresponding author.


