Journal of Cancer Therapy
Vol.2 No.5(2011), Article ID:16615,4 pages DOI:10.4236/jct.2011.25092
Long Term Survival after Resection of a Small Bowel Metastasis of Lung Adenocarcinoma: A Case Report
![]()
1Department of Hepatic-Biliary and Digestive Surgery, CHU Rennes, France; 2Department of Pediatric Surgery, CHU Rennes, France.
E-mail: *laurent.sulpice@chu-rennes.fr
Received July 18th, 2011; revised August 15th, 2011; accepted August 29th, 2011.
Keywords: ileal metastasis, lung cancer metastasis, acute abdominal pain, lymph nodes excision
ABSTRACT
Background: Small bowel metastases of lung adenocarcinoma represent a rare clinical entity, often diagnosed after complications due to obstruction, bleeding or bowel perforation. Case Report: We report a case of ileal metastasis discovered during an intestinal perforation. The patient was a 47-year-old man hospitalized in emergency for acute abdominal pain, with right lower quadrant abdominal defense and a clinical history of left lower pulmonary lobectomy for lung adenocarcinoma 6 months before. Exploratory laparotomy for peritonitis revealed a single ileal tumor which was resected with lymph nodes excision. Pathology finding revealed that it was compatible with an ileal metastasis of his lung adenocarcinoma. Conclusions: The suspicion of a small bowel metastasis of lung carcinoma, although rare, must be taken in consideration and to carry out an extensive surgery, because only this will have an improvement on the survival of these patients. The purpose of this investigation is to add a new case report to the few that exist in order to provide a therapeutic approach to these exceptional cases.
1. Background
Broncho-pulmonary cancer represents a true problem in public health in all Western countries and is the leading cause of cancer related deaths [1]. The preferential extra pulmonary metastatic sites are lymph nodes, liver, brain and adrenal glands [2]. The digestive localisations are exceptional but they seem to be underestimated because they are rarely symptomatic, but it reach almost 11% on systematic autopsy of deceased patients of lung cancer [3,4]. In fact, they can affect the whole digestive tract responsible for a variety of symptoms: anaemia, dysphagia, obstruction and peritonitis due to digestive perforation, in this setting it has a significant impact on mortality, decreasing 1-year survival to less than 3 per cent.
2. Case Report
A 47 years old man hospitalized in emergency for pain and muscular defense in the right iliac pit. Previously, he had a resection of a colon polyp that occurred three years before and an extended left lower pulmonary lobectomy for a lung adenocarcinoma that occurred about six months before (pT2N0M0), no tobacco smoke exposure after surgery.
His clinical history begins 24 hours before hospitalisation with the appearance of abdominal pain in the right lower quadrant that radiates in hypogastric in an oscillating feverish context between 38˚ and 38.5˚. In front of the fast increase of the pains and the appearance of an occlusive syndrome with uncontrollable vomiting, patient is therefore directed to a surgical emergency. The patient reveals the presence of colorectal bleeding for about 1 month. The initial clinical examination shows a 39˚ fever associated with an abdominal generalized defense and a complete disappearance of peristaltic sounds. Blood tests show a marked inflammatory syndrome with values of C-reactive protein to 125 (Nle < 5) associated with hyper leukocytosis (14,000). The remainder of the biological assessment is without characteristic in particular no anemia. Thoracic radiography as well as the radiography of abdomen without preparation is within the limits of normal. Clinical is evocative of appendicitis complicated by local peritonitis, but the antecedents of the patient carry to make an abdomino-pelvic CT scan. The CT scan do not find bowel obstruction, or liquid or air diffuse effusion, but finds a ileal handle with mural thickening and hyperdence in arterial phase associated to a mesenteric infiltration and local extra bowel air (Figures 1 and 2).
A subombilical median laparotomy was made; it allowed
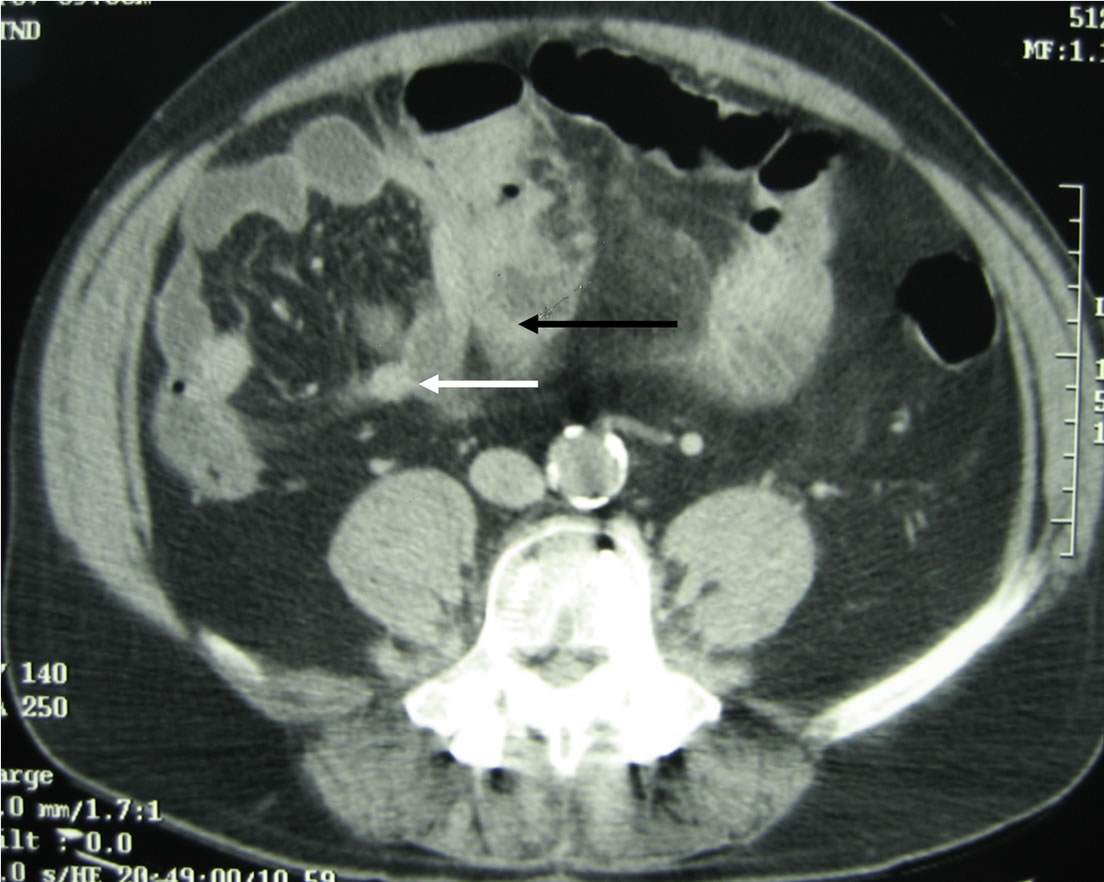
Figure 1. Abdominal CT-scan. Black arrow: ileal metastasis; White arrow: hypervascularised mesenteric lymph node.
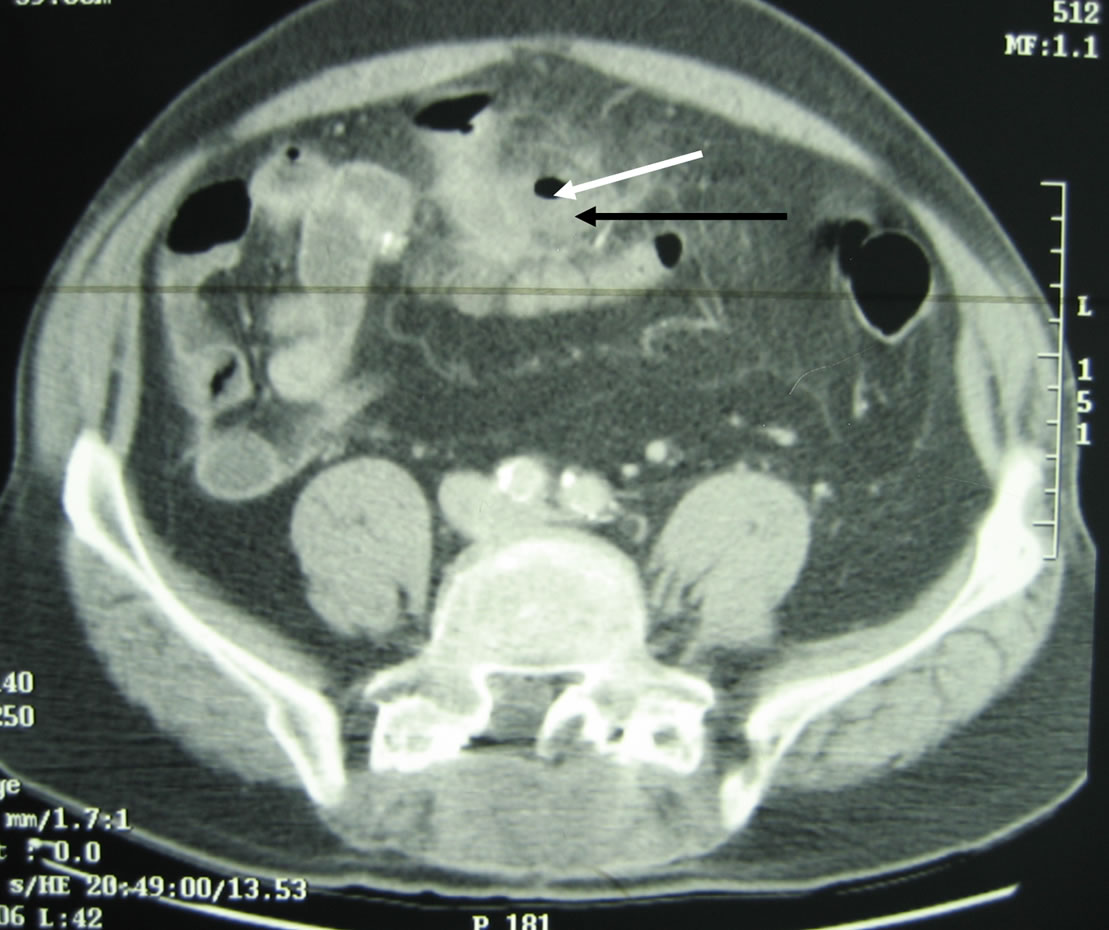
Figure 2. Abdominal CT-scan. Black arrow: mesenteric abscess; White arrow: extra digestive air trapped.
finding an abscess, localized between 2 small bowel handles and the greater omentum. It was a purulent collection (50 cc) associated with a small bowel neoplasm (4 × 3 cm) perforated on the anti-mesenteric edge and localized approximately to 30 cm to Bauhin valve. Many mesenteric lymph nodes have been found around this lesion.
A short ileal resection (18 cm) associated to lymph node, and greater omentum excision was made in only one bloc. An end-to-end, ileo-ileal manual anastomosis was realized to the re-establishment of digestive continuity, followed with a triple probabilistic antibiotic therapy (cephalosporine, gentamicin and metronidazole).
Pathological examination finds: a stenosing and perforated adenocarcinoma cancer pT3N0Mx (N 0/12). Immuno-histochemical complement finds: polyclonal antiACE antibody (+); Anti-CD138 antibody (–); anti CD3 antibody (+); anti-Beta HCG antibody (positive 1/5); Anti-CK7 antibody (++); anti-CK20 antibody (–). The same result was found at the pathological examination of the left lower pulmonary lobectomy six months before concluding to a perforation of small bowel metastasis from the previous lung adenocarcinoma.
No complication in the postoperative period was found. Chemotherapy with Cisplatine and Navelbine was initiated after surgery (4 cycles).
One month after surgery, the thoraco-abdominal CT scan and PET scan, were normal without any new metastatic localization. At 3-year follow-up, was still alive without disease recurrence objectivated by CT-scan and PET-scan.
3. Discussion
Small bowel metastases of lung carcinoma are rare but must be known and suspected in all patients with small bowel neoplasm, in particular in this patient which an history of lung cancer but also in front of history to tobacco smoke exposure [5,6].
It’s not rare that small bowel metastasis reveal the primitive cancer [7,8], but their existence is underestimated because rarely symptomatic [3]. MacNeill and all describes a series of 431 patients deceased for a lung cancer between 1974 and 1984. All the patients have been subordinates to autopsy. In 46 cases a small bowel metastasis were found (10.6%) [4]. In the same way Stenbygaard in 1999 describes 10 small bowel metastases on 218 autopsies for lung cancer (4.6%) [9].
This important incidence demands to seek metastasis in front of an abdominal symptomatology, especially in patients with bronco-pulmonary cancer. Metastasis can be characterised by abdominal pains, anaemia for digestive bleeding or small bowel obstruction or peritonitis for small bowel perforation [8]. These last ones rebel spontaneously as in our observation, or more frequently during chemotherapy after primary surgery.
In the rare cases described in the literature of small bowel perforations on small bowel lung metastases, the prognosis is difficult [2]. There is not case of survival 1 year after surgery. The recommendations of the authors are to practise a minimal surgery [2,6].
In our observation, we made a small bowel resection associated with extend lymph node excision, because we didn’t have pathology intra-operative diagnosis, so our patient is still alive at 3 years follow-up, with CT and PET scan normal.
This case must encourage practicing broad resection in small bowel neoplasm, even in the event of perforations and even in the doubt of a metastasis of lung cancer.
In conclusion: any small bowel tumor must make to think as a lung cancer metastasis; in particular in patient with history to tobacco smoke exposure, even if their incidence is lowland, because rarely symptomatic. If there is not other known metastatic localizations, a broad resection must be proposed with lymph nodes excision.
REFERENCES
- C. F. Mountain, S. D. Greenberg and A. E. Fraire, “Tumor Stage in Non-Small Cell Carcinoma of the Lung,” Chest, Vol. 99, No. 5, 1991, pp. 1258-1260. doi:10.1378/chest.99.5.1258
- A. Sternberg, S. Giler, I. Segal, Z. Shmuter and I. Kott, “Small Bowel Perforation as the Presenting Symptom of Squamous Cell Carcinoma of the Lung,” Journal of Clinical Oncology, Vol. 6, No. 2, 1980, pp. 181-186.
- A. S. Antler, Y. Ough, C. S. Pitchumoni, M. Davidian and W. Thelmo, “Gastrointestinal Metastases from Malignant Tumors of the Lung,” Cancer, Vol. 49, No. 1, 1982, pp. 170-172. doi:10.1002/1097-0142(19820101)49:1<170::AID-CNCR2820490134>3.0.CO;2-A
- P. M. McNeill, L. D. Wagman and J. P. Neifeld, “Small Bowel Metastases from Primary Carcinoma of the Lung,” Cancer, Vol. 59, No. 8, 1987, pp. 1486-1499. doi:10.1002/1097-0142(19870415)59:8<1486::AID-CNCR2820590815>3.0.CO;2-W
- J. M. Woods and M. J. Koretz, “Emergency Abdominal Surgery for Complications of Metastatic Lung Carcinoma,” Archives of Surgery, Vol. 125, No. 5, 1990, pp. 583- 585. doi:10.1001/archsurg.1990.01410170029005
- D. M. Mosier, R. S. Bloch, P. L. Cunningham and S. A. Dorman, “Small Bowel Metastases from Primary Lung Carcinoma: A Rarity Waiting to be Found?” American Journal of Surgery, Vol, 58, No. 11, 1992, pp. 677-682.
- P. A. Renault, R. Arotcarena, V. Cales, A. Lippa, M. Benichou, P. Laurent, et al., “Metastatic Obstruction of the Small Bowel Revealing or Complicating SquamousCell Lung Cancer. Two Cases and a Review of the Literature,” Revue De Pneumologie Clinique, Vol. 59, No. 3, 2003, pp. 161-165.
- A. Berger, C. Cellier, C. Daniel, C. Kron, M. Riquet, J. P. Barbier, et al., “Small Bowel Metastases from Primary Carcinoma of the Lung: Clinical Findings and Outcome,” American Journal of Gastroenterology, Vol. 94, No. 7, 1999, pp. 1884-1887. doi:10.1111/j.1572-0241.1999.01224.x
- L. E. Stenbygaard and J. B. Sorensen, “Small Bowel Metastases in Non-Small Cell Lung Cancer,” Lung Cancer, 1999, Vol. 26, No. 2, 1999, pp. 95-101.

